Abstract
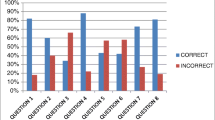
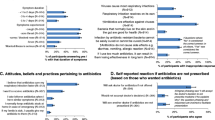
Background Inappropriate use of antibiotic treatment for pharyngitis by community pharmacists is prevalent in developing countries. Little is known about how the pharmacists identify patients with bacterial pharyngitis. Objective To ascertain the appropriateness of diagnosis of streptococcal pharyngitis among Thai community pharmacists according to the Centor criteria and to identify factors related to antibiotic dispensing. Setting 1040 Thai community pharmacists. Method A cross-sectional survey of community pharmacists was conducted in November 2012 to March 2013. The self-administered questionnaires were mailed to 57 % of community pharmacists in the south of Thailand (n = 1040). The survey included questions on diagnosis of streptococcal pharyngitis, knowledge on pharyngitis, and attitudes and control beliefs regarding antibiotic dispensing. Main outcome measure The appropriateness of diagnosis of streptococcal pharyngitis according to the original and modified Centor criteria and determinants of antibiotic dispensing including demographic characteristics of pharmacists, knowledge on pharyngitis, and attitudes and control beliefs on antibiotic dispensing. Results Approximately 68 % completed the questionnaires (n = 703). Compared to the pharmacists who reported not dispensing antibiotics in the hypothetical case with common cold, those reported dispensing antibiotics were more likely to consider the following conditions—presence of cough, mild sore throat and patients with age >60 years as cues for diagnosis of streptococcal pharyngitis (p < 0.05). The use of fewer scores of the clinical prediction rules for diagnosis was observed in antibiotic dispensers, compared to who did not do so (p < 0.005). Antibiotic dispensing was positively associated with period of dispensing experience (>5 years) [odds ratio (OR) 1.52; 95 % confidence interval (CI) 1.03–2.23], belief that antibiotics could shorten duration of pharyngitis (OR 1.48; 95 % CI 1.11–1.99), belief that antibiotics could prevent the complications (OR 1.44; 95 % CI 1.09–1.91) and belief that dispensing antibiotics could satisfy the patients (OR 1.31; 95 % CI 1.01–1.71). Nonetheless, antibiotic dispensing was negatively associated with knowledge about pharyngitis (OR 0.83; 95 % CI 0.75–0.93). Conclusion Pharmacists who are knowledgeable on the Centor criteria are more likely to appropriately diagnose streptococcal pharyngitis and less likely to dispense antibiotics in such case.
Similar content being viewed by others
References
Anjos LM, Marcondes MB, Lima MF, Mondelli AL, Okoshi MP. Streptococcal acute pharyngitis. Rev Soc Bras Med Trop. 2014;47(4):409–13.
Wessels MR. Streptococcal pharyngitis. N Engl J Med. 2011;364(7):648–55.
Herath V, Carapetis J. Sore throat: is it such a big deal anymore? J Infect. 2015;71(Suppl 1):S101–5.
Van Brusselen D, Vlieghe E, Schelstraete P, De Meulder F, Vandeputte C, Garmyn K, et al. Streptococcal pharyngitis in children: to treat or not to treat? Eur J Pediatr. 2014;173(10):1275–83.
Cohen JF, Cohen R, Levy C, Thollot F, Benani M, Bidet P, et al. Selective testing strategies for diagnosing group A streptococcal infection in children with pharyngitis: a systematic review and prospective multicentre external validation study. CMAJ. 2015;187(1):23–32.
Alper Z, Uncu Y, Akalin H, Ercan I, Sinirtas M, Bilgel NG. Diagnosis of acute tonsillopharyngitis in primary care: a new approach for low-resource settings. J Chemother. 2013;25(3):148–55.
Weber R. Pharyngitis. Prim Care Clin Office Pract. 2014;41(1):91–8.
Hildreth AF, Takhar S. Evidence-based evaluation and management of patients with pharyngitis in the emergency department. Emerg Med Pract. 2015;17(9):1–20.
Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making. 1981;1(3):239–46.
Chiappini E, Regoli M, Bonsignori F, Sollai S, Parretti A, Galli L, et al. Analysis of different recommendations from international guidelines for the management of acute pharyngitis in adults and children. Clin Ther. 2011;33(1):48–58.
Mclsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE. Empirical validation of guidelines for the management of pharyngitis in children and adults. JAMA. 2004;291(13):1587–95.
World Health Organization. Antimicrobial resistance; 2015. http://www.who.int/mediacentre/factsheets/antibiotic-resistance/en/. Accessed 3 Aug 2016.
National Antimicrobial Resistance Surveillance Center, Thailand. Antibiogram; 2015. http://narst.dmsc.moph.go.th. Accessed 3 Aug 2016.
Almaaytah A, Mukattash TL, Hajaj J. Dispensing of non-prescribed antibiotics in Jordan. Patient Prefer Adherence. 2015;9:1389–95.
Bin Abdulhak AA, Al Tannir MA, Almansor MA, Almohaya MS, Onazi AS, Marei MA, et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: a cross sectional study. BMC Public Health. 2011;11:538.
Morgan DJ, Okeke IN, Laxminarayan R, Perencevich EN, Weisenberg S. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. 2011;11(9):692–701.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60.
Vazquez-Lago JM, Lopez-Vazquez P, López-Durán A, Taracido-Trunk M, Figueiras A. Attitudes of primary care physicians to the prescribing of antibiotics and antimicrobial resistance: a qualitative study from Spain. Fam Pract. 2012;29(3):352–60.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211.
National Institute for Health and Clinical Excellence (NICE). Prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care (clinical guideline 69); 2008. http://www.nice.org.uk. Accessed 3 Aug 2016.
Snow V, Mottur-Pilson C, Cooper RJ, Hoffman JR. Principles of appropriate antibiotic use for acute pharyngitis in adults. Ann Intern Med. 2001;134(6):506–8.
Regoli M, Chiappini E, Bonsignori F, Galli L, de Martino M. Update on the management of acute pharyngitis in children. Ital J Pediatr. 2011;37:10.
Roggen I, van Berlaer G, Gordts F, Pierard D, Hubloue I. Acute sore throat in children at the emergency department: best medical practice? Eur J Emerg Med. 2015;22(5):343–7.
Botica MV, Botica I, Stamenić V, Andrasević AT, Kern J, Spehar SS. Antibiotic prescription rate for upper respiratory tract infections and risks for unnecessary prescription in Croatia. Coll Antropol. 2013;37(2):449–54.
Chlabicz S, Pytel-Krolczuk B, Ołtarzewska AM, Marcinowicz L. Management of sore throat in Polish primary care facilities: an example from the country with rare use of microbiological testing. J Clin Pharm Ther. 2008;33(2):153–7.
Palla AH, Khan RA, Gilani AH, Marra F. Over prescription of antibiotics for adult pharyngitis is prevalent in developing countries but can be reduced using Mclsaac modification of Centor scores: a cross-sectional study. BMC Pulm Med. 2012;12:70.
Nga DT, Chuc NT, Hoa NP, Hoa NQ, Nguyen NT, Loan HT, et al. Antibiotic sales in rural and urban pharmacies in northern Vietnam: an observational study. BMC Pharmacol Toxicol. 2014;15:6.
Zapata-Cachafeiro M, González-González C, Váquez-Lago JM, Lopez-Vazquez P, Lopez-Duran A, Smyth E, et al. Determinants of antibiotic dispensing without a medical prescription: a cross-sectional study in the north of Spain. J Antimicrob Chemother. 2014;69(11):3156–60.
Urkin J, Allenbogen M, Friger M, Vinker S, Reuveni H, Elahayani A. Acute pharyngitis: low adherence to guidelines highlights need for greater flexibility in managing paediatric cases. Acta Paediatr. 2013;102(11):1075–80.
Saengcharoen W, Chongsuvivatwong V, Lerkiatbundit S, Wongpoowarak P. Factors influencing dispensing of antibiotics for upper respiratory infections among Southern Thai community pharmacists. J Clin Pharm Ther. 2008;33(2):123–9.
Zgierska A, Rabago D, Miller MM. Impact of patient satisfaction ratings on physicians and clinical care. Patient Prefer Adherence. 2014;8:437–46.
Branche AR, Walsh EE, Jadhav N, Karmally R, Baran A, Peterson DR, et al. Provider decisions to treat respiratory illnesses with antibiotics: insights from a randomized controlled trial. PLoS ONE. 2016;11(4):e0152986.
Dekker AR, Verheij TJ, van der Velden AW. Inappropriate antibiotic prescription for respiratory tract indications: most prominent in adult patients. Fam Pract. 2015;32(4):401–7.
Ecker L, Ochoa TJ, Vargas M, Del Valle LJ, Ruiz J. Factors affecting caregivers’ use of antibiotics available without a prescription in Peru. Pediatrics. 2013;131(6):e1771–9.
Mustafa M, Wood F, Butler CC, Elwyn G. Managing expectations of antibiotics for upper respiratory tract infections: a qualitative study. Ann Fam Med. 2014;12(1):29–36.
Rodrigues AT, Roque F, Falcão A, Figueiras A, Herdeiro MT. Understanding physician antibiotic prescribing behaviour: a systematic review of qualitative studies. Int J Antimicrob Agents. 2013;41(3):203–12.
Cadieux G, Abrahamowicz M, Dauphinee D, Tamblyn R. Are physicians with better clinical skills on licensing examinations less likely to prescribe antibiotics for viral respiratory infections in ambulatory care settings? Med Care. 2011;49(2):156–65.
Mousquès J, Renaud T, Scemama O. Is the “practice style” hypothesis relevant for general practitioners? An analysis of antibiotics prescription for acute rhinopharyngitis. Soc Sci Med. 2010;70(8):1176–84.
Kotwani A, Wattal C, Joshi PC, Holloway K. Irrational use of antibiotics and role of the pharmacist: an insight from a qualitative study in New Delhi, India. J Clin Pharm Ther. 2012;37(3):308–12.
Acknowledgments
We gratefully acknowledge all community pharmacists who participated in this study. We wish to thank the lecturers and graduate students of the Faculty for their assistance in questionnaire development. Finally, we thank Dr. Alan Geater for English editing.
Funding
This work was supported by Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Songkhla, Thailand (PSU.598/W.812).
Conflicts of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saengcharoen, W., Jaisawang, P., Udomcharoensab, P. et al. Appropriateness of diagnosis of streptococcal pharyngitis among Thai community pharmacists according to the Centor criteria. Int J Clin Pharm 38, 1318–1325 (2016). https://doi.org/10.1007/s11096-016-0373-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0373-7