Abstract
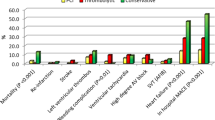
Background Little is known about predictors and outcome differences of primary percutaneous coronary intervention (PPCI) and thrombolytic therapy (TT) in ST-segment elevation myocardial infarction (STEMI) patients in the Middle East. Objective To compare predictors as well as in-hospital outcomes of PPCI and TT in STEMI patients in six Middle Eastern countries. Setting Sixty-five hospitals (covering at least 85 % of the population) in Oman, United Arab Emirates, Qatar, Bahrain, Kuwait and Yemen. Methods This was a prospective, multinational, multicentre, observational survey of consecutive acute coronary syndrome patients who were admitted to 65 hospitals during May 8, 2006 to June 6, 2006 and from January 29, 2007 to June 29, 2007, as part of Gulf RACE (Registry of Acute Coronary Events). Analyses were performed using univariate and multivariate statistical techniques. Main outcome measures Predictors as well as in-hospital outcomes of PPCI and TT in STEMI patients. Results Out of 2,155 STEMI patients admitted to hospitals within 12 h of symptoms onset, 92 % received reperfusion (8 % PPCI and 84 % TT). TT use included reteplase (43 %), tenecteplase (30 %), streptokinase (25 %), and alteplase (2 %). Median age of the study cohort was 50 (44–58) years with majority being males (90 %). There were no significant differences in median onset time to presentation between the TT and PPCI groups (130 vs. 120 min; P = 0.422). Median door-to-needle time and door-to-balloon time were 45 min (29–75) and 75 min (58–120), respectively. Predictors of PPCI included prior PCI, hospitals with catheterization laboratory facilities as well as those involved with academia. Multivariate logistic regression model demonstrated that patients that had PPCI were less likely to have recurrent ischemic attacks than those that had TT (odds ratio, 0.18; 95 % CI, 0.06–0.56; P = 0.003). Conclusions The main reperfusion strategy for STEMI patients in the Arab Middle East region is thrombolytic therapy. Predictors of primary percutaneous coronary intervention included prior percutaneous coronary intervention, hospitals with catheterization laboratory facilities as well as those involved with academia. Primary percutaneous coronary intervention resulted in significant reductions in recurrent ischemic events when compared to thrombolytic therapy.
Similar content being viewed by others
References
Media centre, World Health Organization. Cardiovascular diseases (CVDs). [Internet] 2011 [cited 2011 Mar 2]. Available from: http://www.who.int/mediacentre/factsheets/fs317/en/index.html/.
Ramahi TM. Cardiovascular disease in the Asia Middle East region: global trends and local implications. Asia Pac J Public Health. 2010;22(3 Suppl):83S–9S.
Kushner FG, Hand M, Smith SC Jr, King SB III, Anderson JL, Antman EM, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54(23):2205–41.
Keely E, Boura J, Grines C. Primary angioplasty versus with intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of of 23 randomised trials. Lancet. 2003;361(9351):13–20.
Ziljstra F, Hoorntje JC, de Boer MJ, Reiffers S, Miedema K, Ottervanger JP, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 1999;341(19):1413–9.
The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTOIIb) Angioplasty Substudy Investigators. A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. N Engl J Med. 1997;336(23):1621–28.
Weaver WD, Simes RJ, Betriu A, Grines CL, Zijlstra F, Garcia E, et al. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA. 1997;278(23):2093–8.
Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O’keefe J, et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993;328(10):673–9.
Every NR, Parsons LS, Hlatky M, Martin JS, Weaver WD. A comparison of thrombolytic therapy with primary coronary angioplasty for acute myocardial infarction. N Engl J Med. 1996;335(17):1253–60.
Tiefenbrunn AJ, Chandra NC, French WJ, Gore JM, Rogers WJ. Clinical experience with primary percutaneous transluminal coronary angioplasty compared with alteplase (recombinant tissue-type plasminogen activator) in patients with acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2). J Am Coll Cardiol. 1998;31(6):1240–5.
Danchin N, Vaur L, Genes N, Etienne S, Angioi M, Ferrieres J, et al. Treatment of acute myocardial infarction by primary coronary angioplasty or intravenous thrombolysis in the “real world”: one-year results from a nationwide French survey. Circulation. 1999;99(20):2639–44.
Zubaid M, Rashed WA, Al-Khaja N, Almahmeed W, Al-Lawati J, Sulaiman K, et al. Clinical presentation and outcomes of acute coronary syndromes in the gulf registry of acute coronary events (Gulf RACE). Saudi Med J. 2008;29(2):251–5.
Cannon CP, Battler A, Brindis RG, Cox JL, Ellis SG, Every NR, et al. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee). J Am Coll Cardiol. 2001;38(7):2114–30.
Lemeshow S, Hosmer DWJ. A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. 1982;115(1):92–106.
Stenestrand U, Lindbäck J. RIKS-HIA Registry. Long-term outcome of primary percutaneous coronary intervention vs prehospital and in-hospital thrombolysis for patients with ST-elevation myocardial infarction. JAMA. 2006;296(14):1749–56.
NCDR-ACTION registry-GWTG Results. [Internet] 2010 [cited 2011 Mar 4]. Available from: http://www.cardiosource.org/…/NCDR/…/ACTIONGWTG%20ResultsQ309_Q210.ashx/.
Birkhead JS, Weston C, Lowe D. Impact of specialty of admitting physician and type of hospital on care and outcome for myocardial infarction in England and Wales during 2004–5: observational study. BMJ. 2006;332(7553):1306–11.
Casale SN, Auster CJ, Wolf F, Pei Y, Devereux RB. Ethnicity and socioeconomic status influence use of primary angioplasty in patients presenting with acute myocardial infarction. Am Heart J. 2007;154(5):989–93.
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004;44(3):E1–211.
Al-Mallah MH, Alsheikh-Ali AA, Almahmeed W, Sulaiman K, Al Suwaidi J, Ridha M, et al. Missed opportunities in the management of ST-segment elevation myocardial infarction in the Arab Middle East: patient and physician impediments. Clin Cardiol. 2010;33(9):565–71.
Acknowledgments
The authors would like to thank the patients, physicians, nurses, and support staff participating in the Gulf RACE registry for their invaluable cooperation.
Funding
We disclose the receipt of a grant for this Gulf RACE project from Gulf Heart Association with finances supported by Sanofi Aventis and Qatar Telecommunications Company.
Conflicts of interest
The authors declare no conflicts of interest with respect to the authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Zakwani, I., Zubaid, M., Al-Riyami, A. et al. Primary coronary intervention versus thrombolytic therapy in myocardial infarction patients in the Middle East. Int J Clin Pharm 34, 445–451 (2012). https://doi.org/10.1007/s11096-012-9627-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9627-1