Abstract
Objective
Oral administration of insulin is a potential candidate for managing diabetes. However, it is obstructed by the gastrointestinal tract barriers resulting in negligible oral bioavailability.
Methods
This investigation presents a novel nanocarrier platform designed to address these challenges. In this regard, the process involved amination of sodium alginate by ethylene diamine, followed by its conjugation with deoxycholic acid.
Results
The resulting DCA@Alg@INS nanocarrier revealed a significantly high insulin loading content of 63.6 ± 1.03% and encapsulation efficiency of 87.6 ± 3.84%, with a particle size of 206 nm and zeta potentials of -3 mV. In vitro studies showed sustained and pH-dependent release profiles of insulin from nanoparticles. In vitro cellular studies, confocal laser scanning microscopy and flow cytometry analysis confirmed the successful attachment and internalization of DCA@Alg@INS nanoparticles in Caco-2 cells. Furthermore, the DCA@Alg@INS demonstrated a superior capacity for cellular uptake and permeability coefficient relative to the insulin solution, exhibiting sixfold and 4.94-fold enhancement, respectively. According to the uptake mechanism studies, the results indicated that DCA@Alg@INS was mostly transported through an energy-dependent active pathway since the uptake of DCA@Alg@INS by cells was significantly reduced in the presence of NaN3 by ~ 92% and at a low temperature of 4°C by ~ 94%.
Conclusions
Given the significance of administering insulin through oral route, deoxycholic acid-modified alginate nanoparticles present a viable option to surmount various obstacles presented by the gastrointestinal.









Similar content being viewed by others
Data Availability
The authors declare that the data supporting the findings of this study are available within the paper and its Supplementary Information files. Should any raw data files be needed in another format they are available from the corresponding author upon reasonable request. Source data are provided in this paper.
References
Qidwai W, Ashfaq T. Imminent epidemic of diabetes mellitus in Pakistan: issues and challenges for health care providers. 2010.
Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL-D, Sacre JW, Karuranga S, et al. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Research and Clinical Practice. 2022;183:109118. https://doi.org/10.1016/j.diabres.2021.109118.
Wang A, Fan W, Yang T, He S, Yang Y, Yu M, et al. Liver-Target and Glucose-Responsive Polymersomes toward Mimicking Endogenous Insulin Secretion with Improved Hepatic Glucose Utilization. Adv Func Mater. 2020;30(13):1910168. https://doi.org/10.1002/adfm.201910168.
Li S, Liang N, Yan P, Kawashima Y, Sun S. Inclusion complex based on N-acetyl-L-cysteine and arginine modified hydroxypropyl-β-cyclodextrin for oral insulin delivery. Carbohyd Polym. 2021;252:117202. https://doi.org/10.1016/j.carbpol.2020.117202.
Martins JP, D’Auria R, Liu D, Fontana F, Ferreira MP, Correia A, et al. Engineered Multifunctional Albumin-Decorated Porous Silicon Nanoparticles for FcRn Translocation of Insulin. Small. 2018;14(27):1800462. https://doi.org/10.1002/smll.201800462.
Huang Y-Y, Wang C-H. Pulmonary delivery of insulin by liposomal carriers. J Control Release. 2006;113(1):9–14. https://doi.org/10.1016/j.jconrel.2006.03.014.
Deutel B, Laffleur F, Palmberger T, Saxer A, Thaler M, Bernkop-Schnürch A. In vitro characterization of insulin containing thiomeric microparticles as nasal drug delivery system. Eur J Pharm Sci. 2016;81:157–61. https://doi.org/10.1016/j.ejps.2015.10.022.
Kim S, Yang H, Eum J, Ma Y, Lahiji SF, Jung H. Implantable powder-carrying microneedles for transdermal delivery of high-dose insulin with enhanced activity. Biomaterials. 2020;232:119733. https://doi.org/10.1016/j.biomaterials.2019.119733.
Shi Y, Xue J, Sang Y, Xu X, Shang Q. Insulin-loaded hydroxypropyl methyl cellulose-co-polyacrylamide-co-methacrylic acid hydrogels used as rectal suppositories to regulate the blood glucose of diabetic rats. Int J Biol Macromol. 2019;121:1346–53. https://doi.org/10.1016/j.ijbiomac.2018.09.044.
Banerjee A, Ibsen K, Brown T, Chen R, Agatemor C, Mitragotri S. Ionic liquids for oral insulin delivery. Proc Natl Acad Sci. 2018;115(28):7296–301. https://doi.org/10.1073/pnas.1722338115.
Pridgen EM, Alexis F, Farokhzad OC. Polymeric nanoparticle drug delivery technologies for oral delivery applications. Expert Opin Drug Deliv. 2015;12(9):1459–73. https://doi.org/10.1517/17425247.2015.1018175.
Liu H, Tang R, Pan WS, Zhang Y, Liu H. Potential utility of various protease inhibitors for improving the intestinal absorption of insulin in rats. J Pharm Pharmacol. 2003;55(11):1523–9. https://doi.org/10.1211/0022357022052.
Banerjee A, Mitragotri S. Intestinal patch systems for oral drug delivery. Curr Opin Pharmacol. 2017;36:58–65. https://doi.org/10.1016/j.coph.2017.08.005.
Maher S, Mrsny RJ, Brayden DJ. Intestinal permeation enhancers for oral peptide delivery. Adv Drug Deliv Rev. 2016;106:277–319. https://doi.org/10.1016/j.addr.2016.06.005.
Davies M, Pieber TR, Hartoft-Nielsen M-L, Hansen OK, Jabbour S, Rosenstock J. Effect of oral semaglutide compared with placebo and subcutaneous semaglutide on glycemic control in patients with type 2 diabetes: a randomized clinical trial. JAMA. 2017;318(15):1460–70. https://doi.org/10.1001/jama.2017.14752.
Cheng H, Zhang X, Qin L, Huo Y, Cui Z, Liu C, et al. Design of self-polymerized insulin loaded poly (n-butylcyanoacrylate) nanoparticles for tunable oral delivery. J Control Release. 2020;321:641–53. https://doi.org/10.1016/j.jconrel.2020.02.034.
Zhou X, Wu H, Long R, Wang S, Huang H, Xia Y, et al. Oral delivery of insulin with intelligent glucose-responsive switch for blood glucose regulation. Journal of Nanobiotechnology. 2020;18:1–16. https://doi.org/10.1186/s12951-020-00652-z.
Zhang T, Tang JZ, Fei X, Li Y, Song Y, Qian Z, et al. Can nanoparticles and nano-protein interactions bring a bright future for insulin delivery? Acta Pharmaceutica Sinica B. 2021;11(3):651–67. https://doi.org/10.1016/j.apsb.2020.08.016.
Wu J, Zheng Y, Liu M, Shan W, Zhang Z, Huang Y. Biomimetic viruslike and charge reversible nanoparticles to sequentially overcome mucus and epithelial barriers for oral insulin delivery. ACS Appl Mater Interfaces. 2018;10(12):9916–28. https://doi.org/10.1021/acsami.7b16524.
Crater JS, Carrier RL. Barrier properties of gastrointestinal mucus to nanoparticle transport. Macromol Biosci. 2010;10(12):1473–83. https://doi.org/10.1002/mabi.201000137.
Round AN, Rigby NM, Garcia de la Torre A, Macierzanka A, Mills EC, Mackie AR. Lamellar structures of MUC2-rich mucin: a potential role in governing the barrier and lubricating functions of intestinal mucus. Biomacromolecules. 2012;13(10):3253–61. https://doi.org/10.1021/bm301024x.
Zhang Y, Xiong M, Ni X, Wang J, Rong H, Su Y, et al. Virus-mimicking mesoporous silica nanoparticles with an electrically neutral and hydrophilic surface to improve the oral absorption of insulin by breaking through dual barriers of the mucus layer and the intestinal epithelium. ACS Appl Mater Interfaces. 2021;13(15):18077–88. https://doi.org/10.1021/acsami.1c00580.
Han X, Lu Y, Xie J, Zhang E, Zhu H, Du H, et al. Zwitterionic micelles efficiently deliver oral insulin without opening tight junctions. Nat Nanotechnol. 2020;15(7):605–14. https://doi.org/10.1038/s41565-020-0693-6.
Fan W, Xia D, Zhu Q, Li X, He S, Zhu C, et al. Functional nanoparticles exploit the bile acid pathway to overcome multiple barriers of the intestinal epithelium for oral insulin delivery. Biomaterials. 2018;151:13–23. https://doi.org/10.1016/j.biomaterials.2017.10.022.
Liu C, Shan W, Liu M, Zhu X, Xu J, Xu Y, et al. A novel ligand conjugated nanoparticles for oral insulin delivery. Drug Delivery. 2016;23(6):2015–25. https://doi.org/10.3109/10717544.2015.1058433.
Bashyal S, Seo J-E, Choi YW, Lee S. Bile acid transporter-mediated oral absorption of insulin via hydrophobic ion-pairing approach. J Control Release. 2021;338:644–61. https://doi.org/10.1016/j.jconrel.2021.08.06.
Zheng Y, Wu J, Shan W, Wu L, Zhou R, Liu M, et al. Multifunctional nanoparticles enable efficient oral delivery of biomacromolecules via improving payload stability and regulating the transcytosis pathway. ACS Appl Mater Interfaces. 2018;10(40):34039–49. https://doi.org/10.1021/acsami.8b13707.
Jana S, Jasmin N, Sen KK, Maiti S. Alginate nanostructures: Pharmaceutical approaches. Encycloped Marine Biotechnol. 2020;2:767–82. https://doi.org/10.1002/9781119143802.ch29.
Chia JJ, Shameli K, Yusefi M, Ali RR, Balasundram V, Teow S-Y. Preparation and Application of Cross-linked Alginate Nanoparticles as Drug Carrier: A Review. J Res Nanosci Nanotechnol. 2022;5(1):1–11. https://doi.org/10.37934/jrnn.5.1.111.
Karim A, Rehman A, Feng J, Noreen A, Assadpour E, Kharazmi MS, et al. Alginate-based nanocarriers for the delivery and controlled-release of bioactive compounds. Advances in Colloid and Interface Science. 2022:102744. https://doi.org/10.1016/j.cis.2022.102744
Huang Y, Wang Z. Preparation of composite aerogels based on sodium alginate, and its application in removal of Pb2+ and Cu2+ from water. Int J Biol Macromol. 2018;107:741–7. https://doi.org/10.1016/j.ijbiomac.2017.09.057.
Radmanesh F, Abandansari HS, Pahlavan S, Alikhani M, Karimi M, Rajabi S, et al. Optimization of miRNA delivery by using a polymeric conjugate based on deoxycholic acid-modified polyethylenimine. Int J Pharm. 2019;565:391–408. https://doi.org/10.1016/j.ijpharm.2019.05.009.
Huo M, Wang H, Zhang Y, Cai H, Zhang P, Li L, et al. Co-delivery of silybin and paclitaxel by dextran-based nanoparticles for effective anti-tumor treatment through chemotherapy sensitization and microenvironment modulation. J Control Release. 2020;321:198–210. https://doi.org/10.1016/j.jconrel.2020.02.017.
Chen Y, Li P, Modica JA, Drout RJ, Farha OK. Acid-resistant mesoporous metal–organic framework toward oral insulin delivery: protein encapsulation, protection, and release. J Am Chem Soc. 2018;140(17):5678–81. https://doi.org/10.1021/jacs.8b02089.
Abbasi S, Yousefi G, Firuzi O, Mohammadi‐Samani S. Design and cell cytotoxicity assessment of palmitoylated polyethylene glycol‐grafted chitosan as nanomicelle carrier for paclitaxel. Journal of Applied Polymer Science. 2016;133(13). https://doi.org/10.1002/app.43233
Zeng Z, Qi D, Yang L, Liu J, Tang Y, Chen H, et al. Stimuli-responsive self-assembled dendrimers for oral protein delivery. J Control Release. 2019;315:206–13. https://doi.org/10.1016/j.jconrel.2019.10.049.
Rao R, Liu X, Li Y, Tan X, Zhou H, Bai X, et al. Bioinspired zwitterionic polyphosphoester modified porous silicon nanoparticles for efficient oral insulin delivery. Biomaterials Sci. 2021. https://doi.org/10.1039/D0BM01772H.
Raguraman V, Jayasri M, Suthindhiran K. Magnetosome mediated oral Insulin delivery and its possible use in diabetes management. J Mater Sci - Mater Med. 2020;31(8):1–9. https://doi.org/10.1007/s10856-020-06417-2.
Sarmento B, Ribeiro A, Veiga F, Ferreira D. Development and validation of a rapid reversed-phase HPLC method for the determination of insulin from nanoparticulate systems. Biomed Chromatogr. 2006;20(9):898–903. https://doi.org/10.1002/bmc.616.
Tsai L-C, Chen C-H, Lin C-W, Ho Y-C, Mi F-L. Development of mutlifunctional nanoparticles self-assembled from trimethyl chitosan and fucoidan for enhanced oral delivery of insulin. Int J Biol Macromol. 2019;126:141–50. https://doi.org/10.1016/j.ijbiomac.2018.12.182.
Niu Z, Samaridou E, Jaumain E, Coëne J, Ullio G, Shrestha N, et al. PEG-PGA enveloped octaarginine-peptide nanocomplexes: an oral peptide delivery strategy. J Control Release. 2018;276:125–39. https://doi.org/10.1016/j.jconrel.2018.03.004.
Anchan RB, Koland M. Oral insulin delivery by chitosan coated solid lipid nanoparticles: Ex vivo and in vivo studies. J Young Pharm. 2021;13(1):43. https://doi.org/10.5530/jyp.2021.13.10.
Kristensen M, GuldsmedDiedrichsen R, Vetri V, Foderà V, Mørck NH. Increased carrier peptide stability through pH adjustment improves insulin and PTH (1–34) delivery in vitro and in vivo rather than by enforced carrier peptide-cargo complexation. Pharmaceutics. 2020;12(10):993. https://doi.org/10.3390/pharmaceutics12100993.
Diedrichsen RG, Harloff-Helleberg S, Werner U, Besenius M, Leberer E, Kristensen M, et al. Revealing the importance of carrier-cargo association in delivery of insulin and lipidated insulin. J Control Release. 2021;338:8–21. https://doi.org/10.1016/j.jconrel.2021.07.030.
Bozkaya O, Günay K, Arslan M, Gün GZ. Removal of anionic dyes with glycidyl methacrylate-grafted polyethylene terephthalate (PET) fibers modified with ethylenediamine. Res Chem Intermed. 2021;47(5):2075–93. https://doi.org/10.1007/s11164-021-04398-7.
Singh P, Niederer JP, Versteeg GF. Structure and activity relationships for amine-based CO2 absorbents-II. Chem Eng Res Des. 2009;87(2):135–44. https://doi.org/10.1016/j.cherd.2008.07.014.
Al-Shamkhani A, Duncan R. Synthesis, controlled release properties and antitumour activity of alginate-cis-aconityl-daunomycin conjugates. Int J Pharm. 1995;122(1–2):107–19. https://doi.org/10.1016/0378-5173(95)00055-N.
Kim K, Kwon S, Park JH, Chung H, Jeong SY, Kwon IC, et al. Physicochemical characterizations of self-assembled nanoparticles of glycol chitosan− deoxycholic acid conjugates. Biomacromol. 2005;6(2):1154–8. https://doi.org/10.1021/bm049305m.
Derkach SR, Voron’ko NG, Sokolan NI, Kolotova DS, Kuchina YA. Interactions between gelatin and sodium alginate: UV and FTIR studies. Journal of Dispersion Science and Technology. 2020;41(5):690–8. https://doi.org/10.1080/01932691.2019.1611437.
Liu K, Chen L, Huang L, Lai Y. Evaluation of ethylenediamine-modified nanofibrillated cellulose/chitosan composites on adsorption of cationic and anionic dyes from aqueous solution. Carbohyd Polym. 2016;151:1115–9. https://doi.org/10.1016/j.carbpol.2016.06.071.
Osman Abdi F, Özbaş Z. Cr (VI) Adsorption on Ethylenediamine Functionalized Grafted Sodium Alginate Beads: Effect of Process Parameters. Water Air Soil Pollut. 2021;232(12):1–15. https://doi.org/10.1007/s11270-021-05426-3.
Chiu C-T, Lee J-S, Chu C-S, Chang Y-P, Wang Y-J. Development of two alginate-based wound dressings. J Mater Sci - Mater Med. 2008;19(6):2503–13. https://doi.org/10.1007/s10856-008-3389-2.
Li L, Liang N, Wang D, Yan P, Kawashima Y, Cui F, et al. Amphiphilic polymeric micelles based on deoxycholic acid and folic acid modified chitosan for the delivery of paclitaxel. Int J Mol Sci. 2018;19(10):3132. https://doi.org/10.3390/ijms19103132.
Guo R, Chen L, Cai S, Liu Z, Zhu Y, Xue W, et al. Novel alginate coated hydrophobically modified chitosan polyelectrolyte complex for the delivery of BSA. J Mater Sci - Mater Med. 2013;24(9):2093–100. https://doi.org/10.1007/s10856-013-4977-3.
Wang F, Zhang D, Duan C, Jia L, Feng F, Liu Y, et al. Preparation and characterizations of a novel deoxycholic acid–O-carboxymethylated chitosan–folic acid conjugates and self-aggregates. Carbohyd Polym. 2011;84(3):1192–200. https://doi.org/10.1016/j.carbpol.2011.01.017.
Mooranian A, Negrulj R, Al-Salami H. Alginate-deoxycholic acid interaction and its impact on pancreatic Β-cells and insulin secretion and potential treatment of type 1 diabetes. J Pharm Innov. 2016;11(2):156–61. https://doi.org/10.1007/s12247-016-9248-7.
Mumuni MA, Kenechukwu FC, Ofokansi KC, Attama AA, Díaz DD. Insulin-loaded mucoadhesive nanoparticles based on mucin-chitosan complexes for oral delivery and diabetes treatment. Carbohyd Polym. 2020;229:115506. https://doi.org/10.1016/j.carbpol.2019.115506.
Zheng Y, Xing L, Chen L, Zhou R, Wu J, Zhu X, et al. Tailored elasticity combined with biomimetic surface promotes nanoparticle transcytosis to overcome mucosal epithelial barrier. Biomaterials. 2020;262:120323. https://doi.org/10.1016/j.biomaterials.2020.120323.
Kim YH, Gihm SH, Park CR, Lee KY, Kim TW, Kwon IC, et al. Structural characteristics of size-controlled self-aggregates of deoxycholic acid-modified chitosan and their application as a DNA delivery carrier. Bioconjug Chem. 2001;12(6):932–8. https://doi.org/10.1021/bc015510c.
Engberts JB, Kevelam J. Formation and stability of micelles and vesicles. Curr Opin Colloid Interface Sci. 1996;1(6):779–89. https://doi.org/10.1016/S1359-0294(96)80082-3.
Hashidzume A, Harada A. Micelles and vesicles. Encyclopedia of polymeric Nanomaterials. 2015:1238–41.
Sarmento B, Ferreira D, Veiga F, Ribeiro A. Characterization of insulin-loaded alginate nanoparticles produced by ionotropic pre-gelation through DSC and FTIR studies. Carbohyd Polym. 2006;66(1):1–7. https://doi.org/10.1016/j.carbpol.2006.02.008.
Xi Z, Ahmad E, Zhang W, Li J, Wang A, Wang N, et al. Dual-modified nanoparticles overcome sequential absorption barriers for oral insulin delivery. J Control Release. 2022;342:1–13. https://doi.org/10.1016/j.jconrel.2021.11.045.
Soltanzadeh M, Peighambardoust SH, Ghanbarzadeh B, Mohammadi M, Lorenzo JM. Chitosan nanoparticles as a promising nanomaterial for encapsulation of pomegranate (Punica granatum L.) peel extract as a natural source of antioxidants. Nanomaterials. 2021;11(6):1439. https://doi.org/10.3390/nano11061439.
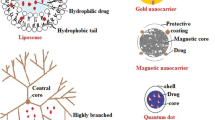
Sharma G, Parchur AK, Jagtap JM, Hansen CP, Joshi A. Hybrid nanostructures in targeted drug delivery. Hybrid nanostructures for cancer theranostics: Elsevier; 2019. p. 139–58. https://doi.org/10.1016/B978-0-12-813906-6.00008-1
Martins S, Sarmento B, Souto EB, Ferreira DC. Insulin-loaded alginate microspheres for oral delivery–effect of polysaccharide reinforcement on physicochemical properties and release profile. Carbohyd Polym. 2007;69(4):725–31. https://doi.org/10.1016/j.carbpol.2007.02.012.
Chen Z, Han S, Yang X, Xu L, Qi H, Hao G, et al. Overcoming multiple absorption barrier for insulin oral delivery using multifunctional nanoparticles based on chitosan derivatives and hyaluronic acid. Int J Nanomed. 2020;15:4877. https://doi.org/10.2147/IJN.S251627.
Sarmento B, Ribeiro A, Veiga F, Ferreira D. Development and characterization of new insulin containing polysaccharide nanoparticles. Colloids Surf, B. 2006;53(2):193–202. https://doi.org/10.1016/j.colsurfb.2006.09.012.
Zhang Y, Wei W, Lv P, Wang L, Ma G. Preparation and evaluation of alginate–chitosan microspheres for oral delivery of insulin. Eur J Pharm Biopharm. 2011;77(1):11–9. https://doi.org/10.1016/j.ejpb.2010.09.016.
Builders PF, Kunle OO, Okpaku LC, Builders MI, Attama AA, Adikwu MU. Preparation and evaluation of mucinated sodium alginate microparticles for oral delivery of insulin. Eur J Pharm Biopharm. 2008;70(3):777–83. https://doi.org/10.1016/j.ejpb.2008.06.021.
Tahtat D, Mahlous M, Benamer S, Khodja AN, Oussedik-Oumehdi H, Laraba-Djebari F. Oral delivery of insulin from alginate/chitosan crosslinked by glutaraldehyde. Int J Biol Macromol. 2013;58:160–8. https://doi.org/10.1016/j.ijbiomac.2013.03.064.
Afzal S, Maswal M, Dar AA. Rheological behavior of pH responsive composite hydrogels of chitosan and alginate: characterization and its use in encapsulation of citral. Colloids Surf, B. 2018;169:99–106. https://doi.org/10.1016/j.colsurfb.2018.05.002.
Wang Z, Zhang X, Gu J, Yang H, Nie J, Ma G. Electrodeposition of alginate/chitosan layer-by-layer composite coatings on titanium substrates. Carbohyd Polym. 2014;103:38–45. https://doi.org/10.1016/j.carbpol.2013.12.007.
Camacho DH, Uy SJY, Cabrera MJF, Lobregas MOS, Fajardo TJMC. Encapsulation of folic acid in copper-alginate hydrogels and it’s slow in vitro release in physiological pH condition. Food Res Int. 2019;119:15–22. https://doi.org/10.1016/j.foodres.2019.01.053.
Fang X, Zhao X, Yu G, Zhang L, Feng Y, Zhou Y, et al. Effect of molecular weight and pH on the self-assembly microstructural and emulsification of amphiphilic sodium alginate colloid particles. Food Hydrocolloids. 2020;103:105593. https://doi.org/10.1016/j.foodhyd.2019.105593.
Ramdhan T, Ching SH, Prakash S, Bhandari B. Time dependent gelling properties of cuboid alginate gels made by external gelation method: Effects of alginate-CaCl2 solution ratios and pH. Food Hydrocolloids. 2019;90:232–40. https://doi.org/10.1016/j.foodhyd.2018.12.022.
Stender EG, Khan S, Ipsen R, Madsen F, Hägglund P, Abou Hachem M, et al. Effect of alginate size, mannuronic/guluronic acid content and pH on particle size, thermodynamics and composition of complexes with β-lactoglobulin. Food Hydrocolloids. 2018;75:157–63. https://doi.org/10.1016/j.foodhyd.2017.09.001.
Sarmento B, Martins S, Ferreira D, Souto EB. Oral insulin delivery by means of solid lipid nanoparticles. Int J Nanomed. 2007;2(4):743. https://doi.org/10.2147/IJN.S2.4.743.
Xu Y, Zhan C, Fan L, Wang L, Zheng H. Preparation of dual crosslinked alginate–chitosan blend gel beads and in vitro controlled release in oral site-specific drug delivery system. Int J Pharm. 2007;336(2):329–37. https://doi.org/10.1016/j.ijpharm.2006.12.019.
Kim KS, Kwag DS, Hwang HS, Lee ES, Bae YH. Immense insulin intestinal uptake and lymphatic transport using bile acid conjugated partially uncapped liposome. Mol Pharm. 2018;15(10):4756–63. https://doi.org/10.1021/acs.molpharmaceut.8b00708.
Qiu J, Zhang J, Li A. Cytotoxicity and intestinal permeability of phycotoxins assessed by the human Caco-2 cell model. Ecotoxicol Environ Saf. 2023;249:114447. https://doi.org/10.1016/j.ecoenv.2022.114447.
Chen T, Li S, Zhu W, Liang Z, Zeng Q. Self-assembly pH-sensitive chitosan/alginate coated polyelectrolyte complexes for oral delivery of insulin. J Microencapsul. 2019;36(1):96–107. https://doi.org/10.1080/02652048.2019.1604846.
Manuja A, Kumar B, Athira S, Sarkar P, Riyesh T, Kumar N, et al. Zinc oxide nanoparticles encapsulated in polysaccharides alginate/gum acacia and iron oxide nanomatrices show enhanced biocompatibility and permeability to intestinal barrier. Food Hydrocolloids for Health. 2022;2:100050. https://doi.org/10.1016/j.fhfh.2021.100050.
Cheng H, Wu H, Guo T, Park HJ, Li J. Zinc insulin hexamer loaded alginate zinc hydrogel: Preparation, characterization and in vivo hypoglycemic ability. Eur J Pharm Biopharm. 2022;179:173–81. https://doi.org/10.1016/j.ejpb.2022.08.016.
Das D, Pham HTT, Lee S, Noh I. Fabrication of alginate-based stimuli-responsive, non-cytotoxic, terpolymric semi-IPN hydrogel as a carrier for controlled release of bovine albumin serum and 5-amino salicylic acid. Mater Sci Eng, C. 2019;98:42–53. https://doi.org/10.1016/j.msec.2018.12.127.
Wu S, Bin W, Tu B, Li X, Wang W, Liao S, et al. A delivery system for oral administration of proteins/peptides through bile acid transport channels. J Pharm Sci. 2019;108(6):2143–52. https://doi.org/10.1016/j.xphs.2019.01.027.
Li L, Jiang G, Yu W, Liu D, Chen H, Liu Y, et al. Preparation of chitosan-based multifunctional nanocarriers overcoming multiple barriers for oral delivery of insulin. Mater Sci Eng, C. 2017;70:278–86. https://doi.org/10.1016/j.msec.2016.08.083.
Zhou Y, Liu L, Cao Y, Yu S, He C, Chen X. A Nanocomposite vehicle based on metal–organic framework nanoparticle incorporated biodegradable microspheres for enhanced oral insulin delivery. ACS Appl Mater Interfaces. 2020;12(20):22581–92. https://doi.org/10.1021/acsami.0c04303.
Park J, Choi JU, Kim K, Byun Y. Bile acid transporter mediated endocytosis of oral bile acid conjugated nanocomplex. Biomaterials. 2017;147:145–54. https://doi.org/10.1016/j.biomaterials.2017.09.022.
Jia X, Yuan Z, Yang Y, Huang X, Han N, Liu X, et al. Multi-functional self-assembly nanoparticles originating from small molecule natural product for oral insulin delivery through modulating tight junctions. J Nanobiotechnol. 2022;20(1):1–17. https://doi.org/10.1186/s12951-022-01260-9.
Tlaskalová-Hogenová H, Štěpánková R, Kozáková H, Hudcovic T, Vannucci L, Tučková L, et al. The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases. Cellular Molecul Immunol. 2011;8(2):110–20. https://doi.org/10.1038/cmi.2010.67.
Fasano A. Leaky gut and autoimmune diseases. Clinical Reviews in Allergy & Immunology. 2012;42:71–8. https://doi.org/10.1007/s12016-011-8291-x
Yao W, Xu Z, Sun J, Luo J, Wei Y, Zou J. Deoxycholic acid-functionalised nanoparticles for oral delivery of rhein. Eur J Pharm Sci. 2021;159:105713. https://doi.org/10.1016/j.ejps.2021.105713.
Li M, Wang Q, Li Y, Cao S, Zhang Y, Wang Z, et al. Apical sodium-dependent bile acid transporter, drug target for bile acid related diseases and delivery target for prodrugs: Current and future challenges. Pharmacol Ther. 2020;212:107539. https://doi.org/10.1016/j.pharmthera.2020.107539.
Pavlović N, Goločorbin-Kon S, Ðanić M, Stanimirov B, Al-Salami H, Stankov K, et al. Bile acids and their derivatives as potential modifiers of drug release and pharmacokinetic profiles. Front Pharmacol. 2018;9:1283. https://doi.org/10.3389/fphar.2018.01283.
Xu Z, Hou Y, Sun J, Zhu L, Zhang Q, Yao W, et al. Deoxycholic acid-chitosan coated liposomes combined with in situ colonic gel enhances renal fibrosis therapy of emodin. Phytomedicine. 2022;101:154110. https://doi.org/10.1016/j.phymed.2022.154110.
Mahmud F, Jeon O-C, Al-Hilal TA, Kweon S, Yang VC, Lee DS, et al. Absorption mechanism of a physical complex of monomeric insulin and deoxycholyl-l-lysyl-methylester in the small intestine. Mol Pharm. 2015;12(6):1911–20. https://doi.org/10.1021/mp500626a.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Razmjooei, M., Hosseini, S.M., Yousefi, G. et al. Exploiting Apical Sodium-Dependent Bile Acid Transporter (ASBT)-Mediated Endocytosis with Multi-Functional Deoxycholic Acid Grafted Alginate Amide Nanoparticles as an Oral Insulin Delivery System. Pharm Res 41, 335–353 (2024). https://doi.org/10.1007/s11095-023-03641-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-023-03641-7