Abstract
Purpose
Glioblastoma multiforme (GBM) is a grade IV, highly proliferative, and malignant form of brain tumor with a 5-year survival rate at ~ 5%. Current treatment strategies for GBM include surgery, radiation, and chemotherapy. Major challenges in GBM management include difficulties in surgical resection due to brain’s vital functions and GBM metastasis, development of resistance to temozolomide (TMZ), and protection of tumor by blood brain barrier (BBB). Therefore, we aimed to discover a novel therapeutic for GBM by targeting its metabolic reprogramming.
Method
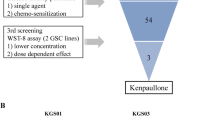
We screened metabolic inhibitors by their effects on GBM cell viability by MTT assay. We discovered an FDA-approved drug stiripentol (STP) in our screening of metabolic inhibitors in GBM cells. STP is used for Dravet syndrome (a rare epilepsy). We further tested efficacy of STP using proliferation assay, clonogenic assay, in vitro migration assay, cell cycle assay, apoptosis assay, and in U87 3D spheroids. We also tested the toxicity of STP, and combinations used in the study on normal human dermal fibroblasts.
Results
STP was effective in decreasing GBM cell viability, proliferation, clonogenic ability, and migration. Moreover, cell cycle changes were involved but robust apoptosis was absent in STP’s anticancer effects. STP was effective in 3D spheroid models, and in TMZ-resistant cells. STP showed additive or synergistic effect with TMZ in different anticancer assays on GBM cells and was considerably less toxic in normal cells.
Conclusion
Our results indicate that STP can be an effective GBM therapeutic that enhances the effects of TMZ on GBM cells. Importantly, STP reduced viability of TMZ-resistant cells. Our results warrant further studies in the mechanistic basis of STP’s effects on GBM cells and the preclinical potential of STP in animal models.









Similar content being viewed by others
References
Chen B, Chen C, Zhang Y, Xu J. Recent incidence trend of elderly patients with glioblastoma in the United States, 2000–2017. BMC Cancer. 2021;21:54.
Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al. CBTRUS Statistical Report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro-Oncol. 2015;17(Suppl 4):iv1-62.
Gilbert MR, Wang M, Aldape KD, Stupp R, Hegi ME, Jaeckle KA, et al. Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31:4085–91.
Khaddour K, Johanns TM, Ansstas G. The landscape of novel therapeutics and challenges in glioblastoma multiforme: contemporary state and future directions. Pharmaceuticals [Internet]. 2020 [cited 2021 May 14];13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7696377/.
Chen X, Zhang M, Gan H, Wang H, Lee J-H, Fang D, et al. A novel enhancer regulates MGMT expression and promotes temozolomide resistance in glioblastoma. Nat Commun. 2018;9:2949.
Jiapaer S, Furuta T, Tanaka S, Kitabayashi T, Nakada M. Potential strategies overcoming the temozolomide resistance for glioblastoma. Neurol Med Chir (Tokyo). 2018;58:405–21.
Golub D, Iyengar N, Dogra S, Wong T, Bready D, Tang K, et al. Mutant isocitrate dehydrogenase inhibitors as targeted cancer therapeutics. Front Oncol [Internet]. 2019 [cited 2020 Jun 15];9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6534082/.
Hanahan D. Hallmarks of cancer: New dimensions. Cancer Discov. 2022;12(1):31–46. https://doi.org/10.1158/2159-8290.CD-21-1059.
Hanahan D, Weinberg RA. The Hallmarks of Cancer. Cell. 2000;100:57–70.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Strickland M, Stoll EA. Metabolic reprogramming in glioma. Front Cell Dev Biol [Internet]. 2017 [cited 2019 Sep 29];5. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5405080/.
Faubert B, Solmonson A, DeBerardinis RJ. Metabolic reprogramming and cancer progression. Science [Internet]. 2020 [cited 2020 Jun 15];368:eaaw5473. Available from: https://www.sciencemag.org/lookup/doi/10.1126/science.aaw5473.
Pavlova NN, Thompson CB. The emerging hallmarks of cancer metabolism. Cell Metab [Internet]. 2016 [cited 2020 Jun 9];23:27–47. Available from: https://linkinghub.elsevier.com/retrieve/pii/S155041311500621X.
DeBerardinis RJ, Lum JJ, Hatzivassiliou G, Thompson CB. The biology of cancer: metabolic reprogramming fuels cell growth and proliferation. Cell Metab. 2008;7:11–20.
Fadaka A, Ajiboye B, Ojo O, Adewale O, Olayide I, Emuowhochere R. Biology of glucose metabolization in cancer cells. J Oncol Sci. 2017;3:45–51.
Sun RC, Dukhande VV, Zhou Z, Young LEA, Emanuelle S, Brainson CF, et al. Nuclear glycogenolysis modulates histone acetylation in human non-small cell lung cancers. Cell Metab [Internet]. 2019 [cited 2020 Jan 6];30:903–916.e7. Available from: http://www.sciencedirect.com/science/article/pii/S1550413119304437.
Barot S, Abo-Ali EM, Zhou DL, Palaguachi C, Dukhande VV. Inhibition of glycogen catabolism induces intrinsic apoptosis and augments multikinase inhibitors in hepatocellular carcinoma cells. Exp Cell Res. 2019;381:288–300.
Barot S, Stephenson OJ, Priya Vemana H, Yadav A, Bhutkar S, Trombetta LD, et al. Metabolic alterations and mitochondrial dysfunction underlie hepatocellular carcinoma cell death induced by a glycogen metabolic inhibitor. Biochem Pharmacol. 2022;203: 115201.
Brown AM, Ransom BR. Astrocyte glycogen and brain energy metabolism. Glia [Internet]. 2007;55:1263–71. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17659525.
de la Cruz-López KG, Castro-Muñoz LJ, Reyes-Hernández DO, García-Carrancá A, Manzo-Merino J. Lactate in the regulation of tumor microenvironment and therapeutic approaches. Front Oncol [Internet]. Frontiers; 2019 [cited 2020 Jun 10];9. Available from: https://www.frontiersin.org/articles/10.3389/fonc.2019.01143/full.
Valvona CJ, Fillmore HL, Nunn PB, Pilkington GJ. The regulation and function of lactate dehydrogenase a: therapeutic potential in brain tumor. Brain Pathol. 2016;26:3–17.
Du P, Liao Y, Zhao H, Zhang J, Muyiti Keremu, et al. ANXA2P2/miR-9/LDHA axis regulates Warburg effect and affects glioblastoma proliferation and apoptosis. Cell Signal. 2020;74:109718.
Feng Y, Xiong Y, Qiao T, Li X, Jia L, Han Y. Lactate dehydrogenase A: a key player in carcinogenesis and potential target in cancer therapy. Cancer Med [Internet]. 2018 [cited 2020 Jun 10];7:6124–36. Available from: http://doi.wiley.com/10.1002/cam4.1820.
Faubert B, Li KY, Cai L, Hensley CT, Kim J, Zacharias LG, et al. Lactate metabolism in human lung tumors. Cell. 2017;171:358-371.e9.
Brooks GA. The science and translation of lactate shuttle theory. Cell Metab [Internet]. 2018 [cited 2020 Mar 15];27:757–85. Available from: https://www.cell.com/cell-metabolism/abstract/S1550-4131(18)30186-4.
Chen Y-J, Mahieu NG, Huang X, Singh M, Crawford PA, Johnson SL, et al. Lactate metabolism is associated with mammalian mitochondria. Nat Chem Biol [Internet]. 2016 [cited 2020 Jun 10];12:937–43. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5069139/.
Sada N, Lee S, Katsu T, Otsuki T, Inoue T. Targeting LDH enzymes with a stiripentol analog to treat epilepsy. Science. 2015;347:1362–7.
Buck ML, Goodkin HP. Stiripentol: a novel antiseizure medication for the management of dravet syndrome. Ann Pharmacother. 2019;53:1136–44.
Bonuccelli G, De Francesco EM, de Boer R, Tanowitz HB, Lisanti MP. NADH autofluorescence, a new metabolic biomarker for cancer stem cells: identification of Vitamin C and CAPE as natural products targeting “stemness.” Oncotarget. 2017;8:20667–78.
Fisher JL. The anticonvulsant stiripentol acts directly on the GABAA receptor as a positive allosteric modulator. Neuropharmacology. 2009;56:190–7.
Di Veroli GY, Fornari C, Wang D, Mollard S, Bramhall JL, Richards FM, et al. Combenefit: an interactive platform for the analysis and visualization of drug combinations. Bioinformatics. 2016;32:2866–8.
Hanahan D. Hallmarks of cancer: new dimensions. Cancer Discov. 2022;12:31–46.
Faubert B, Solmonson A, DeBerardinis RJ. Metabolic reprogramming and cancer progression. Science. 2020;368:eaaw5473.
Fisher JL. The effects of stiripentol on GABAA receptors: stiripentol and GABAA Receptors. Epilepsia. 2011;52:76–8.
Baumann F, Leukel P, Doerfelt A, Beier CP, Dettmer K, Oefner PJ, et al. Lactate promotes glioma migration by TGF-β2–dependent regulation of matrix metalloproteinase-2. Neuro-Oncol. 2009;11:368–80.
Goetze K, Walenta S, Ksiazkiewicz M, Kunz-Schughart LA, Mueller-Klieser W. Lactate enhances motility of tumor cells and inhibits monocyte migration and cytokine release. Int J Oncol. 2011;39:453–63.
Liu Y, Guo J-Z, Liu Y, Wang K, Ding W, Wang H, et al. Nuclear lactate dehydrogenase A senses ROS to produce α-hydroxybutyrate for HPV-induced cervical tumor growth. Nat Commun [Internet]. Nature Publishing Group; 2018 [cited 2020 Jun 10];9:4429. Available from: https://www.nature.com/articles/s41467-018-06841-7.
Granchi C, Bertini S, Macchia M, Minutolo F. Inhibitors of lactate dehydrogenase isoforms and their therapeutic potentials. Curr Med Chem. 2010;17:672–97.
Lyne SB, Yamini B. An alternative pipeline for glioblastoma therapeutics: a systematic review of drug repurposing in glioblastoma. Cancers. 2021;13:1953.
Acknowledgements
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award numbers R16GM145557 and SC2GM125550 to Dukhande V. and by funds from the College of Pharmacy and Health Sciences, St. John’s University, Queens, NY, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information

Supplemental Fig. 1
STP decreases cell viability in LN229 and SW1088. A) Cellular viability values of STP and TMZ on LN229 and B) SW1088 cells after 48 hr of treatment plotted on log (dose) - response curve on GraphPad Prism 9. (PNG 157 kb)

Supplemental Fig. 2
Morphological changes on STP and TMZ synergistic effect on U87. Representative brightfield images of synergy studies on U87 cells after 48 hr treatment with STP, TMZ, and their combinations at 100X magnification. Images were acquired using Evos FL2 Auto microscope. (PNG 1405 kb)

Supplemental Fig. 3
STP and TMZ have synergistic effect on U87 and U138. A) Loewe and B) Bliss synergy matrix plots obtained from Combenefit software upon running the cell viability of U87 and U138 cells respectively at various concentrations of STP, TMZ, and their combinations. (PNG 101 kb)

Supplemental Fig. 4
Effect of STP and combination on migration ability of U87. A) Representative brightfield images of U87 cells after treatment with STP, TMZ, their combination, and SB43512 positive control for its effect on migration after a scratch on U87 monolayer. Images acquired on Evos FL2 auto microscope. B) Quantification using Adobe illustrator was plotted on GraphPad Prism 9. Two-way ANOVA, n=3, * p < 0.03, ***p < 0.001. (PNG 1362 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yadav, A., Alnakhli, A., Vemana, H.P. et al. Repurposing an Antiepileptic Drug for the Treatment of Glioblastoma. Pharm Res 39, 2871–2883 (2022). https://doi.org/10.1007/s11095-022-03399-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03399-4