Abstract
Purpose
Quantitative targeted absolute proteomics (QTAP) quantifies proteins by measuring the signature peptides produced from target proteins by trypsin digestion. The selection of signature peptides is critical for reliable peptide quantification. The purpose of this study was to comprehensively assess the digestion efficiency and stability of tryptic peptides and to identify optimal signature peptides for human hepatic transporters and membrane marker proteins.
Methods
The plasma membrane fraction of the human liver was digested at different time points and the peptides were comprehensively quantified using quantitative proteomics. Transporters and membrane markers were quantified using the signature peptides by QTAP.
Results
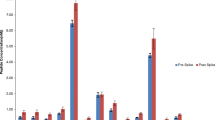
Tryptic peptides were classified into clusters with low digestion efficiency, low stability, and high digestion efficiency and stability. Using the cluster information, we found that a proline residue next to the digestion site or the peptide position in or close to the transmembrane domains lowers digestion efficiency. A peptide containing cysteine at the N-terminus or arginine-glycine lowers peptide stability. Based on this information and the time course of peptide quantification, optimal signature peptides were identified for human hepatic transporters and membrane markers. The quantification of transporters with multiple signature peptides yielded consistent absolute values with less than 30% of coefficient variants in human liver microsomes and homogenates.
Conclusions
The signature peptides selected in the present study enabled the reliable quantification of human hepatic transporters. The QTAP protocol using these optimal signature peptides provides quantitative data on hepatic transporters usable for integrated pharmacokinetic studies.





Similar content being viewed by others
Data Availability
Raw data files of proteomic analysis have been deposited in jPOST (http://jpostdb.org.jPOST ID: JPST001658/PXD034402).
References
Masuda T, Mori A, Ito S, Ohtsuki S. Quantitative and targeted proteomics-based identification and validation of drug efficacy biomarkers. Drug Metab Pharmacokinet. 2021;36: 100361.
Uchida Y, Tachikawa M, Obuchi W, Hoshi Y, Tomioka Y, Ohtsuki S, et al. A study protocol for quantitative targeted absolute proteomics (QTAP) by LC-MS/MS: application for inter-strain differences in protein expression levels of transporters, receptors, claudin-5, and marker proteins at the blood-brain barrier in ddY, FVB, and C57BL/6J mice. Fluids Barriers CNS. 2013;10:21.
Olsen JV, Ong SE, Mann M. Trypsin cleaves exclusively C-terminal to arginine and lysine residues. Mol Cell Proteomics. 2004;3:608–14.
Bi YA, Qiu X, Rotter CJ, Kimoto E, Piotrowski M, Varma MV, et al. Quantitative assessment of the contribution of sodium-dependent taurocholate co-transporting polypeptide (NTCP) to the hepatic uptake of rosuvastatin, pitavastatin and fluvastatin. Biopharm Drug Dispos. 2013;34:452–61.
Bosgra S, van de Steeg E, Vlaming ML, Verhoeckx KC, Huisman MT, Verwei M, et al. Predicting carrier-mediated hepatic disposition of rosuvastatin in man by scaling from individual transfected cell-lines in vitro using absolute transporter protein quantification and PBPK modeling. Eur J Pharm Sci. 2014;65:156–66.
Ishida K, Ullah M, Tóth B, Juhasz V, Unadkat JD. Successful prediction of in vivo hepatobiliary clearances and hepatic concentrations of rosuvastatin using sandwich-cultured rat hepatocytes, transporter-expressing cell lines, and quantitative proteomics. Drug Metab Dispos. 2018;46:66–74.
Li N, Singh P, Mandrell KM, Lai Y. Improved extrapolation of hepatobiliary clearance from in vitro sandwich cultured rat hepatocytes through absolute quantification of hepatobiliary transporters. Mol Pharm. 2010;7:630–41.
Ito S, Lee W, Park JE, Yasunaga M, Mori A, Ohtsuki S, et al. Transient, tunable expression of NTCP and BSEP in MDCKII cells for kinetic delineation of the rate-determining process and inhibitory effects of rifampicin in hepatobiliary transport of taurocholate. J Pharm Sci. 2021;110:365–75.
Kumar V, Salphati L, Hop CECA, Xiao G, Lai Y, Mathias A, et al. A comparison of total and plasma membrane abundance of transporters in suspended, plated, sandwich-cultured human hepatocytes versus human liver tissue using quantitative targeted proteomics and cell surface biotinylation. Drug Metab Dispos. 2019;47:350–7.
Ohtsuki S, Kawakami H, Inoue T, Nakamura K, Tateno C, Katsukura Y, et al. Validation of uPA/SCID mouse with humanized liver as a human liver model: protein quantification of transporters, cytochromes P450, and UDP-glucuronosyltransferases by LC-MS/MS. Drug Metab Dispos. 2014;42:1039–43.
Schaefer O, Ohtsuki S, Kawakami H, Inoue T, Liehner S, Saito A, et al. Absolute quantification and differential expression of drug transporters, cytochrome P450 enzymes, and UDP-glucuronosyltransferases in cultured primary human hepatocytes. Drug Metab Dispos. 2012;40:93–103.
Wang L, Prasad B, Salphati L, Chu X, Gupta A, Hop CE, et al. Interspecies variability in expression of hepatobiliary transporters across human, dog, monkey, and rat as determined by quantitative proteomics. Drug Metab Dispos. 2015;43:367–74.
Wang L, Collins C, Kelly EJ, Chu X, Ray AS, Salphati L, et al. Transporter expression in liver tissue from subjects with alcoholic or hepatitis C cirrhosis quantified by targeted quantitative proteomics. Drug Metab Dispos. 2016;44:1752–8.
Prasad B, Gaedigk A, Vrana M, Gaedigk R, Leeder JS, Salphati L, et al. Ontogeny of hepatic drug transporters as quantified by LC-MS/MS proteomics. Clin Pharmacol Ther. 2016;100:362–70.
van Groen BD, van de Steeg E, Mooij MG, van Lipzig MMH, de Koning BAE, Verdijk RM, et al. Proteomics of human liver membrane transporters: a focus on fetuses and newborn infants. Eur J Pharm Sci. 2018;124:217–27.
Peng KW, Bacon J, Zheng M, Guo Y, Wang MZ. Ethnic variability in the expression of hepatic drug transporters: absolute quantification by an optimized targeted quantitative proteomic approach. Drug Metab Dispos. 2015;43:1045–55.
Prasad B, Evers R, Gupta A, Hop CE, Salphati L, Shukla S, et al. Interindividual variability in hepatic organic anion-transporting polypeptides and P-glycoprotein (ABCB1) protein expression: quantification by liquid chromatography tandem mass spectroscopy and influence of genotype, age, and sex. Drug Metab Dispos. 2014;42:78–88.
Vildhede A, Nguyen C, Erickson BK, Kunz RC, Jones R, Kimoto E, et al. Comparison of proteomic quantification approaches for hepatic drug transporters: multiplexed global quantitation correlates with targeted proteomic quantitation. Drug Metab Dispos. 2018;46:692–6.
Wegler C, Gaugaz FZ, Andersson TB, Wiśniewski JR, Busch D, Gröer C, et al. Variability in mass spectrometry-based quantification of clinically relevant drug transporters and drug metabolizing enzymes. Mol Pharm. 2017;14:3142–51.
Prasad B, Achour B, Artursson P, Hop CECA, Lai Y, Smith PC, et al. Toward a consensus on applying quantitative liquid chromatography-tandem mass spectrometry proteomics in translational pharmacology research: a white paper. Clin Pharmacol Ther. 2019;106:525–43.
Badee J, Achour B, Rostami-Hodjegan A, Galetin A. Meta-analysis of expression of hepatic organic anion-transporting polypeptide (OATP) transporters in cellular systems relative to human liver tissue. Drug Metab Dispos. 2015;43:424–32.
Fallon JK, Neubert H, Hyland R, Goosen TC, Smith PC. Targeted quantitative proteomics for the analysis of 14 UGT1As and -2Bs in human liver using NanoUPLC-MS/MS with selected reaction monitoring. J Proteome Res. 2013;12:4402–13.
Chen B, Liu L, Ho H, Chen Y, Yang Z, Liang X, et al. Strategies of drug transporter quantitation by lc-ms: importance of peptide selection and digestion efficiency. AAPS J. 2017;19:1469–78.
Kamiie J, Ohtsuki S, Iwase R, Ohmine K, Katsukura Y, Yanai K, et al. Quantitative atlas of membrane transporter proteins: development and application of a highly sensitive simultaneous LC/MS/MS method combined with novel in-silico peptide selection criteria. Pharm Res. 2008;25:1469–83.
Uchida Y, Sasaki H, Terasaki T. Establishment and validation of highly accurate formalin-fixed paraffin-embedded quantitative proteomics by heat-compatible pressure cycling technology using phase-transfer surfactant and SWATH-MS. Sci Rep. 2020;10:11271.
Masuda T, Saito N, Tomita M, Ishihama Y. Unbiased quantitation of Escherichia coli membrane proteome using phase transfer surfactants. Mol Cell Proteomics. 2009;8:2770–7.
Masuda T, Tomita M, Ishihama Y. Phase transfer surfactant-aided trypsin digestion for membrane proteome analysis. J Proteome Res. 2008;7:731–40.
Demichev V, Messner CB, Vernardis SI, Lilley KS, Ralser M. DIA-NN: neural networks and interference correction enable deep proteome coverage in high throughput. Nat Methods. 2020;17:41–4.
Slechtova T, Gilar M, Kalikova K, Tesarova E. Insight into trypsin miscleavage: comparison of kinetic constants of problematic peptide sequences. Anal Chem. 2015;87:7636–43.
Nakamura K, Hirayama-Kurogi M, Ito S, Kuno T, Yoneyama T, Obuchi W, et al. Large-scale multiplex absolute protein quantification of drug-metabolizing enzymes and transporters in human intestine, liver, and kidney microsomes by SWATH-MS: Comparison with MRM/SRM and HR-MRM/PRM. Proteomics. 2016;16:2106–17.
Ohtsuki S, Schaefer O, Kawakami H, Inoue T, Liehner S, Saito A, et al. Simultaneous absolute protein quantification of transporters, cytochromes P450, and UDP-glucuronosyltransferases as a novel approach for the characterization of individual human liver: comparison with mRNA levels and activities. Drug Metab Dispos. 2012;40:83–92.
Pan Y, Cheng K, Mao J, Liu F, Liu J, Ye M, et al. Quantitative proteomics reveals the kinetics of trypsin-catalyzed protein digestion. Anal Bioanal Chem. 2014;406:6247–56.
Geoghegan KF, Hoth LR, Tan DH, Borzilleri KA, Withka JM, Boyd JG. Cyclization of N-terminal S-carbamoylmethylcysteine causing loss of 17 Da from peptides and extra peaks in peptide maps. J Proteome Res. 2002;1:181–7.
Purwaha P, Silva LP, Hawke DH, Weinstein JN, Lorenzi PL. An artifact in LC-MS/MS measurement of glutamine and glutamic acid: in-source cyclization to pyroglutamic acid. Anal Chem. 2014;86:5633–7.
Yang H, Zubarev RA. Mass spectrometric analysis of asparagine deamidation and aspartate isomerization in polypeptides. Electrophoresis. 2010;31:1764–72.
Radkiewicz JL, Zipse H, Clarke S, Houk KN. Neighboring side chain effects on asparaginyl and aspartyl degradation: an ab initio study of the relationship between peptide conformation and backbone NH acidity. J Am Chem Soc. 2001;123:3499–506.
Perdivara I, Deterding LJ, Przybylski M, Tomer KB. Mass spectrometric identification of oxidative modifications of tryptophan residues in proteins: chemical artifact or post-translational modification? J Am Soc Mass Spectrom. 2010;21:1114–7.
Simat TJ, Steinhart H. Oxidation of free tryptophan and tryptophan residues in peptides and proteins. J Agric Food Chem. 1998;46:490–8.
Wang X, Swensen AC, Zhang T, Piehowski PD, Gaffrey MJ, Monroe ME, et al. Accurate identification of deamidation and citrullination from global shotgun proteomics data using a dual-search delta score strategy. J Proteome Res. 2020;19:1863–72.
Yagi R, Masuda T, Ogata S, Mori A, Ito S, Ohtsuki S. Proteomic evaluation of plasma membrane fraction prepared from a mouse liver and kidney using a bead homogenizer: enrichment of drug-related transporter proteins. Mol Pharm. 2020;17:4101–13.
Morse BL, Kolur A, Hudson LR, Hogan AT, Chen LH, Brackman RM, et al. Pharmacokinetics of Organic Cation Transporter 1 (OCT1) Substrates in Oct1/2 Knockout Mice and Species Difference in Hepatic OCT1-Mediated Uptake. Drug Metab Dispos. 2020;48:93–105.
Shu Y, Brown C, Castro RA, Shi RJ, Lin ET, Owen RP, et al. Effect of genetic variation in the organic cation transporter 1, OCT1, on metformin pharmacokinetics. Clin Pharmacol Ther. 2008;83:273–80.
Chen L, Shu Y, Liang X, Chen EC, Yee SW, Zur AA, et al. OCT1 is a high-capacity thiamine transporter that regulates hepatic steatosis and is a target of metformin. Proc Natl Acad Sci U S A. 2014;111:9983–8.
Eisenhofer G, Kopin IJ, Goldstein DS. Catecholamine metabolism: a contemporary view with implications for physiology and medicine. Pharmacol Rev. 2004;56:331–49.
Boxberger KH, Hagenbuch B, Lampe JN. Common drugs inhibit human organic cation transporter 1 (OCT1)-mediated neurotransmitter uptake. Drug Metab Dispos. 2014;42:990–5.
Balogh L, Kimoto E, Chupka J, Zhang H, Lai Y. Membrane protein quantification by peptide-based mass spectrometry approaches: studies on the organic anion-transporting polypeptide family. J Proteomics Bioinform. 2013;6:229–36.
Couto N, Al-Majdoub ZM, Achour B, Wright PC, Rostami-Hodjegan A, Barber J. Quantification of Proteins Involved in Drug Metabolism and Disposition in the Human Liver Using Label-Free Global Proteomics. Mol Pharm. 2019;16:632–47.
Shawahna R, Uchida Y, Declèves X, Ohtsuki S, Yousif S, Dauchy S, et al. Transcriptomic and quantitative proteomic analysis of transporters and drug metabolizing enzymes in freshly isolated human brain microvessels. Mol Pharm. 2011;8:1332–41.
Ji C, Tschantz WR, Pfeifer ND, Ullah M, Sadagopan N. Development of a multiplex UPLC-MRM MS method for quantification of human membrane transport proteins OATP1B1, OATP1B3 and OATP2B1 in in vitro systems and tissues. Anal Chim Acta. 2012;717:67–76.
Kinzi J, Grube M, Schwabedissen Meyer Zu, HE. OATP2B1 - The underrated member of the organic anion transporting polypeptide family of drug transporters? Biochem Pharmacol. 2021;188:114534.
Funding
This work was supported in part by JSPS KAKENHI (21H02649), JST CREST (JP171024167), and AMED BINDS (22ama121018).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design. Mori S conducted the experiments and performed data analysis. Mori S and Ohtsuki S wrote the manuscript. All authors provided final approval for the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Sumio Ohtsuki is a full professor at Kumamoto University and is also a director of Proteomedix Frontiers. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mori, A., Masuda, T., Ito, S. et al. Human Hepatic Transporter Signature Peptides for Quantitative Targeted Absolute Proteomics: Selection, Digestion Efficiency, and Peptide Stability. Pharm Res 39, 2965–2978 (2022). https://doi.org/10.1007/s11095-022-03387-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03387-8