Abstract
Aims
Gastric ulcer is a continuous worldwide threat that inquires protective agents. Olmesartan (OLM) has potent anti-oxidant and anti-inflammatory characters, yet having limited bioavailability. We targeted the gastro-protective potential and probable mechanism of OLM and its niosomal form against indomethacin (IND) induced-gastric ulcer in rats.
Main methods
we prepared OLM niosomes (OLM-NIO) with different surfactant: cholesterol molar ratios. We evaluated particle size, zeta-potential, polydispersity, and entrapment efficiency. In-vitro release study, Fourier transform infrared spectroscopy, differential scanning calorimetry, and transmission electron microscopy were performed for selected niosomes. In-vivo, we used oral Omeprazole (30 mg/kg), OLM or OLM-NIO (10 mg/kg) for 3 days before IND (25 mg/kg) ingestion. We assessed gastric lesions, oxidative and inflammatory markers.
Key findings
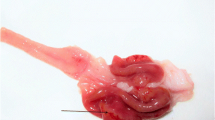
OLM-NIO prepared with span 60:cholesterol ratio (1:1) showed high entrapment efficiency 93 ± 2%, small particle size 159.3 ± 6.8 nm, low polydispersity 0.229 ± 0.009, and high zeta-potential −35.3 ± 1.2 mV, with sustained release mechanism by release data. In-vivo macroscopical and histological results showed gastro-protective effects of OLM pretreatment, which improved oxidative stress parameters and enhanced the gastric mucosal cyclooxygenase-1 (COX-1) and prostaglandin E2 (PGE2) contents. OLM pretreatment suppressed interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) contents and translocation of p38 mitogen-activated protein kinase (p38-MAPK). Besides, OLM substantially promoted the nuclear factor erythroid 2-related factor 2 (Nrf2)/heme oxygenase-1 (HO-1) protective pathway. OLM-NIO furtherly improved all previous outcomes.
Significance
We explored OLM anti-ulcerative effects, implicating oxidative stress and inflammation improvement, mediated by the Nrf2/HO-1 signaling pathway and p38-MAPK translocation. Meanwhile, the more bioavailable OLM-NIO achieved better gastro-protective effects compared to conventional OLM form.










Similar content being viewed by others
References
Wu Y, Murray GK, Byrne EM, Sidorenko J, Visscher PM, Wray NR. GWAS of peptic ulcer disease implicates Helicobacter pylori infection, other gastrointestinal disorders and depression. Nat Commun [Internet]. Springer US; 2021;12:1–17. Available from: https://doi.org/10.1038/s41467-021-21280-7
AlKreathy HM, Alghamdi MK, Esmat A. Tetramethylpyrazine ameliorates indomethacin-induced gastric ulcer in rats: Impact on oxidative, inflammatory, and angiogenic machineries. Saudi Pharm J [Internet]. The Author(s); 2020 [cited 2021 Mar 23];28:916–26. Available from: https://doi.org/10.1016/j.jsps.2020.06.012.
Charpignon C, Lesgourgues B, Pariente A, Nahon S, Pelaquier A, Gatineau-Sailliant G, et al. Peptic ulcer disease: One in five is related to neither Helicobacter pylori nor aspirin/NSAID intake. Aliment Pharmacol Ther. 2013;38:946–54.
El-Ashmawy NE, Khedr EG, El-Bahrawy HA, Selim HM. Nebivolol prevents indomethacin-induced gastric ulcer in rats. J Immunotoxicol [Internet]. Taylor and Francis Ltd; 2016 [cited 2021 Apr 8];13:580–9. Available from: https://www.tandfonline.com/action/journalInformation?journalCode=iimt20http://dx.doi.org/10.3109/1547691X.2016.1142488
J C, N R-G, B C, C V-L, A F-R, F N, et al. Individual NSAIDs and upper gastrointestinal complications: a systematic review and meta-analysis of observational studies (the SOS project). Drug Saf [Internet]. Drug Saf; 2012 [cited 2021 Oct 6];35:1127–46. Available from: https://pubmed.ncbi.nlm.nih.gov/23137151/
Arab HH, Salama SA, Omar HA, Arafa ESA, Maghrabi IA. Diosmin protects against ethanol-induced gastric injury in rats: Novel anti-ulcer actions. PLoS One. 2015;10:1–21.
Satou R, Penrose H, Navar LG. Inflammation as a Regulator of the Renin-Angiotensin System and Blood Pressure [Internet]. Curr. Hypertens. Rep. Current Medicine Group LLC 1; 2018 [cited 2021 Apr 19]. p. 100. Available from: /pmc/articles/PMC6203444/.
Saber S, Khalil RM, Abdo WS, Nassif D, El-Ahwany E. Olmesartan ameliorates chemically-induced ulcerative colitis in rats via modulating NFκB and Nrf-2/HO-1 signaling crosstalk. Toxicol Appl Pharmacol [Internet]. Academic Press Inc.; 2019 [cited 2021 Apr 8];364:120–32. Available from: https://pubmed.ncbi.nlm.nih.gov/30594690/
Nakagiri A, Sunamoto M, Murakami M. Angiotensin AT1 receptor blockers suppress ischemia/reperfusion-induced gastric injury in rats. Inflammopharmacology [Internet]. Inflammopharmacology; 2007 [cited 2021 Apr 19];15:171–4. Available from: https://pubmed.ncbi.nlm.nih.gov/17701020/
Mason RP. Optimal therapeutic strategy for treating patients with hypertension and atherosclerosis: Focus on olmesartan medoxomil [Internet]. Vasc. Health Risk Manag. DOVE Medical Press Ltd.; 2011 [cited 2021 Apr 11]. p. 405–16. Available from: /pmc/articles/PMC3141913/.
Guerra GCB, De Menezes MSS, De Araújo AA, De Araújo Júnior RF, De Medeiros CACX. Olmesartan prevented intra-articular inflammation induced by zymosan in rats. Biol Pharm Bull. Pharmaceutical Society of Japan. 2016;39:1793–801.
Araújo AA, Lopes De Souza G, Souza TO, De Castro Brito GA, Sabóia Aragão K, Xavier De Medeiros CA, et al. Olmesartan decreases IL-1β and TNF-α levels; Downregulates MMP-2, MMP-9, COX-2, and RANKL; And upregulates OPG in experimental periodontitis. Naunyn Schmiedebergs Arch Pharmacol [Internet]. Springer; 2013 [cited 2021 Apr 11];386:875–84. Available from: https://link.springer.com/article/10.1007/s00210-013-0886-8
Nagib MM, Tadros MG, Elsayed MI, Khalifa AE. Anti-inflammatory and anti-oxidant activities of olmesartan medoxomil ameliorate experimental colitis in rats. Toxicol Appl Pharmacol [Internet]. Toxicol Appl Pharmacol; 2013 [cited 2021 Apr 8];271:106–13. Available from: https://pubmed.ncbi.nlm.nih.gov/23665423/
Aziz MM, Abd El Fattah MA, Ahmed KA, Sayed HM. Protective effects of olmesartan and L-carnitine on doxorubicin-induced cardiotoxicity in rats. Can J Physiol Pharmacol [Internet]. Canadian Science Publishing; 2020 [cited 2021 Apr 11];98:183–93. Available from: https://pubmed.ncbi.nlm.nih.gov/31665614/
Sasidhar RLC, Vidyadhara S, Maheswari G V, Deepti B, Babu SP. Solubility and dissolution rate enhancement of olmesartan medoxomil by complexation and development of mouth dissolving tablets. Biol Res. 2013;7.
Burbure N, Lebwohl B, Arguelles-Grande C, Green PHR, Bhagat G, Lagana S. Olmesartan-associated sprue-like enteropathy: A systematic review with emphasis on histopathology. Hum Pathol [Internet]. W.B. Saunders; 2016 [cited 2021 Apr 19];50:127–34. Available from: https://pubmed.ncbi.nlm.nih.gov/26997446/
B. A, D. N, Veerabrahma K. Development of olmesartan medoxomil lipid-based nanoparticles and nanosuspension: preparation, characterization and comparative pharmacokinetic evaluation. Artif Cells, Nanomedicine, Biotechnol [Internet]. Taylor and Francis Ltd.; 2018 [cited 2021 Apr 19];46:126–37. Available from: https://www.tandfonline.com/doi/full/10.1080/21691401.2017.1299160
Arzani G, Haeri A, Daeihamed M, Bakhtiari-Kaboutaraki H, Dadashzadeh S. Niosomal carriers enhance oral bioavailability of carvedilol: effects of bile salt-enriched vesicles and carrier surface charge. Int J Nanomedicine Dove Medical Press. 2015;10:4797–813.
Ammar HO, Haider M, Ibrahim M, El Hoffy NM. In vitro and in vivo investigation for optimization of niosomal ability for sustainment and bioavailability enhancement of diltiazem after nasal administration. Drug Deliv Taylor & Francis. 2017;24:414–21.
Ullah S, Shah MR, Shoaib M, Imran M, Shah SWA, Ahmed F, et al. Hydrophilically modified self-assembling α-tocopherol derivative as niosomal nanocarrier for improving clarithromycin oral bioavailability. Artif Cells, Nanomedicine, Biotechnol. Taylor & Francis; 2018;46:568–78.
(17) Preparation and Characterization Techniques in Niosomal Vesicular Systems- A Review. | Request PDF [Internet]. [cited 2021 Apr 12]. Available from: https://www.researchgate.net/publication/304705141_Preparation_and_Characterization_Techniques_in_Niosomal_Vesicular_Systems-_A_Review
Song J, Yang X, Jacobson O, Lin L, Huang P, Niu G, et al. Sequential Drug Release and Enhanced Photothermal and Photoacoustic Effect of Hybrid Reduced Graphene Oxide-Loaded Ultrasmall Gold Nanorod Vesicles for Cancer Therapy. ACS Nano [Internet]. American Chemical Society; 2015 [cited 2021 Apr 12];9:9199–209. Available from: https://pubs.acs.org/doi/abs/10.1021/acsnano.5b03804
Yang L, Fassihi R. Accessibility of solid core tablet for dissolution in an asymmetric triple-layer matrix system. J Pharm Pharmacol [Internet]. Oxford University Press (OUP); 2010 [cited 2021 Apr 27];55:1331–7. Available from: https://academic.oup.com/jpp/article/55/10/1331/6148139
Liu Y, Schwartz JB, Schnaare RL, Sugita ET. A Multi-mechanistic Drug Release Approach in a Bead Dosage Form and In Vitro/In Vivo Correlations. Pharm Dev Technol [Internet]. 2003 [cited 2021 Apr 27];8:409–17. Available from: http://www.tandfonline.com/doi/full/10.1081/PDT-120024694
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C, et al. DDSolver: An add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010;12:263–71.
Xu X, Al-Ghabeish M, Krishnaiah YSR, Rahman Z, Khan MA. Kinetics of drug release from ointments: Role of transient-boundary layer. Int J Pharm Elsevier. 2015;494:31–9.
Singhvi G, Singh M. International Journal of Pharmaceutical Studies and Research REVIEW: IN-VITRO DRUG RELEASE CHARACTERIZATION MODELS. Int J Pharm Stud Res [Internet]. 2011 [cited 2021 Apr 29];2:77–84. Available from: https://www.researchgate.net/profile/Mahaveer-Singh-3/publication/285447890_Review_In_vitro_Drug_Release_Characterization_Models/links/606aceaea6fdccad3f71a806/Review-In-vitro-Drug-Release-Characterization-Models.pdf
Papadopoulou V, Kosmidis K, Vlachou M, Macheras P. On the use of the Weibull function for the discernment of drug release mechanisms. Int J Pharm [Internet]. Int J Pharm; 2006 [cited 2021 Apr 12];309:44–50. Available from: https://pubmed.ncbi.nlm.nih.gov/16376033/
Pratap Singh A, Siddiqui J, Diosady LL. Characterizing the pH-Dependent Release Kinetics of Food-Grade Spray Drying Encapsulated Iron Microcapsules for Food Fortification. Food Bioprocess Technol [Internet]. Springer New York LLC; 2018 [cited 2021 Apr 27];11:435–46. Available from: https://doi.org/10.1007/s11947-017-2022-0.
Lin CC, Metters AT. Hydrogels in controlled release formulations: Network design and mathematical modeling. Adv. Drug Deliv. Rev. 2006. p. 1379–408.
Kalam M, Humayun M, Parvez N, Yadav S. Release Kinetics of Modified Pharmaceutical Dosage Forms: a Review. Cont J Pharm Sci [Internet]. 2007;1:30–5. Available from: http://www.wiloludjournal.com/pdf/pharmsci/2007/30-35.pdf
Sathish R, Sahu A, Natarajan K. Antiulcer and antioxidant activity of ethanolic extract of Passiflora foetida L. Indian J Pharmacol [Internet]. Medknow Publications and Media Pvt. Ltd.; 2011 [cited 2021 Apr 12];43:336–9. Available from: http://www.ijp-online.com/text.asp?2011/43/3/336/81501
Hamdan DI, El-Shiekh RA, El-Sayed MA, Khalil HMA, Mousa MR, Al-Gendy AA, et al. Phytochemical characterization and anti-inflammatory potential of Egyptian Murcott mandarin cultivar waste (stem, leaves and peel). Food Funct [Internet]. Royal Society of Chemistry; 2020 [cited 2021 Apr 12];11:8214–36. Available from: https://pubs.rsc.org/en/content/articlehtml/2020/fo/d0fo01796e
Beutler E, Duron O, Kelly BM. Improved method for the determination of blood glutathione. J Lab Clin Med [Internet]. 1963 [cited 2021 Apr 12];61:882–8. Available from: https://pubmed.ncbi.nlm.nih.gov/13967893/
Tateishi T, Yoshimine N, Kuzuya F. Serum lipid peroxide assayed by a new colorimetric method. Exp Gerontol. 1987;22:103–11.
Nishikimi M, Appaji Rao N, Yagi K. The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochem Biophys Res Commun [Internet]. Biochem Biophys Res Commun; 1972 [cited 2021 Apr 12];46:849–54. Available from: https://pubmed.ncbi.nlm.nih.gov/4400444/
Schacht V, Kern JS. Basics of immunohistochemistry. J Invest Dermatol [Internet]. Nature Publishing Group; 2015 [cited 2021 Apr 12];135:e30. Available from: https://pubmed.ncbi.nlm.nih.gov/25666678/
Kamboj S, Saini V, Bala S. Formulation and characterization of drug loaded nonionic surfactant vesicles (Niosomes) for oral bioavailability enhancement. Sci World J 2014;2014.
Badran M, Arabia S. [PDF] FORMULATION AND IN VITRO EVALUATION OF FLUFENAMIC ACID LOADED DEFORMABLE LIPOSOMES FOR IMPROVED SKIN DELIVERY | Semantic Scholar [Internet]. undefined. 2014 [cited 2021 Apr 20]. Available from: https://www.semanticscholar.org/paper/FORMULATION-AND-IN-VITRO-EVALUATION-OF-FLUFENAMIC-Badran-Arabia/d0091db01b013d48a58baefde339b17f6a4a7e0a
Chen M, Liu X, Fahr A. Skin penetration and deposition of carboxyfluorescein and temoporfin from different lipid vesicular systems: In vitro study with finite and infinite dosage application. Int J Pharm [Internet]. Int J Pharm; 2011 [cited 2021 Apr 20];408:223–34. Available from: https://pubmed.ncbi.nlm.nih.gov/21316430/
Putri DCA, Dwiastuti R, Marchaban M, Nugroho AK. OPTIMIZATION OF MIXING TEMPERATURE AND SONICATION DURATION IN LIPOSOME PREPARATION. J Pharm Sci Community [Internet]. Sanata Dharma University; 2017 [cited 2021 Apr 20];14:79–85. Available from: https://doi.org/10.24071/jpsc.142728
Kulkarni P, Rawtani D. Application of Box-Behnken Design in the Preparation, Optimization, and In Vitro Evaluation of Self-Assembly–Based Tamoxifen- and Doxorubicin-Loaded and Dual Drug–Loaded Niosomes for Combinatorial Breast Cancer Treatment. J Pharm Sci [Internet]. Elsevier B.V.; 2019 [cited 2021 Apr 20];108:2643–53. Available from: https://pubmed.ncbi.nlm.nih.gov/30905701/
Nasseri B. Effect of cholesterol and temperature on the elastic properties of niosomal membranes. Int J Pharm [Internet]. 2005 [cited 2021 Apr 20];300:95–101. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0378517305003170
Liu T, Guo R, Hua W, Qiu J. Structure behaviors of hemoglobin in PEG 6000/Tween 80/Span 80/H2O niosome system. Colloids Surfaces A Physicochem Eng Asp. Elsevier; 2007;293:255–61.
Liu DZ, Chen WY, Tasi LM, Yang SP. Microcalorimetric and shear studies on the effects of cholesterol on the physical stability of lipid vesicles. Colloids Surfaces A Physicochem Eng Asp [Internet]. Elsevier; 2000 [cited 2021 Apr 20];172:57–67. Available from: https://tmu.pure.elsevier.com/en/publications/microcalorimetric-and-shear-studies-on-the-effects-of-cholesterol
Li D. Development and Evaluation of a Niosome Carrier for Topical Use of Antioxidant. 2014;
Sezgin-Bayindir Z, Antep MN, Yuksel N. Development and Characterization of Mixed Niosomes for Oral Delivery Using Candesartan Cilexetil as a Model Poorly Water-Soluble Drug. AAPS PharmSciTech [Internet]. Springer New York LLC; 2014 [cited 2021 Apr 20];16:108–17. Available from: /pmc/articles/PMC4309817/.
Malfertheiner P, Chan FK, McColl K EL. Peptic ulcer disease [Internet]. Lancet. Elsevier B.V.; 2009 [cited 2021 Apr 20]. p. 1449–61. Available from: https://pubmed.ncbi.nlm.nih.gov/19683340/
Fiorucci S, Antonelli E, Morelli A. Mechanism of non-steroidal anti-inflammatory drug-gastropathy [Internet]. Dig. Liver Dis. Pacini Editore s.r.l.; 2001 [cited 2021 Apr 20]. Available from: https://pubmed.ncbi.nlm.nih.gov/11827361/
Pozzoli C, Menozzi A, Grandi D, Solenghi E, Ossiprandi MC, Zullian C, et al. Protective effects of proton pump inhibitors against indomethacin-induced lesions in the rat small intestine. Springer [Internet]. [cited 2021 Apr 8]; Available from: https://link.springer.com/content/pdf/10.1007/s00210-006-0121-y.pdf
Luo C, Chen H, Wang Y, Lin G, Li C, Tan L, et al. Protective effect of coptisine free base on indomethacin-induced gastric ulcers in rats: Characterization of potential molecular mechanisms. Life Sci [Internet]. 2018 [cited 2021 Apr 8];193:47–56. Available from: https://www.sciencedirect.com/science/article/pii/S0024320517306318
Ricciotti E, Fitzgerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol [Internet]. NIH Public Access; 2011 [cited 2021 Apr 20];31:986–1000. Available from: /pmc/articles/PMC3081099/.
Wallace JL. Pathogenesis of NSAID-induced gastroduodenal mucosal injury. Best Pract Res Clin Gastroenterol [Internet]. Bailliere Tindall Ltd; 2001 [cited 2021 Apr 20];15:691–703. Available from: https://pubmed.ncbi.nlm.nih.gov/11566035/
Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE. Oxidative stress: An essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol Rev [Internet]. American Physiological Society; 2014 [cited 2021 Apr 20];94:329–54. Available from: https://pubmed.ncbi.nlm.nih.gov/24692350/
Chattopadhyay S, Adhikary B, Yadav SK, Roy K, Bandyopadhyay SK. Black tea and theaflavins assist healing of indomethacin-induced gastric ulceration in mice by antioxidative action. Evidence-based Complement Altern Med [Internet]. Hindawi Limited; 2011 [cited 2021 Apr 20];2011:11. Available from: /pmc/articles/PMC2952312/.
Pérez S, Taléns-Visconti R, Rius-Pérez S, Finamor I, Sastre J. Redox signaling in the gastrointestinal tract. Free Radic. Biol. Med. Elsevier Inc.; 2017. p. 75–103.
Ighodaro OM, Akinloye OA. First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): Their fundamental role in the entire antioxidant defence grid. Alexandria J Med Informa UK Limited. 2018;54:287–93.
Circu ML, Aw TY. Intestinal redox biology and oxidative stress. Semin. Cell Dev. Biol. Elsevier Ltd; 2012. p. 729–37.
Aziz RS, Siddiqua A, Shahzad M, Shabbir A, Naseem N. Oxyresveratrol ameliorates ethanol-induced gastric ulcer via downregulation of IL-6, TNF-α NF-ĸB, and COX-2 levels, and upregulation of TFF-2 levels. Biomed Pharmacother [Internet]. Elsevier Masson SAS; 2019 [cited 2021 Apr 20];110:554–60. Available from: https://pubmed.ncbi.nlm.nih.gov/30530291/
Chauhan I, Agrawal S, Goel RK. Status of inflammatory markers and growth factor in gastric ulcer protective effects of Punica granatum L. peel extract in rat. Natl J Physiol Pharm Pharmacol [Internet]. 2018 [cited 2021 Apr 20];12. Available from: www.njppp.com
Bak MJ, Truong VL, Ko SY, Nguyen XNG, Jun M, Hong SG, et al. Induction of Nrf2/ARE-mediated cytoprotective genes by red ginseng oil through ASK1–MKK4/7E–JNK and p38 MAPK signaling pathways in HepG2 cells. J Ginseng Res [Internet]. Elsevier B.V.; 2016 [cited 2021 Apr 25];40:423–30. Available from: /pmc/articles/PMC5052443/.
Wong SY, Tan MGK, Wong PTH, Herr DR, Lai MKP. Andrographolide induces Nrf2 and heme oxygenase 1 in astrocytes by activating p38 MAPK and ERK. J Neuroinflammation [Internet]. BioMed Central Ltd.; 2016 [cited 2021 Apr 22];13:251. Available from: http://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-016-0723-3
Chaparro-Huerta V, Flores-Soto ME, Gudiño-Cabrera G, Rivera-Cervantes MC, Bitzer-Quintero OK, Beas-Zárate C. Role of p38 MAPK and pro-inflammatory cytokines expression in glutamate-induced neuronal death of neonatal rats. Int J Dev Neurosci [Internet]. Int J Dev Neurosci; 2008 [cited 2021 Apr 25];26:487–95. Available from: https://pubmed.ncbi.nlm.nih.gov/18396383/
Kaminska B. MAPK signalling pathways as molecular targets for anti-inflammatory therapy - From molecular mechanisms to therapeutic benefits. Biochim Biophys Acta - Proteins Proteomics. Elsevier; 2005. p. 253–62.
Carrozzino F, Pugnale P, Féraille E, Montesano R. Inhibition of basal p38 or JNK activity enhances epithelial barrier function through differential modulation of claudin expression. Am J Physiol - Cell Physiol [Internet]. Am J Physiol Cell Physiol; 2009 [cited 2021 Apr 25];297. Available from: https://pubmed.ncbi.nlm.nih.gov/19605737/
Zhang Z, Zhang Q, Li F, Xin Y, Duan Z. Contributions of ho-1-dependent mapk to regulating intestinal barrier disruption. Biomol Ther [Internet]. Korean Society of Applied Pharmacology; 2021 [cited 2021 Apr 25];29:175–83. Available from: /pmc/articles/PMC7921856/.
Mazumder S, De R, Debsharma S, Bindu S, Maity P, Sarkar S, et al. Indomethacin impairs mitochondrial dynamics by activating the PKCζ-p38-DRP1 pathway and inducing apoptosis in gastric cancer and normal mucosal cells. J Biol Chem [Internet]. American Society for Biochemistry and Molecular Biology Inc.; 2019 [cited 2021 Apr 25];294:8238–58. Available from: https://pubmed.ncbi.nlm.nih.gov/30940726/
Luo C, Chen H, Wang Y, Lin G, Li C, Tan L, et al. Protective effect of coptisine free base on indomethacin-induced gastric ulcers in rats: Characterization of potential molecular mechanisms. Life Sci [Internet]. Elsevier Inc.; 2018 [cited 2021 Apr 25];193:47–56. Available from: https://pubmed.ncbi.nlm.nih.gov/29223540/
Saha S, Buttari B, Panieri E, Profumo E, Saso L. An Overview of Nrf2 Signaling Pathway and Its Role in Inflammation. Molecules. 2020;25:1–31.
Puentes-Pardo JD, Moreno-Sanjuan S, Carazo Á, León J. Heme oxygenase-1 in gastrointestinal tract health and disease. Antioxidants. 2020;9:1–30.
Soares MP, Bach FH. Heme oxygenase-1: from biology to therapeutic potential. Trends Mol Med [Internet]. Trends Mol Med; 2009 [cited 2021 Apr 25];15:50–8. Available from: https://pubmed.ncbi.nlm.nih.gov/19162549/
Yanaka A. Role of NRF2 in protection of the gastrointestinal tract against oxidative stress [Internet]. J. Clin. Biochem. Nutr. The Society for Free Radical Research Japan; 2018 [cited 2021 Apr 25]. p. 18–25. Available from: /pmc/articles/PMC6064821/.
Staurengo-Ferrari L, Badaro-Garcia S, Hohmann MSN, Manchope MF, Zaninelli TH, Casagrande R, et al. Contribution of Nrf2 modulation to the mechanism of action of analgesic and anti-inflammatory drugs in pre-clinical and clinical stages [Internet]. Front. Pharmacol. Frontiers Media S.A.; 2019 [cited 2021 Apr 25]. Available from: /pmc/articles/PMC6337248/
Smirnova LE. K probleme komorbidnosti iazvenno-érozivnykh porazhenii gastroduodenal’noi zony i arterial’noi gipertonii. [Internet]. Klin. Med. (Mosk). Klin Med (Mosk); 2003 [cited 2021 Oct 7]. p. 9–15. Available from: https://pubmed.ncbi.nlm.nih.gov/12698842/
Author information
Authors and Affiliations
Contributions
Al-Aliaa M. Sallam-Alia.sallam@pharma.asu.edu.eg-Writing - Original Draft, Resources, Methodology, Validation, Conceptualization
Samar F. Darwish-Samar.fathy@buc.edu.eg-Supervision, Writing - Review & Editing, Formal analysis, Investigation, Software, Visualization
Walaa A. El-Dakroury-w_dakroury@yahoo.com-Visualization, Writing - Original Draft, Formal analysis, Investigation, Software
Eman Radwan-Emanradwan@aun.edu.eg-Data Curation, Methodology, Conceptualization
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sallam, AA.M., Darwish, S.F., El-Dakroury, W.A. et al. Olmesartan niosomes ameliorates the Indomethacin-induced gastric ulcer in rats: Insights on MAPK and Nrf2/HO-1 signaling pathway. Pharm Res 38, 1821–1838 (2021). https://doi.org/10.1007/s11095-021-03126-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-021-03126-5