Abstract
Purpose
To use physiologically-based pharmacokinetic (PBPK) modelling to explore the food effect of different DNX hydrobromide (HBr) hemihydrate salt tablet formulations using biorelevant dissolution.
Methods
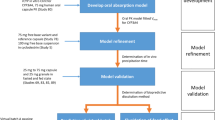
Compendial dissolution using a paddle method and TIM-1 biorelevant dissolution were performed and incorporated into a previously reported PBPK model. A two-part clinical study evaluated tablet formulations in the fasted/fed (high fat) state (Part A), and the impact of food (fasted/normal/high fat) and Proton Pump Inhibitor (PPI) co-administration for a selected formulation; as well as a formulation containing DNX HBr in the monohydrate state (Part B).
Results
TIM-1 data showed that the fed state bioaccessibility of DNX was significantly decreased compared to the fasted state with no significant differences between formulations. Dosed with normal/high fat food the selected formulation showed comparable exposure and a modest increase in DNX systemic PK was observed with PPI dependent on meal type. Under fed conditions DNX systemic exposure was comparable for the monohydrate and hemihydrate formulations. The integration of biorelevant TIM-1 data into the PBPK model led to the successful simulation of a DNX negative food effect.
Conclusions
Interactions between DNX and food components are the likely the source of the negative food effect via micellar entrapment, ion pairing and/or meal induced viscosity changes.






Similar content being viewed by others
Data Availability
Anonymized individual participant data and study documents can be requested for further research from www.clinicalstudydatarequest.com
Abbreviations
- API:
-
Active pharmaceutical ingredient
- AUC:
-
Area under the curve
- Cmax :
-
Maximum blood concentration
- CI:
-
Confidence interval
- DC:
-
Direct compression
- DNX:
-
Danirixin
- FaSSIF:
-
Fasted state simulated intestinal fluid
- FB:
-
Free base
- FeSSIF:
-
Fed state simulated intestinal fluid
- HBr:
-
Hydrobromide
- HPLC:
-
High performance liquid chromatography
- HPMC:
-
Hydroxypropyl methylcellulose
- OMP:
-
Omeprazole
- PBPK:
-
Physiologically-based pharmacokinetic
- PK:
-
Pharmacokinetic
- PPI:
-
Proton pump inhibitor
- RC:
-
Roller compaction
- SD:
-
Standard deviation
- SGF:
-
Simulated gastric fluid
- TIM-1:
-
TNO/Triskelion intestinal model 1
- tmax :
-
Time of occurrence of maximum blood concentration
References
Busch-Petersen J, Carpenter DC, Burman M, Foley J, Hunsberger GE, Kilian DJ, et al. Danirixin: a reversible and selective antagonist of the CXC chemokine receptor 2. J Pharmacol Exp Ther. 2017;362(2):338–46.
Lazaar AL, Miller BE, Tabberer M, Yonchuk J, Leidy N, Ambery C, et al. Effect of the CXCR2 antagonist danirixin on symptoms and health status in COPD. Eur Respir J. 2018;52(4):1801020.
Bloomer JC, Ambery C, Miller BE, Connolly P, Garden H, Henley N, et al. Identification and characterisation of a salt form of Danirixin with reduced pharmacokinetic variability in patient populations. Eur J Pharm Biopharm. 2017;117:224–31.
Food and Drug Administration. Guidance for industry: food-effect bioavailability and fed bioequivalence studies. US Department of Health and Human Services, Rockville, MD.; 29 November 2018.
Dickinson PA, Abu Rmaileh R, Ashworth L, Barker RA, Burke WM, Patterson CM, et al. An investigation into the utility of a multi-compartmental, dynamic, system of the upper gastrointestinal tract to support formulation development and establish bioequivalence of poorly soluble drugs. AAPS J. 2012;14(2):196–205.
Blanquet S, Zeijdner E, Beyssac E, Meunier J-P, Denis S, Havenaar R, et al. A dynamic artificial gastrointestinal system for studying the behavior of orally administered drug dosage forms under various physiological conditions. Pharm Res. 2004;21(4):585–91.
Miller BE, Mistry S, Smart K, Connolly P, Carpenter DC, Cooray H, Bloomer JC, Tal-Singer R, Lazaar AL. The pharmacokinetics and pharmacodynamics of danirixin (GSK1325756) - a selective CXCR2 antagonist - in healthy adult subjects. BMC Pharmacology and Toxicology. 2015;16(1).
Johnson MA, Wilfret D, Chen S, Jones L, Bloomer J, Peat A. First time single and repeated dose IV administration and absolute bioavailability of a novel CXCR2 antagonist, GSK1325756 (Danirixin); study NCT02169583. San Diego, California, USA: In.Interscience Conference on Antimicrobial Agents; 2015.
Iida T, Matsuzawa Y, Ogura H, Nagakubo T, Wakamatsu A, Ambery C, Miller BE, Lazaar AL, Numachi Y. Evaluation of the Safety, Tolerability, Pharmacokinetics, and Food Effect of Danirixin Hydrobromide Tablets in Japanese Healthy Elderly Participants. Clinical Pharmacology in Drug Development;0(0).
Heinen CA, Reuss S, Amidon GL, Langguth P. Ion pairing with bile salts modulates intestinal permeability and contributes to food-drug interaction of BCS class III compound trospium chloride. Mol Pharm. 2013;10(11):3989–96.
Rubbens J, Brouwers J, Tack J, Augustijns P. Gastrointestinal dissolution, supersaturation and precipitation of the weak base indinavir in healthy volunteers. Eur J Pharm Biopharm. 2016;109:122–9.
Radwan A, Amidon GL, Langguth P. Mechanistic investigation of food effect on disintegration and dissolution of BCS class III compound solid formulations: the importance of viscosity. Biopharm Drug Dispos. 2012;33(7):403–16.
Abuhelwa AY, Williams DB, Upton RN, Foster DJR. Food, gastrointestinal pH, and models of oral drug absorption. Eur J Pharm Biopharm. 2017;112:234–48.
Li M, Zhao P, Pan Y, Wagner C. Predictive performance of physiologically based pharmacokinetic models for the effect of food on Oral drug absorption: current status. CPT Pharmacometrics Syst Pharmacol. 2018;7(2):82–9.
Tistaert C, Heimbach T, Xia B, Parrott N, Samant TS, Kesisoglou F. Food effect projections via physiologically based pharmacokinetic modeling: predictive case studies. J Pharm Sci. 2018.
Lau YY, Gu W, Lin T, Song D, Yu R, Scott JW. Effects of meal type on the oral bioavailability of the ALK inhibitor ceritinib in healthy adult subjects. J Clin Pharmacol. 2016;56(5):559–66.
Sutton SC, Nause R, Gandelman K. The impact of gastric pH, volume, and emptying on the food effect of ziprasidone oral absorption. AAPS J. 2017;19(4):1084–90.
Andreas CJ, Pepin X, Markopoulos C, Vertzoni M, Reppas C, Dressman JB. Mechanistic investigation of the negative food effect of modified release zolpidem. Eur J Pharm Sci. 2017;102:284–98.
O'Shea JP, Holm R, O'Driscoll CM, Griffin BT. Food for thought: formulating away the food effect – a PEARRL review. J Pharm Pharmacol. 2019;71(4):510–35.
Grimm M, Scholz E, Koziolek M, Kühn J-P, Weitschies W. Gastric water emptying under fed state clinical trial conditions is as fast as under fasted conditions. Mol Pharm. 2017;14(12):4262–71.
Cvijić S, Parojčić J, Langguth P. Viscosity-mediated negative food effect on oral absorption of poorly-permeable drugs with an absorption window in the proximal intestine: in vitro experimental simulation and computational verification. Eur J Pharm Sci. 2014;61(1):40–53.
Kawai Y, Fujii Y, Tabata F, Ito J, Metsugi Y, Kameda A, et al. Profiling and trend analysis of food effects on Oral drug absorption considering micelle interaction and Solubilization by bile micelles. Drug Metabolism and Pharmacokinetics. 2011;26(2):180–91.
ACKNOWLEDGEMENTS AND DISCLOSURES
The authors would like to thank the staff of Quintiles, Inc. and, most importantly, the volunteers for their participation in the clinical study which was funded by GlaxoSmithKline (ClinicalTrials.gov identifier NCT03457727). The authors would also like to thank the staff of Pozlab sp. z o.o for performing the in-vitro TIM experiments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
RSL reports employment and shareholder status at GlaxoSmithKline; MIH reports former employment and shareholder status at GlaxoSmithKline; SJC former employment status, pension and shareholder status at GlaxoSmithKline; AP reports employment and shareholder status at GlaxoSmithKline; JCB reports employment and shareholder status at GlaxoSmithKline; XZ reports employment and shareholder status at GlaxoSmithKline; BM reports employment and shareholder status at GlaxoSmithKline; DD reports former employment and shareholder status at GlaxoSmithKline; AD reports employment and shareholder status at GlaxoSmithKline; RTS reports former employment and shareholder status at GlaxoSmithKline; CA reports employment and shareholder status at GlaxoSmithKline.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 280 kb)
Rights and permissions
About this article
Cite this article
Lloyd, R.S., Hingle, M.I., Bloomer, J.C. et al. Negative Food Effect of Danirixin: Use of PBPK Modelling to Explore the Effect of Formulation and Meal Type on Clinical PK. Pharm Res 37, 233 (2020). https://doi.org/10.1007/s11095-020-02948-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02948-z