Abstract
Purpose
The objective of this study was to optimize nose-to-lung aerosol delivery in an adult upper airway model using computational fluid dynamics (CFD) simulations in order to guide subsequent human subject aerosol delivery experiments.
Methods
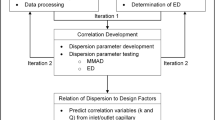
A CFD model was developed that included a new high-flow nasal cannula (HFNC) and pharmaceutical aerosol delivery unit, nasal cannula interface, and adult upper airway geometry. Aerosol deposition predictions in the system were validated with existing and new experimental results. The validated CFD model was then used to explore aerosol delivery parameters related to synchronizing aerosol generation with inhalation and inhalation flow rate.
Results
The low volume of the new HFNC unit minimized aerosol transit time (0.2 s) and aerosol bolus spread (0.1 s) enabling effective synchronization of aerosol generation with inhalation. For aerosol delivery correctly synchronized with inhalation, a small particle excipient-enhanced growth delivery strategy reduced nasal cannula and nasal depositional losses each by an order of magnitude and enabled ~80% of the nebulized dose to reach the lungs. Surprisingly, nasal deposition was not sensitive to inhalation flow rate due to use of a nasal cannula interface with co-flow inhaled air and the small initial particle size.
Conclusions
The combination of correct aerosol synchronization and small particle size enabled high efficiency nose-to-lung aerosol delivery in adults, which was not sensitive to inhalation flow rate.











Similar content being viewed by others
Abbreviations
- ACI:
-
Andersen Cascade Impactor
- AS:
-
Albuterol sulfate
- CFD:
-
Computational Fluid Dynamics
- DE:
-
Deposition efficiency
- DF:
-
Deposition fraction
- EEG:
-
Excipient enhanced growth
- FE:
-
Fraction exhaled
- FR:
-
Fraction remaining
- GCI:
-
Grid convergence index
- HFNC:
-
High flow nasal cannula
- HPLC:
-
High performance liquid chromatography
- LPM:
-
Liters per minute
- LRN:
-
Low Reynolds number
- MMAD:
-
Mass median aerodynamic diameter
- NaCl:
-
sodium chloride
- NIV:
-
Non-invasive ventilation
- NMT:
-
Nose-mouth-throat
- NW:
-
Near-wall
- PF:
-
Penetration fraction
- RANS:
-
Reynolds averaged Navier-Stokes
- RH:
-
Relative humidity
- TB:
-
Tracheobronchial
- UDF:
-
User defined function
References
Bhashyam AR, Wolf MT, Marcinkowski AL, Saville A, Thomas K, Carcillo JA, et al. Aerosol delivery through nasal cannulas: an in vitro study. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2008;21:181–7.
Longest PW, Golshahi L, Behara SRB, Tian G, Farkas DR, Hindle M. Efficient nose-to-lung (N2L) aerosol delivery with a dry powder inhaler. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2015;28:189–201.
Farkas D, Hindle M, Longest PW. Application of an inline dry powder inhaler to deliver high dose pharmaceutical aerosols during low flow nasal cannula therapy. Int J Pharm. 2018;546:1–9.
Hess DR. Aerosol therapy during noninvasive ventilation or high-flow nasal cannula. Respir Care. 2015;60:880–93.
Dhand R. Aerosol therapy in patients receiving noninvasive positive pressure ventilation. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2012;25:63–78.
Farkas D, Hindle M, Longest PW. Application of an inline dry powder inhaler to deliver high dose pharmaceutical aerosols during low flow nasal cannula therapy. Int J Pharm. 2018;546:1–9. https://doi.org/10.1016/j.ijpharm.2018.05.011.
Rubin BK. Pediatric aerosol therapy: new devices and new drugs. Respir Care. 2011;56:1411–21.
Laube BL. Aerosolized medications for gene and peptide therapy. Respir Care. 2015;60:806–24.
Dixon AE. Rhinosinusitis and asthma: the missing link. Curr Opin Pulm Med. 2009;15:19–24.
Aanæs K. Bacterial sinusitis can be a focus for initial lung colonisation and chronic lung infection in patients with cystic fibrosis. J Cyst Fibros. 2013;12:S1–S20.
Zeman KL, Rojas Balcazar J, Fuller F, Donn KH, Boucher RC, Bennett WD, et al. A trans-nasal aerosol delivery device for efficient pulmonary deposition. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2017;30:223–9.
Geller DE. Aerosol antibiotics in cystic fibrosis. Respir Care. 2009;54:658–70.
Spence BM, Longest PW, Wei X, Dhapare S, and Hindle M. Development of a high flow nasal cannula (HFNC) and pharmaceutical aerosol combination device. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2019; https://doi.org/10.1089/jamp.2018.1488
Rubin BK, Fink JB. Aerosol therapy for children. Respir Care Clin N Am. 2001;7:175–213.
Devadason SG. Recent advances in aerosol therapy for children with asthma. Journal of Aerosol Medicine-Deposition Clearance and Effects in the Lung. 2006;19:61–6.
Perry SA, Kesser KC, Geller DE, Selhorst DM, Rendle JK, Hertzog JH. Influences of cannula size and flow rate on aerosol drug delivery through the Vapotherm humidified high-flow nasal cannula system. Pediatr Crit Care Med. 2013;14:E250–6.
Bennett G, Joyce M, Sweeney L, MacLoughlin R. In vitro determination of the main effects in the design of high-flow nasal therapy systems with respect to aerosol performance. Pulmonary Therapy. 2018;4:73–86. https://doi.org/10.1007/s41030-018-0054-x:1-14.
DiBlasi RM. Clinical controversies in aerosol therapy for infants and children. Respir Care. 2015;60:894–916.
Ward JJ. High-flow oxygen administration by nasal cannula for adult and perinatal patients. Respir Care. 2013;58:98–120.
Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care. 2015;3:15.
Dysart K, Miller TL, Wolfson MR, Shaffer TH. Research in high flow therapy: mechanisms of action. Respir Med. 2009;103:1400–5.
Golshahi L, Longest PW, Azimi M, Syed A, Hindle M. Intermittent aerosol delivery to the lungs during high flow nasal cannula therapy. Respir Care. 2014;59:1476–86.
Golshahi L, Tian G, Azimi M, Son Y-J, Walenga RL, Longest PW, et al. The use of condensational growth methods for efficient drug delivery to the lungs during noninvasive ventilation high flow therapy. Pharm Res. 2013;30:2917–30.
Reminiac F, Vecellio L, Heuze-Vourc'h N, Petitcollin A, Respaud R, Cabrera M, Le Pennec D, Diot P, and Ehrmann S. Aerosol therapy in adults receiving high flow nasal cannula oxygen therapy. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2016; https://doi.org/10.1089/jamp.2015.1219
Dailey PA, Harwood R, Walsh K, Fink JB, Thayer T, Gagnon G, et al. Aerosol delivery through adult high flow nasal cannula with heliox and oxygen. Respir Care. 2018;62:1186–92.
Hess DR. The mask of noninvasive ventilation: principles of design and effects on aerosol delivery. Journal of Aerosol Medicine. 2007;20:S85–99.
Dhand R. Inhalation therapy in invasive and noninvasive mechanical ventilation. Curr Opin Crit Care. 2007;13:27–38.
Ari A, Fink JB. Inhalation therapy in patients receiving mechanical ventilation: an update. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2012;25:319–32.
Dugernier J, Hesse M, Jumetz T, Bialais E, Roeseler J, Depoortere V, et al. Aerosol delivery with two nebulizers through high-flow nasal cannula: a randomized cross-over single-photon emission computed tomography study. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2017;30:349–58.
Bräunlich J, Wirtz H. Oral versus nasal high-flow bronchodilator inhalation in chronic obstructive pulmonary disease. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2018;31:248–54.
Borgstrom L, Olsson B, Thorsson L. Degree of throat deposition can explain the variability in lung deposition of inhaled drugs. Journal of Aerosol Medicine. 2006;19:473–83.
Walenga RL, Longest PW, Kaviratna A, Hindle M. Aerosol drug delivery during noninvasive positive pressure ventilation: effects of intersubject variability and excipient enhanced growth. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2017;30:190–205.
Weers J. Inhaled antimicrobial therapy - barriers to effective treatment. Adv Drug Deliv Rev. 2015;85:24–43.
Barnes PJ. New anti-inflammatory targets for chronic obstructive pulmonary disease. Nat Rev Drug Discov. 2013;12:543–59.
Barnes PJ. Development of new drugs for COPD. Curr Med Chem. 2013;20:1531–40.
Longest PW, Walenga RL, Son Y-J, Hindle M. High efficiency generation and delivery of aerosols through nasal cannula during noninvasive ventilation. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2013;26:266–79.
Longest PW, Golshahi L, Hindle M. Improving pharmaceutical aerosol delivery during noninvasive ventilation: effects of streamlined components. Ann Biomed Eng. 2013;41:1217–32.
Longest PW, and Hindle M. Systems, devices, and methods for changing therapeutic aeorsol size and improving efficiency of ventilation and aerosol drug delivery. US Patent 10,010,692 B2. 2018;
Golshahi L, Walenga RL, Longest PW, Hindle M. Development of a transient flow aersol mixer-heater system for lung delivery of nasally administered aerosols using a nasal cannula. Aerosol Sci Technol. 2014;48:1009–21.
Schuster J, Rubsamen R, Lloyd P, Lloyd J. The AERx™ aerosol delivery system. Pharm Res. 1997;14:354–7.
Denyer J, Nikander K, Smith N. Adaptive aerosol delivery (AAD®) technology. Expert Opin Drug Deliv. 2004;1:165–76.
Longest PW, and Hindle M. Improved delivery of submicrometer and nanometer aerosols to the lungs using hygroscopic excipients or dual stream nasal delivery. US Patent No. 9,433,588 B2. 2016;
Longest PW, Hindle M, Xi J. Enhanced delivery of nano- and micro-sized pharmaceutical aerosols through controlled hygroscopic growth. US Patent. 2013;8:479,728.
Longest PW, Hindle M. Numerical model to characterize the size increase of combination drug and hygroscopic excipient nanoparticle aerosols. Aerosol Sci Technol. 2011;45:884–99.
Hindle M, Longest PW. Condensational growth of combination drug-excipient submicrometer particles for targeted high efficiency pulmonary delivery: evaluation of formulation and delivery device. J Pharm Pharmacol. 2012;64:1254–63.
Hindle M, Longest PW. Evaluation of enhanced condensational growth (ECG) for controlled respiratory drug delivery in a mouth-throat and upper tracheobronchial model. Pharm Res. 2010;27:1800–11.
Longest PW, Tian G, Li X, Son Y-J, Hindle M. Performance of combination drug and hygroscopic excipient submicrometer particles from a softmist inhaler in a characteristic model of the airways. Ann Biomed Eng. 2012;40:2596–610.
Son Y-J, Longest PW, Tian G, Hindle M. Evaluation and modification of commercial dry powder inhalers for the aerosolization of submicrometer excipient enhanced growth (EEG) formulation. Eur J Pharm Sci. 2013;49:390–9.
Tian G, Hindle M, Longest PW. Targeted lung delivery of nasally administered aerosols. Aerosol Sci Technol. 2014;48:434–49.
Tian G, Longest PW, Li X, Hindle M. Targeting aerosol deposition to and within the lung airways using excipient enhanced growth. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2013;26:248–65.
Longest PW, Hindle M. Condensational growth of combination drug-excipient submicrometer particles: comparison of CFD predictions with experimental results. Pharm Res. 2012;29:707–21.
Kim CS, Jaques PA. Respiratory dose of inhaled ultrafine particles in healthy adults. Philosophical Transactions Of The Royal Society Of London Series A-Mathematical Physical And Engineering Sciences. 2000;358:2693–705.
Walenga RL, Tian G, Hindle M, Yelverton J, Dodson K, Longest PW. Variability in nose-to-lung aerosol delivery. J Aerosol Sci. 2014;78:11–29.
Longest PW, Tian G, and Hindle M. Improving the lung delivery of nasally administered aerosols during noninvasive ventilation - An application of enhanced condensational growth (ECG). Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2011;24:103–118, DOI: 1https://doi.org/10.1089/jamp.2010.0849.
Franca EET, de Andrade AFD, Cabral G, Almeida P, Silva KC, Galindo VC, et al. Nebulization associated with bi-level noninvasive ventilation: analysis of pulmonary radioaerosol deposition. Respir Med. 2006;100:721–8.
ICRP. Human respiratory tract model for radiological protection. New York: Elsevier Science Ltd.; 1994.
Delvadia RR, Longest PW, Hindle M, Byron PR. In vitro tests for aerosol deposition. III: effect of inhaler insertion angle on aerosol deposition. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2013;26:145–56.
Longest PW, Hindle M, Das Choudhuri S, Byron PR. Numerical simulations of capillary aerosol generation: CFD model development and comparisons with experimental data. Aerosol Sci Technol. 2007;41:952–73.
Longest PW, Xi J. Condensational growth may contribute to the enhanced deposition of cigarette smoke particles in the upper respiratory tract. Aerosol Sci Technol. 2008;42:579–602.
Gosman AD, Ioannides E. Aspects of computer simulation of liquid-fueled combustors. Journal of Energy. 1981;7:482–90.
Matida EA, Finlay WH, Grgic LB. Improved numerical simulation of aerosol deposition in an idealized mouth-throat. J Aerosol Sci. 2004;35:1–19.
Wang Y, James PW. On the effect of anisotropy on the turbulent dispersion and deposition of small particles. Int J Multiphase Flow. 1999;22:551–8.
Longest PW, Xi J. Effectiveness of direct Lagrangian tracking models for simulating nanoparticle deposition in the upper airways. Aerosol Sci Technol. 2007;41:380–97.
Longest PW, Kleinstreuer C, Buchanan JR. Efficient computation of micro-particle dynamics including wall effects. Comput Fluids. 2004;33:577–601.
Bass K, Longest PW. Recommendations for simulating microparticle deposition at conditions similar to the upper airways with two-equation turbulence models. J Aerosol Sci. 2018;119:31–50. https://doi.org/10.1016/j.jaerosci.2018.02.007.
Horsfield K, Dart G, Olson DE, Cumming G. Models of the human bronchial tree. J Appl Physiol. 1971;31:207–17.
Asgharian B, Price OT. Airflow distribution in the human lung and its influence on particle deposition. Inhal Toxicol. 2006;18:795–801.
Walenga RL, Tian G, Longest PW. Development of characteristic upper tracheobronchial airway models for testing pharmaceutical aerosol delivery. ASME Journal of Biomechanical Engineering. 2013;135(9):091010.
Bennett G, Joyce M, Sweeney L, MacLoughlin R. In vitro study of the effect of breathing pattern on aerosol delivery during high-flow nasal therapy. Pulmonary Therapy. 2019;5:43–54.
Kelly JT, Asgharian B, Kimbell JS, Wong B. Particle deposition in human nasal airway replicas manufactured by different methods. Part I: inertial regime particles. Aerosol Sci Technol. 2004;38:1063–71.
Cheng YS. Aerosol deposition in the extrathoracic region. Aerosol Sci Technol. 2003;37:659–71.
Golshahi L, Noga ML, Thompson RB, Finlay WH. In vitro deposition measurement of inhaled micrometer-sized particle in extrathoracic airways of children and adolescents during nose breathing. J Aerosol Sci. 2011;42:474–88.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dutta, R., Spence, B., Wei, X. et al. CFD Guided Optimization of Nose-to-Lung Aerosol Delivery in Adults: Effects of Inhalation Waveforms and Synchronized Aerosol Delivery. Pharm Res 37, 199 (2020). https://doi.org/10.1007/s11095-020-02923-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02923-8