Abstract
Purpose
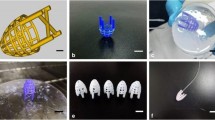
Due to low therapeutic efficacy and severe adverse reaction of systemic administration for coronary heart disease (CHD) therapy, we designed a novel local target delivery system, called Active hydraulic ventricular Support Drug delivery system (ASD). This study aims to investigate the potential advantages of ASD compared to intrapericardial (IPC) injection and factors affecting drug absorption through epicardium.
Methods
Liposoluble, water soluble and viscous solutions of cyanine 5 (Cy5) fluorescent dye were delivered individually through ASD and IPC in Sprague-Dawley (SD) rats and then tissues were isolated and observed by in vivo imaging system. Atria and ventricles of the heart were taken for the paraffin section and observed under a fluorescence microscope.
Results
The fluorescence intensity of Cy5 injected by ASD distributed in the heart was significantly higher than IPC injection. Whereas, the fluorescence signal spread in other tissues such as lung, liver, spleen, and kidney of ASD groups was much weaker. Moreover, when choosing liposoluble and viscous Cy5, the intensity of the heart turned stronger and fluorescence dye distributed in other tissues was lesser.
Conclusions
The application of ASD device may provide a promising route of drug delivery for CHD. Furthermore, increasing viscosity of the solution and liposolublity of the drug was beneficial to facilitate drug absorption through the epicardium.









Similar content being viewed by others
References
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics - 2018 update: a report from the American Heart Association. Circulation. 2018;137:E67–E492.
Ferreira-González I. The epidemiology of coronary heart disease. Rev Española Cardiol (English Ed. 2014;67:139–44.
Horio Y, Yasue H, Okumura K, Takaoka K, Matsuyama K, Goto K, et al. Effects of intracoronary injection of acetylcholine on coronary arterial hemodynamics and diameter. Am J Cardiol. 1988;62:887–91.
Williams AR, Trachtenberg B, Velazquez DL, McNiece I, Altman P, Rouy D, et al. Intramyocardial stem cell injection in patients with ischemic cardiomyopathy: functional recovery and reverse remodeling. Circ Res. 2011;108:792–6.
Pokushalov E, Romanov A, Chernyavsky A, Larionov P, Terekhov I, Artyomenko S, et al. Efficiency of intramyocardial injections of autologous bone marrow mononuclear cells in patients with ischemic heart failure: a randomized study. J Cardiovasc Transl Res. 2010;3:160–8.
Zhu H, Jiang X, Li X, Hu M, Wan W, Wen Y, et al. Intramyocardial delivery of VEGF165 via a novel biodegradable hydrogel induces angiogenesis and improves cardiac function after rat myocardial infarction. Heart Vessel. 2016;31:963–75.
Uchida Y, Yanagisawa-Miwa A, Nakamura F, Yamada K, Tomaru T, Kimura K, et al. Angiogenic therapy of acute myocardial infarction by intrapericardial injection of basic fibroblast growth factor and heparin sulfate: an experimental study. Am Heart J. 1995;130:1182–8.
Laham RJ, Rezaee M, Post M, Xu X, Sellke FW. Intrapericardial administration of basic fibroblast growth factor: myocardial and tissue distribution and comparison with intracoronary and intravenous administration. Catheter Cardiovasc Interv. 2003;58:375–81.
Defouilloy C, Meyer G, Slama M, Galy C, Verhaeghe P, Touati G, et al. Intrapericardial fibrinolysis: a useful treatment in the management of purulent pericarditis. Intensive Care Med. 1997;23:117–8.
Bolderman RW, Rob Hermans JJ, Rademakers LM, Jansen TS, Verheule S, Van Der Veen FH, et al. Intrapericardial delivery of amiodarone and sotalol: atrial transmural drug distribution and electrophysiological effects. J Cardiovasc Pharmacol. 2009;54:355–63.
Carvas M, Nascimento BCG, Acar M, Nearing BD, Belardinelli L, Verrier RL. Intrapericardial ranolazine prolongs atrial refractory period and markedly reduces atrial fibrillation inducibility in the intact porcine heart. J Cardiovasc Pharmacol. 2010;55:286–91.
Maslov M, Foianini S, Lovich M. Delivery of drugs, growth factors, genes and stem cells via intrapericardial, epicardial and intramyocardial routes for sustained local targeted therapy of myocardial disease. Expert Opin Drug Deliv. 2017;14:1227–39.
Zhou Xiaohui (2010) Active Hydraulic Ventricular Attaching Support System. United State Patents. https://doi.org/US 9,089,425 B2.
Teo AJT, Mishra A, Park I, Kim YJ, Park WT, Yoon YJ. Polymeric biomaterials for medical implants and devices. ACS Biomater Sci Eng. 2016;2:454–72.
Ulery BD, Nair LS, Laurencin CT. Biomedical applications of biodegradable polymers. J Polym Sci Part B Polym Phys. 2011;49:832–64.
Naveed M, Wenhua L, Gang W, Mohammad IS, Abbas M, Liao X, et al. A novel ventricular restraint device (ASD) repetitively deliver Salvia miltiorrhiza to epicardium have good curative effects in heart failure management. Biomed Pharmacother. 2017;95:701–10.
Yue S, Naveed M, Gang W, Chen D, Wang Z, Yu F, et al. Cardiac support device (ASD) delivers bone marrow stem cells repetitively to epicardium has promising curative effects in advanced heart failure. Biomed Microdevices. 2018;20:40.
Snoeks TJA, Löwik CWGM, Kaijzel EL. “In vivo” optical approaches to angiogenesis imaging. Angiogenesis. 2010;13:135–47.
Li X, Mikrani R, Li C, Naveed M, Liu Z, Abbas M, et al. An epicardial delivery of nitroglycerine by active hydraulic ventricular support drug delivery system improves cardiac function in a rat model. Drug Deliv Transl Res. 2020;10:23–33.
Jensen EC. Quantitative analysis of histological staining and fluorescence using ImageJ. Anat Rec. 2013;296:378–81.
Feldman AT, Wolfe D. Tissue processing and hematoxylin and eosin staining. Methods Mol Biol. 2014;1180:31–43.
Nishida K, Nakakoga Y, Sato N, Kawakami S, Mukai T, Sasaki H, et al. Effect of viscous additives on drug absorption from the liver surface in rats using phenol red as a model. Eur J Pharm Biopharm. 2000;50:397–402.
Sasaki H, Yamamura K, Mukai T, Nishida K, Nakamura J, Nakashima M, et al. Pharmacokinetic prediction of the ocular absorption of an instilled drug with ophthalmic viscous vehicle. Biol Pharm Bull. 2000;23:1352–6.
Dib N, Khawaja H, Varner S, McCarthy M, Campbell A. Cell therapy for cardiovascular disease: a comparison of methods of delivery. J Cardiovasc Transl Res. 2011;4:177–81.
Herity NA, Lo ST, Oei F, Lee DP, Ward MR, Filardo SD, et al. Selective regional myocardial infiltration by the percutaneous coronary venous route: a novel technique for local drug delivery. Catheter Cardiovasc Interv. 2000;51:358–63.
Hou D, Youssef EAS, Brinton TJ, Zhang P, Rogers P, Price ET, et al. Radiolabeled cell distribution after intramyocardial, intracoronary, and interstitial retrograde coronary venous delivery: implications for current clinical trials. Circulation. 2005;112:I150–6.
Ly HQ, Hoshino K, Pomerantseva I, Kawase Y, Yoneyama R, Takewa Y, et al. In vivo myocardial distribution of multipotent progenitor cells following intracoronary delivery in a swine model of myocardial infarction. Eur Heart J. 2009;30:2861–8.
Baek SH, Hrabie JA, Keefer LK, Hou D, Fineberg N, Rhoades R, et al. Augmentation of intrapericardial nitric oxide level by a prolonged-release nitric oxide donor reduces luminal narrowing after porcine coronary angioplasty. Circulation. 2002;105:2779–84.
Llano R, Epstein S, Zhou R, Zhang H, Hamamdzic D, Keane MG, et al. Intracoronary delivery of mesenchymal stem cells at high flow rates after myocardial infarction improves distal coronary blood flow and decreases mortality in pigs. Catheter Cardiovasc Interv. 2009;73:251–7.
Gäbel R, Klopsch C, Furlani D, Yerebakan C, Li W, Ugurlucan M, et al. Single high-dose intramyocardial administration of erythropoietin promotes early intracardiac proliferation, proves safety and restores cardiac performance after myocardial infarction in rats☆. Interact Cardiovasc Thorac Surg. 2009;9:20–5.
Gertz ZM, Wilensky RL. Local drug delivery for treatment of coronary and peripheral artery disease. Cardiovasc Ther. 2011;29:e54–66.
Garcia JR, Campbell PF, Kumar G, Langberg JJ, Cesar L, Wang L, et al. A minimally invasive, translational method to deliver hydrogels to the heart through the pericardial space. JACC Basic Transl Sci. 2017;2:601–9.
Fukushima S, Campbell NG, Coppen SR, Yamahara K, Yuen AHY, Smolenski RT, et al. Quantitative assessment of initial retention of bone marrow mononuclear cells injected into the coronary arteries. J Hear Lung Transplant. 2011;30:227–33.
Liu Z, Mikrani R, Zubair HM, Taleb A, Naveed M, Baig MMFA, et al. Systemic and local delivery of mesenchymal stem cells for heart renovation: challenges and innovations. Eur J Pharmacol. 2020;876:173049.
Vanderheyden M, Vercauteren S, Mansour S, Delrue L, Vandekerckhove B, Heyndrickx GR, et al. Time-dependent effects on coronary remodeling and epicardial conductance after intracoronary injection of enriched hematopoietic bone marrow stem cells in patients with previous myocardial infarction. Cell Transplant. 2007;16:919–25.
Bartunek J, Wijns W, Heyndrickx GR, Vanderheyden M. Timing of intracoronary bone-marrow-derived stem cell transplantation after ST-elevation myocardial infarction. Nat Clin Pract Cardiovasc Med. 2006;3:S52–6.
Dib N, Menasche P, Bartunek JJ, Zeiher AM, Terzic A, Chronos NA, et al. Recommendations for successful training on methods of delivery of biologics for cardiac regeneration. A Report of the International Society for Cardiovascular Translational Research. JACC Cardiovasc Interv. 2010;3:265–75.
Nguyen QT, Olson ES, Aguilera TA, Jiang T, Scadeng M, Ellies LG, et al. Surgery with molecular fluorescence imaging using activatable cell-penetrating peptides decreases residual cancer and improves survival. Proc Natl Acad Sci U S A. 2010;107:4317–22.
Frangioni JV. In vivo near-infrared fluorescence imaging. Curr Opin Chem Biol. 2003;7:626–34.
Yasmeen S, Liao X, Khan FU, Ihsan AU, Li X, Li C, et al. A novel approach to devise the therapy for ventricular fibrillation by epicardial delivery of lidocaine using active hydraulic ventricular attaching support system: an experimental study in rats. J Biomed Mater Res - Part B Appl Biomater. 2019;107:1722–31.
Naveed M, Wenhua L, Gang W, Mohammad IS, Abbas M, Liao X, et al. A novel ventricular restraint device (ASD) repetitively deliver Salvia miltiorrhiza to epicardium have good curative effects in heart failure management. Biomed Pharmacother. 2017;95:701–10.
Tanaka A, Furubayashi T, Yamasaki H, Takano K, Kawakami M, Kimura S, et al. The enhancement of nasal drug absorption from powder formulations by the addition of sodium carboxymethyl cellulose. IEEE Trans Nanobioscience. 2016;15:798–803.
Cho HJ, Jee JP, Kang JY, Shin DY, Choi HG, Maeng HJ, et al. Cefdinir solid dispersion composed of hydrophilic polymers with enhanced solubility, dissolution, and bioavailability in rats. Molecules. 2017;22. https://doi.org/10.3390/molecules22020280.
Ashley JJ, Levy G. Effect of vehicle viscosity and an anticholinergic agent on bioavailability of a poorly absorbed drug (phenolsulfonphthalein) in man. J Pharm Sci. 1973;62:688–90.
Wang L, Peng J, Wang X, Zhu X, Cheng B, Gao J, et al. Carboxymethylcellulose sodium improves the pharmacodynamics of 1-deoxynojirimycin by changing its absorption characteristics and pharmacokinetics in rats. Pharmazie. 2012;67:168–73.
Männer J, Pérez-Pomares JM, Macías D, Muñoz-Chápuli R. The origin, formation and developmental significance of the epicardium: a review. Cells Tissues Organs. 2001;169:89–103.
Cao J, Poss KD. The epicardium as a hub for heart regeneration. Nat Rev Cardiol. 2018;15:631–47.
Narita T, Shintani Y, Ikebe C, Kaneko M, Campbell NG, Coppen SR, et al. The use of scaffold-free cell sheet technique to refine Mesenchymal stromal cell-based therapy for heart failure. Mol Ther. 2013;21:860–7.
Koomalsingh KJ, Witschey WRT, McGarvey JR, Shuto T, Kondo N, Xu C, et al. Optimized local infarct restraint improves left ventricular function and limits remodeling. Ann Thorac Surg. 2013;95:155–62.
Naveed M, Han L, Khan GJ, Yasmeen S, Mikrani R, Abbas M, et al. Cardio-supportive devices (VRD & DCC device) and patches for advanced heart failure: a review, summary of state of the art and future directions. Biomed Pharmacother. 2018;102:41–54.
Xiaohui Z (2010) Active hydraulic ventricular attaching support system.
Sembatya KR, Gang W, Muhammad N, Yasmeen S, Zhou X (2020) Cardioprotective effect of silicone built restraint device (ASD), for left ventricle remodeling in rat heart failure models. Authorea Prepr. https://doi.org/10.22541/AU.158888126.60534417.
Funding
This study is sponsored by the National Nature Science Foundation of China (grant numbers 30973003 & 30901993) and Qing Lan Project of Jiangsu Province, China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflict of interest.
Additional information
Reyaj Mikrani and Cunyu Li are co-first authors
Rights and permissions
About this article
Cite this article
Mikrani, R., Li, C., Naveed, M. et al. Pharmacokinetic Advantage of ASD Device Promote Drug Absorption through the Epicardium. Pharm Res 37, 173 (2020). https://doi.org/10.1007/s11095-020-02898-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02898-6