Abstract
Purpose
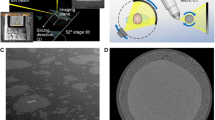
Desorption electrospray ionization mass spectrometry imaging (DESI-MSI) coupled with gas-phase ion mobility spectrometry was used to characterize the drug distribution in polymeric implants before and after exposure to accelerated in vitro release (IVR) media. DESI-MSI provides definitive chemical identification and localization of formulation components, including 2D chemical mapping of individual components with essentially no sample preparation.
Methods
Polymeric implants containing 40% (w/w) entecavir and poly(D,L-lactide) (PLA) were prepared and then exposed to either acidified PBS (pH 2.5) or MeOH:H2O (50:50, v/v) medias during a 7-day IVR test using continuous flow-through (CFT) cell dissolution. The amount of drug released from the polymer matrix during the 7-day IVR test was monitored by online-ultraviolet spectroscopy (UV) and HPLC-UV. After that period, intact implants and radial sections of implants were analyzed by DESI-MSI with ion mobility spectrometry. The active ingredient along with impurities and contaminants were used to generate chemical maps before and after exposure to the release medias.
Results
Bi-phasic release profiles were observed for implants during IVR release using both medias. During the second phase of release, implants exposed to PBS, pH 2.5, released the entecavir faster than the implants exposed to MeOH:H2O (50:50, v/v). Radial images of the polymer interior show that entecavir is localized along the central core of the implant after exposure to MeOH:H2O (50:50, v/v) and that the drug is more uniformly distributed throughout the implant after exposure to acidified PBS (pH 2.5).
Conclusions
DESI-MSI coupled with ion mobility analysis produced chemical images of the drug distribution on the exterior and interior of cylindrical polymeric implants before and after exposure to various release medias. These results demonstrated the utility of this technique for rapid characterization of drug and impurity/degradant distribution within polymeric implants with direct implications for formulation development as well as analytical method development activities for various solid parenteral and oral dosage forms. These results are especially meaningful since samples were analyzed with essentially no preparative procedures.





Similar content being viewed by others
Abbreviations
- API:
-
Active Pharmaceutical Ingredient
- CFT:
-
Continuous flow-through
- DESI:
-
Desorption electrospray ionization
- HDI:
-
High definition imaging
- HDMS:
-
High-definition mass spectrometry
- HPLC:
-
High-performance liquid chromatography
- IM:
-
Intramuscular
- IMS:
-
Ion mobility spectrometry
- LAP:
-
Long-acting parenteral
- MSI:
-
Mass spectrometry imaging
- PBS:
-
Phosphate-buffered saline
- PLA:
-
Poly(D,L-lactide)
- SC:
-
Subcutaneous
- TIC:
-
Total ion chromatogram
- USP:
-
United States Pharmacopeia
- UV:
-
Ultraviolet
References
Kreye F, Hamm G. MALDI-TOF imaging of controlled release implants. J Control Release. 2012;161:98–108.
Hamoudi-Ben Yelles MC, Tran Tan V, Danede F, Willart JF, Siepmann J. PLGA implants: How Poloxamer/PEO addition slows down or accelerates polymer degradation and drug release. J Control Release. 2017;253:19–29.
Bhardwaj U, Sura R, Papadimitrakopoulos F, Burgess DJ. PLGA/PVA hydrogel composites for long-term inflammation control following s.c. implantation. Int. J. Pharm. 2010;384:76–86.
Shi Y, Li LC. Current advances in sustained-release systems for parenteral drug delivery. Expert Opin Drug Deliv. 2005;2:1039–58.
Shen J, Burgess DJ. Accelerated in-vitro release testing methods for extended-release parenteral dosage forms. J Pharm Pharmacol. 2012;64:986–96.
Sasić S. Raman mapping of low-content API pharmaceutical formulations. I. Mapping of Alprazolam in Alprazolam/Xanax tablets. Pharm Res. 2007;24:58–65.
Sasić S. An in-depth analysis of Raman and near-infrared chemical images of common pharmaceutical tablets. Appl Spectrosc. 2007;61:239–50.
Zhang Q, Gladden L, Avalle P, Mantle M. in vitro quantitative 1H and 19F nuclear magnetic resonance spectroscopy and imaging studies of fluvastatin ™ in Lescol ® XL tablets in a USP-IV dissolution cell. J Control Release. 2011;156:345–54.
Bodzon-Kulakowska A, Suder P. Imaging mass spectrometry: instrumentation, applications, and combination with other visualization techniques. Mass Spectrom Rev. 2016;25:147–69.
Wu C, Dill AL, Eberlin LS, Cooks RG, Ifa DR. Mass spectrometry imaging under ambient conditions. Mass Spectrom Rev. 2013;32:218–43.
Earnshaw CJ, Carolan VA, Richards DS, Clench MR. Direct analysis of pharmaceutical tablet formulations using Matrix-Assisted Laser Desorption/Ionisation Mass Spectrometry Imaging. Rapid Commun Mass Spectrom. 2010;24:1665–72.
McDonnell LA, Heeren RM. Imaging mass spectrometry. Mass Spectrom Rev. 2007;26:606–43.
Veryovkin IV, Callaway WF, Tripa CE, Pellin MJ. Mass Spectrometry on the nanoscale with ion sputtering based techniques: What is feasible. Nucl Instrum Methods Phys Res B. 2007;261:508–11.
Ifa DR, Wiseman JM, Song Q, Cooks RG. Development of capabilities for imaging mass spectrometry under ambient conditions with desorption electrospray ionization (DESI). Int J Mass Spectrom. 2007;259:8–15.
Takats Z, Wiseman JM, Gologan B, Cooks RG. Mass spectrometry sampling under ambient conditions with desorption electrospray ionization. Science. 2004;306:471–3.
Wiseman JM, Ifa DR, Song Q, Cooks RG. Tissue imaging at atmospheric pressure using desorption electrospray ionization (DESI) mass spectrometry. Angew Chem Int Ed Engl. 2006;45:188–92.
Leuthold LA, Mandscheff JF, Fathi M, Giroud C, Augsburger M, Varesio E, et al. Desorption electrospray ionization mass spectrometry: direct toxilogical screening and analysis of illicit Ecstasy tablets. Rapid Commun Mass Spectrom. 2006;20:103–10.
Weston DJ, Bateman R, Wilson ID, Wood TR, Creaser CS. Direct analysis of pharmaceutical drug formulations using ion mobility spectrometry/quadrupole-time-of-flight mass spectrometry combined with desorption electrospray ionization. Anal Chem. 2005;77:7572–80.
Williams JP, Scrivens JH. Rapid accurate mass desorption electrospray ionization tandem mass spectrometry of pharmaceutical samples. Rapid Commun Mass Spectrom. 2005;19:3643–50.
Cornett DS, Frappier SL, Caprioli RM. MALDI-FTICR Imaging Mass Spectrometry of Drugs and Metabolites in Tissue. Anal Chem. 2008;80:5648–53.
Skraskova K, Claude E, Jones EA, Towers M, Ellis SR, Heeren RM. Enhanced capabilities for imaging gangliosides in murine brain with matrix-assisted laser desorption/ionizatoin and desorption electrospray ionization mass spectrometry coupled to ion mobility separation. Methods. 2016;104:67–78.
Chouinard CD, Beekman CR, Kemperman RHJ, Harrison MK, Yost RA. Ion mobility-mass spectrometry separation of steroid structural isomers and epimers. Int J Ion Mobil Spectrom. 2017;20:31–9.
Lanucara F, Holman SW, Gray CJ, Eyers CE. The power of ion mobility-mass spectrometry for structural characterization and the study of conformational dynamics. Nat Chem. 2014;6:281–94.
Harvey SR, MacPhee CE, Barran PE. Ion mobility mass spectrometry for peptide analysis. Methods. 2011;54:454–61.
Wyttenbach T, Pierson NA, Clemmer DE, Bowers MT. Ion mobility analysis of molecular dynamics. Annu Rev Phys Chem. 2015;65:175–96.
Zhong Y, Hyung SJ, Ruotolo BT. Ion mobility-mass spectrometry for structural proteomics. Expert Rev Proteomics. 2012;9:47–58.
Baraclude, INN-Entecavir, Copyright EMEA 2006 (https://www.ema.europa.eu/en/documents/scientific-discussion/baraclude-epar-scientific-discussion_en.pdf).
Henry SJ, Barrett SE, Forster SP, Teller RS, Yang Z, Li L, et al. Exploration of long-acting implant formulation of hepatitis B drug entecavir. J Pharm Sci. 2019;136:104958.
Kakhi M. Classification of the flow regimes in the flow-through cell. Eur J Pharm Sci. 2009;37:531–44.
Yoshida H, Kuwana A, Shibata H, Izutsu K, Goda Y. Effects of Pump Pulsation on Hydrodynamic Properties and Dissolution Profiles in Flow-Through Dissolution Systems (USP-4). Pharm Res. 2016;33:1327–36.
Baraclude (entecavir) Prescribing Information, Bristol-Myers Squibb.
Pitt CG, Gratzl MM, Kimmel GL, Surles J, Schindler A. Aliphatic polyesters II. The degradation of poly (DL-lactide), poly (epsilon-caprolactone), and their copolymers in vivo. Biomaterials. 1981;2:251–20.
C Brown D, Kieselmann, S. Low-level Drug Release-Rate Testing of Ocular Implants Using USP Apparatus 4 Dissolution and HPLC End Analysis. Dissolution Technologies. 2010; https://doi.org/10.14227/DT170110P12.
Neubert A, Sternberg K, Nagel S, Harder C, Schmitz KP, Kroemer HK, et al. Development of a vessel-simulating flow-through cell method for the in vitro evaluation of release and distribution from drug-eluting stents. J. Control Release. 2008;130:2–8.
Shen J, Burgess DJ. Accelerated in-vitro release testing methods for extended-release parenteral dosage forms. J Pharm Pharmacol. 2012;64:986–96.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors would like to thank Ray Seto for his assistance with producing radial sections of the implants. Additionally, a special thanks to Stephanie Barrett, Justin Pennington, Paul Walsh, and W. Peter Wuelfing for their helpful insights and discussions. Financial support for this work was provided by Merck & Co., Inc., Kenilworth, NJ, USA and Waters Corporation, Beverly, MA, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pierson, E.E., Midey, A.J., Forrest, W.P. et al. Direct Drug Analysis in Polymeric Implants Using Desorption Electrospray Ionization – Mass Spectrometry Imaging (DESI-MSI). Pharm Res 37, 107 (2020). https://doi.org/10.1007/s11095-020-02823-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02823-x