Abstract
Purposes
Senescence is an inevitable and irreversible process, which may lead to loss in muscle and bone density, decline in brain volume and loss in renal clearance. Although aging is a well-known process, few studies on the consumption of nanodrugs by elderly people were performed.
Methods
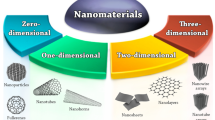
We evaluated three different nanosystems: i) carbon based nanosystem (Graphene Quantum Dots, GQD), ii) polymeric nanoparticles and mesoporous silica (magnetic core mesoporous silica, MMSN). In previous studies, our group has already characterized GQD and MMSN nanoparticles by dynamic light scattering analysis, atomic force microscopy, transmission electron microscopy, X-ray diffraction, Raman analysis, fluorescence and absorbance. The polymeric nanoparticle has been characterized by AFM and DLS. All the nanosystems were radiolabeled with 99 m-Tc by. The in vivo biodistribution/tissue deposition analysis evaluation was done using elder (PN270) and young (PN90) mice injected with radioactive nanosystems.
Results
The nanosystems used in this study were well-formed as the radiolabeling processes were stable. Biodistribution analysis showed that there is a decrease in the uptake of the nanoparticles in elder mice when compared to young mice, showing that is necessary to increase the initial dose in elder people to achieve the same concentration when compared to young animals.
Conclusion
The discrepancy on tissue distribution of nanosystems between young and elder individuals must be monitored, as the therapeutic effect will be different in the groups. Noteworthy, this data is an alarm that some specific conditions must be evaluated before commercialization of nano-drugs.

Changes between younger and elderly individuals are undoubtedly, especially in drug tissue deposition, biodistribution and pharmacokinetics. The same thought should be applied to nanoparticles. A comprehensive analysis on how age discrepancy change the biological behavior of nanoparticles has been performed.







Similar content being viewed by others
Abbreviations
- DNA:
-
Deoxyribonucleic acid
- IL-6:
-
Interleukin-6
- TNF-alpha:
-
Tumor Necrosis factor-alpha
- NPs:
-
Nanoparticles
- PCL:
-
Polycaprolactone (PCL)
- PDI:
-
Polydispersity index (PDI)
- DLS:
-
Dynamic light scattering (DLS)
- 99mTc:
-
99mTechentium
- MMSN:
-
Magnetic core mesoporous silica
- GQDs:
-
Graphene quantum dots
- PN90:
-
Postnatal day 90 (young animals)
- PN270:
-
Postnatal day 270 (elder animals)
- AFM:
-
Atomic Force Microscopy
References
Liu Y, Gao W, Koellmann C, Le Clerc S, Huls A, Li B, et al. Genome-wide scan identified genetic variants associated with skin aging in a Chinese female population. J Dermatol Sci. 2019. https://doi.org/10.1016/j.jdermsci.2019.08.010.
Thomas N, Gurvich C, Kulkarni J. Sex differences in aging and associated biomarkers. Adv Exp Med Biol. 2019;1178:57–76. https://doi.org/10.1007/978-3-030-25650-0_4.
Shavlakadze T, Morris M, Fang J, Wang SX, Zhu J, Zhou W, et al. Age-related gene expression signature in rats demonstrate early, late, and linear transcriptional changes from multiple tissues. Cell Rep. 2019;28:3263–3273.e3. https://doi.org/10.1016/j.celrep.2019.08.043.
Dodig S, Čepelak I, Pavić I. Hallmarks of senescence and aging. Biochem medica. 2019;29:30501. https://doi.org/10.11613/bm.2019.030501.
Victorelli S, Passos JF. Telomeres and cell senescence. EBioMedicine. 2017;21:14–20. https://doi.org/10.1016/j.ebiom.2017.03.027.
M. Chiriaco, G. Georgiopoulos, E. Duranti, L. Antonioli, I. Puxeddu, M. Nannipieri, J. Rosada, C. Blandizzi, S. Taddei, A. Virdis, et al., Inflammation and vascular ageing: from telomeres to novel emerging mechanisms, high blood press. Cardiovasc. Prev. (2019) 321–329. https://doi.org/10.1007/s40292-019-00331-7.
Pereira BI, Devine OP, Vukmanovic-Stejic M, Chambers ES, Subramanian P, Patel N, et al. Senescent cells evade immune clearance via HLA-E-mediated NK and CD8+ T cell inhibition. Nat Commun. 2019;10:2387 https://doi.org/10.1038/s41467-019-10335-5.
T. Tchkonia, J. L. Kirkland, JAMA , Aging, cell senescence, and chronic disease, (2018), 1319. https://doi.org/10.1001/jama.2018.12440.
D. S. Cho, J. D. Doles, Skeletal muscle progenitor cell heterogeneity, Adv. Exp. Med. Biol. (2019)179–193. https://doi.org/10.1007/978-3-030-24108-7_9.
K. Kounakis, N. Tavernarakis, The cytoskeleton as a modulator of aging and neurodegeneration. Adv Exp Med Biol. (2019), 227–245. https://doi.org/10.1007/978-3-030-25650-0_12.
Forsberg A, Johnson W, Logie RH. Aging and feature-binding in visual working memory: the role of verbal rehearsal. Psychol Aging. 2019. https://doi.org/10.1037/pag0000391.
B. Pan, H. Li, Y. Wang, M. Sun, H. Cai, J. Wang, Physical activity and the risk of frailty among community-dwelling healthy older adults. Medicine (Baltimore). (2019),, e16955. https://doi.org/10.1097/md.0000000000016955.
M. Ogrodnik, H. Salmonowicz, V. N. Gladyshev, Integrating cellular senescence with the concept of damage accumulation in aging: Relevance for clearance of senescent cells., Aging Cell (2019) e12841. https://doi.org/10.1111/acel.12841.
Bu H, Wedel S, Cavinato M, Jansen-Dürr P. MicroRNA regulation of oxidative stress-induced cellular senescence. Oxidative Med Cell Longev. 2017:1–17. https://doi.org/10.1155/2017/2398696.
H. Song, M. Wei, N. Zhang, H. Li, X. Tan, Y. Zhang, W. Zheng, Enhanced permeability of blood–brain barrier and targeting function of brain via borneol-modified chemically solid lipid nanoparticle, Int. J. Nanomedicine (2018) 1869–1879. https://doi.org/10.2147/ijn.s161237.
A. Alexander, M. Agrawal, A. Uddin, S. Siddique, A. M. Shehata, M. A. Shaker, S. Ata Ur Rahman, M. I. M. Abdul, M. A. Shaker, Recent expansions of novel strategies towards the drug targeting into the brain. Int. J. Nanomedicine (2019) 5895–5909. https://doi.org/10.2147/ijn.s210876
Faustino C, Rijo P, Reis CP. Nanotechnological strategies for nerve growth factor delivery: therapeutic implications in Alzheimer’s disease. Pharmacol Res. 2017;120:68–87. https://doi.org/10.1016/j.phrs.2017.03.020.
Y. Xiao, D. Xu, H. Song, F. Shu, P. Wei, X. Yang, C. Zhong, X. Wang, W. E. Muller, Y. Zheng, et al., Cuprous oxide nanoparticles reduces hypertrophic scarring by inducing fibroblast apoptosis. Int. J. Nanomedicine (2019) 5989–6000. https://doi.org/10.2147/ijn.s196794.
Choi YH, Han H-K. Nanomedicines: current status and future perspectives in aspect of drug delivery and pharmacokinetics. J Pharm Investig. 2018;48:43–60. https://doi.org/10.1007/s40005-017-0370-4.
R.-M. F, S. N, A. N, J. N. Gold-Curcumin Nanostructure in Photothermal Therapy on Breast Cancer Cell Line: 650 and 808 nm Diode Lasers as Light Sources.Biomed. Phys. Eng. (2019). https://doi.org/10.31661/jbpe.v0i0.906.
Dhas N, Ige P, Kudarha R. Design, optimization and in-vitro study of folic acid conjugated-chitosan functionalized plga nanoparticle for delivery of bicalutamide in prostate cancer. Power Technol. 2015;283:234–45. https://doi.org/10.1016/j.powtec.2015.04.053.
Jain A, Jain A, Garg NK, Tyagi RK, Singh B, Katare OP, et al. Surface engineered polymeric nanocarriers mediate the delivery of transferrin–methotrexate conjugates for an improved understanding of brain cancer. Acta Biomater. 2015;24:140–51. https://doi.org/10.1016/j.actbio.2015.06.027.
M. Ben Haddada, D. Koshel, Z. Yang, W. Fu, J. Spadavecchia, S. Pesnel, A.-L. Morel, Proof of concept of plasmonic thermal destruction of surface cancers by gold nanoparticles obtained by green chemistry. Colloids Surf. B. Biointerfaces (2019) 110496. https://doi.org/10.1016/j.colsurfb.2019.110496
R. Maity, M. Chatterjee, A. Banerjee, A. Das, R. Mishra, S. Mazumder, N. Chanda, Gold nanoparticle-assisted enhancement in the anti-cancer properties of theaflavin against human ovarian cancer cells. Mater. Sci. Eng. C. Mater. Biol. Appl. (2019) 109909. https://doi.org/10.1016/j.msec.2019.109909
L.-X. Gai, W.-Q. Wang, X. Wu, X.-J. Su, F.-C. Yang, J. NIR absorbing reduced graphene oxide for photothermal radiotherapy for treatment of esophageal cancer. Photochem. Photobiol. B. (2019) 188–193. https://doi.org/10.1016/j.jphotobiol.2019.03.014.
Zheng Z, Huang L, Yan L, Yuan F, Wang L, Wang K, et al. Polyaniline functionalized Graphene Nanoelectrodes for the regeneration of PC12 cells via electrical stimulation. Int J Mol Sci. 2019;2013. https://doi.org/10.3390/ijms20082013.
Fan C, Kong F, Shetti D, Zhang B, Yang Y, Wei K. Resveratrol loaded oxidized mesoporous carbon nanoparticles: a promising tool to treat triple negative breast cancer. Biochem Biophys Res Commun. 2019. https://doi.org/10.1016/j.bbrc.2019.09.016.
R. Kamakura, M. Kovalainen, J. Riikonen, T. Nissinen, G. Shere Raza, J. Walkowiak, V.-P. Lehto, K.-H. Herzig. Inorganic mesoporous particles for controlled α-linolenic acid delivery to stimulate GLP-1 secretion in vitro, Eur. J. Pharm. Biopharm. (2019) 132–138, https://doi.org/10.1016/j.ejpb.2019.09.009.
Y.-C. Lin, C.-F. Lin, A. Alalaiwe, P.-W. Wang, Y.-P. Fang, J.-Y. Fang, UV filter entrapment in mesoporous silica hydrogel for skin protection against UVA with minimization of percutaneous absorption. Eur. J. Pharm. Sci. (2018) 185–194. https://doi.org/10.1016/j.ejps.2018.07.013.
Y. He, S. Liang, M. Long, H. XuMesoporous silica nanoparticles as potential carriers for enhanced drug solubility of paclitaxel. Mater Sci Eng C, 78 (2017), pp. 12–17.
Portilho FL, Helal Neto E, Cabezas SS, Pinto SR, Dos Santos SN, Pozzo L, et al. Magnetic core mesoporous silica nanoparticles doped with dacarbazine and labelled with 99mTc for early and differential detection of metastatic melanoma by single photon emission computed tomography. Nanomedicine, And Biotechnology: Artificial Cells; 2018. p. 1080–7. https://doi.org/10.1080/21691401.2018.1443941.
de Menezes FD, Dos Reis SRR, Pinto SR, Portilho FL, do Vale Chaves E Mello F, Helal-Neto E, da Silva de Barros AO et al. Graphene quantum dots unraveling: green synthesis, characterization, radiolabeling with 99mTc, in vivo behavior and mutagenicity Materials Science and Engineering. (2019) 102, p.405–414. https://doi.org/10.1016/j.msec.2019.04.058.
Saez, V, De Menezes FD, Dos Santos CC, Alencar, LMR, Ricci-Junior E, Mansur CRE, Santos-Oliveira R. Graphene quantum dots nanoparticles changed the rheological properties of hydrophilic gels (carbopol). Journal of Molecular Liquids. (2019) 110949. https://doi.org/10.1016/j.molliq.2019.110949
Dos Santos, SN, Dos Reis SR, Pires LP, Helal-Neto E, Sancenon F, Barja-Fidalgo, TC, De Mattos RM et al.. Avoiding the mononuclear phagocyte system using human albumin for mesoporous silica nanoparticle system. Microporous And Mesoporous Materials. (2017) 181–189. https://doi.org/10.1016/j.micromeso.2017.06.005.
Rosa TG, Dos Santos SN, de Jesus Andreoli Pinto T, Ghisleni DDM, Barja-Fidalgo TC, Ricci-Junior E, Al-Qahtani M, Kozempel J, Bernardes ES, Santos-Oliveira R. Microradiopharmaceutical for Metastatic Melanoma. Pharmaceutical Research. (2017). 2922–2930. https://doi.org/10.1007/s11095-017-2275-3.
Fatemika H, Seyedabadi M, Karimi Z, Tanha K, Assadi M, Tanha K. Comparison of 99mTc-DMSA renal scintigraphy with biochemical and histopathological findings in animal models of acute kidney injury. Mol Cell Biochem. 2017;434(1–2):163–9. https://doi.org/10.1007/s11010-017-3046-5
Rodrigues VST, Moura EG, Bernardino DN, Carvalho JC, Soares PN, Peixoto TC, et al. Supplementation of suckling rats with cow's milk induces hyperphagia and higher visceral adiposity in females at adulthood, but not in males. J Nutr Biochem. 2018;55:89–103. https://doi.org/10.1016/j.jnutbio.2017.12.001.
SJ Jackson, N Andrews , D Ball , I Bellantuono, J. Gray, L. Hachoumi, A. Holmes, J. Latcham, A. Petrie, P. Potter, A. Rice, A. Ritchie, K. Chapman. Does age matter? The impact of rodent age on study outcomes. Lab Anim. (2017) Apr;51(2):160–169.
E. Lindsay, Pappas, TR. Nagy. The translation of age-related body composition findings from rodents to humans. Eur J Clin Nutr. (2019) Feb;73(2):172–178.
Adams DJ. The valley of death in anticancer drug development: a reassessment. Trends Pharmacol Sci. 2012;33:173–80.
A. Talevi, CL Bellera, M Di Ianni, M Gantner, LE Bruno- Blanch and EA Castro. CNS drug development – lost in translation? Mini Rev Med Chem. (2012) Sep 1;12(10):959–70.
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 2010;8:e1000412.
Landis SC, Amara SG, Asadullah K. A call for transparent reporting to optimize the predictive value of preclinical research. Nature. 2012;490:187.
Koff RS, Garvey AJ, Burney SW, Bell B. Absence of an age effect on sulfobromophtalein retention in healthy men. Gastroenterology. 1973;65:300–2.
Kampmann JP, Sinding J, Moller-Jorgensen I. Effect of age on liver function. Geriatrics. 1975;30:91–5.
Fu A. NK Sreekumaran. Age effect on fibrinogen and albumin synthesis in humans. Am J Phys. 1998;275.
Mori K, Blackshear PE, Lobenhofer EK. Hepatic transcript levels for genes coding for enzymes associated with xenobiotic metabolism are altered with age. Toxicol Pathol. 2007;35:242–51.
Pibiri M, Sulas P, Leoni VP. Global gene expression profile of normal and regenerating liver in young and old mice. Age (Dordr). 2015;37:9796.
Castleden CM, George CF. The effect of ageing on the hepatic clearance of propranolol. Br J Clin Pharmacol. 1979;7:49–54.
Greenblatt DJ, Harmatz JS, Shapiro L, Engelhardt N, Gouthro TA, Shader RI. Sensitivity to triazolam in the elderly. N Engl J Med. 1991;324:1691–8.
Anantharaju A, Feller A, Chedid A. Aging liver. A review Gerontology. 2002;48:343–53.
Robertson DR, Waller DG, Renwick AG, George CF. Age-related changes in the pharmacokinetics and pharmacodynamics of nifedipine. Br J Clin Pharmacol. 1988;25:297–305.
Castleden CM, Kaye CM, Parsons RL. The effect of age on plasma levels of propranolol and practolol in man. Br J Clin Pharmacol. 1975;2:303–6.
Davies RO, Gomez HJ, Irvin JD, Walker JF. An overview of the clinical pharmacology of enalapril. Br J Clin Pharmacol. 1984;18(Suppl 2):215S–29S.
Todd PA, Fitton A. Perindopril A review of its pharmacological properties and therapeutic use. Drugs. 1991;42:90–114.
Jr Fulop T, Worum I, Csongor J, Foris G, Leovey A. Body composition in elderly people. I. Determination of body composition by multiisotope method and the elimination kinetics of these isotopes in healthy elderly subjects. Gerontology. 1985;31:6–14.
Redolfi A, Borgogelli E, Lodola E. Blood level of cimetidine in relation to age. Eur J Clin Pharmacol. 1979;15:257–61.
Zeeh J, Platt D. The aging liver: structural and functional changes and their consequences for drug treatment in old age. Gerontology. 2002;48(3):121–7.
Tateishi T, Fujimura A, Shiga T, Ohashi K, Ebihara A. Influence of aging on the oxidative and conjugative metabolism of propranolol. Int J Clin Pharmacol Res. 1995;15(3):95–101.
Anantharaju A, Feller A, Chedid A. Aging liver. A review. Gerontology. 2002;48(6):343–53.
Sun X, Yan X, Jacobson O, Sun W, Wang Z, Tong X, et al. Improved tumor uptake by optimizing liposome based RES blockade strategy. Theranostics. 2017;7(2):319.
Tsoi KM, MacParland SA, Ma X-Z, Spetzler VN, Echeverri J, Ouyang B, et al. Mechanism of hard-nanomaterial clearance by the liver. Nature Materials. 2016;15:1212.
SA MacParland, KM Tsoi, B Ouyang, XZ Ma, J Manuel, A Fawaz, MA Ostrowski, BA Alman, A Zilman, WC Chan, ID McGilvray, Phenotype determines nanoparticle uptake by human macrophages from liver and blood ACS Nano, (2017) 28;11(3), 2428.
Dreyfuss D, Shader RI, Harmatz JS, Greenblatt DJ. Kinetics and dynamics of single doses of oxazepam in the elderly: implications of absorption rate. J Clin Psychiatry. 1986;47:511–4.
Divoll M, Ameer B, Abernethy DR, Greenblatt DJ. Age does not alter acetaminophen absorption. J Am Geriatr Soc. 1982;30:240–4.
Gainsborough N, Maskrey VL, Nelson ML, Keating J, Sherwood RA, Jackson SHD, et al. The association of age with gastric emptying. Age Ageing. 1993;22:37–40.
Wynne H. Drug metabolism and ageing. J Br Menopause Soc. 2005;11(2):51–6.
Blechman MB, Gelb AM. Aging and gastrointestinal physiology. Clin Geriatr Med. 1999;15:429–38.
Klawans HL. Emerging strategies in Parkinson’s disease. Neurology. 1990;40(Suppl 3):1–76.
Rostami-Hodjegan A, Kroemer HK, Tucker GT. In vivo indices of enzyme activity. The effect of renal impairment on the assessment of CYP2D6 activity. Pharmacogenetics. 1999;9:277–86.
Yuan R, Venitz J. Effect of chronic renal failure on the disposition of highly hepatically metabolized drugs. Int J Clin Pharmacol Ther. 2000;38:245–53.
Pichette V, Leblond FA. Drug metabolism in chronic renal failure. Curr Drug Metab. 2003;4:91–103.
Wynne HA, Cope LH, Mutch E, Rawlins MD, Woodhouse KW, James OF. The effect of age upon liver volume and apparent liver blood flow in healthy man. Hepatology. 1989;9:297–301.
de Jesus FC, Helal-Neto E, Portilho FL, Rocha Pinto S, Sancenón F, Martínez-Máñez R, et al. Effect of obesity on biodistribution of nanoparticles. J Control Release. 2018 Jul 10;281:11–8. https://doi.org/10.1016/j.jconrel.2018.05.003.
De Jong WH, Hagens WI, Krystek P, Burger MC, Sips AJ. Geertsma RE particle size-dependent organ distribution of gold nanoparticles after intravenous administration. Biomaterials. 2008 Apr;29(12):1912–9.
Kattumuri V, Katti K, Bhaskaran S, Boote EJ, Casteel SW, Fent GM, et al. Gum arabic as a phytochemical construct for the stabilization of gold nanoparticles: in vivo pharmacokinetics and X-ray-contrast-imaging studies. Small. 2007 Feb;3(2):333–41.
Mohamed Anwar K Abdelhalim and Bashir M Jarrar Renal tissue alterations were size-dependent with smaller ones induced more effects and related with time exposure of gold nanoparticles. GNP Lipids Health Dis. 2011; 10: 163. https://doi.org/10.1186/1476-511X-10-163
AA Mangoni and SH Jackson. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. (2004) Jan;57(1):6–14.
S. Shaojun and K Ulrich. Age-Related Changes in Pharmacokinetics. Current Drug Metabolism, Volume 12, Number 7 (2011) pp. 601–610(10).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 214 kb)
Rights and permissions
About this article
Cite this article
dos Reis, S.R.R., Pinto, S.R., de Menezes, F.D. et al. Senescence and the Impact on Biodistribution of Different Nanosystems: the Discrepancy on Tissue Deposition of Graphene Quantum Dots, Polycaprolactone Nanoparticle and Magnetic Mesoporous Silica Nanoparticles in Young and Elder Animals. Pharm Res 37, 40 (2020). https://doi.org/10.1007/s11095-019-2754-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-019-2754-9