Abstract
Purpose
Pancreatic Polypeptide-secreting tumor of the distal pancreas (PPoma) is a rare, difficult and indolent type of cancer with a survival rate of 5-year in only 10% of all cases. The PPoma is classified as a neuroendocrine tumor (NET) not functioning that overexpresses SSTR 2 (somatostatin receptor subtype 2). Thus, in order to improve the diagnosis of this type of tumor, we developed nanoparticulate drug carriers based on poly-lactic acid (PLA) polymer loaded with octreotide and radiolabeled with Technetium-99 m (99mTc).
Methods
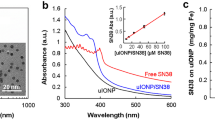
PLA/PVA octreotide nanoparticles were developed by double-emulsion technique. These nanoparticles were characterized by Atomic Force Microscopy (AFM) and Dynamic Light Scattering (DLS) and radiolabeled with 99mTc by the direct via forming 99mTc-PLA/PVA octreotide nanoparticles. The safety of these nanosystems was evaluated by the MTT cell toxicity assay and their in vivo biodistribution was evaluated in xenografted inducted animals.
Results
The results showed that a 189 nm sized nanoparticle were formed with a PDI of 0,097, corroborating the monodispersive behavior. These nanoparticles were successfully radiolabeled with 99mTc showing uptake by the inducted tumor. The MTT assay corroborated the safety of the nanosystem for the cells.
Conclusion
The results support the use of this nanosystem (99mTc-PLA/PVA octreotide nanoparticles) as imaging agent for PPoma.

Polypeptide-Secreting Tumor of the Distal Pancreas (PPoma) Radiolabeled Nanoparticles for Imaging





Similar content being viewed by others
Abbreviations
- AFM:
-
Atomic Force Microscopy
- CO2 :
-
Carbon Dioxide
- DLS:
-
Dynamic Light Scattering
- DMEM:
-
Dulbecco ModifiedEagle’sMinimalEssentialMedium
- EDTA:
-
Ethylenediaminetetraaceticacid
- EE:
-
Entrapment Efficiency
- EPR:
-
Enhanced Permeability and Retention
- FBS:
-
Fetal BovineSerum
- HEPES:
-
N-2 Hydroxyethyl Piperazine-N′-2 Sulfonic Acid Ethane
- ID/organ:
-
Dose per Organ
- IPEN/CNEN:
-
Instituto de Pesquisas Energéticas e Nucleares/Comissão Nacional de Energia Nuclear_Institute of Energy and Nuclear Research/National Nuclear Energy Commission
- μCi :
-
Microcurie
- MBq:
-
Megabecquerel
- MIA PACA-2:
-
Cells from human pancreas carcinoma
- MPS:
-
Mononuclear Phagocytic System
- MTT:
-
3- (4,5-dimethylthiazol-2-yl) -2,5-diphenyltetrazolium bromide
- NaHCO3 :
-
Sodium Bicarbonate
- NET:
-
Neuroendocrine Tumor
- PDI:
-
Polydispersity Index
- PLA:
-
Polylactic Acid
- PP:
-
Pancreatic Polypeptide
- PPoma:
-
Pancreatic Polypeptide-secreting tumor of the distal pancreas
- PVA:
-
Poly(Vinyl Alcohol)
- RPMI:
-
Roswell Park Memorial Institute
- SC:
-
Subcutaneous
- SD:
-
Standard Deviation
- SnCl2 :
-
Stannous Chloride
- SSTR 2:
-
Somatostatin Receptor Subtype 2
- 99mTc:
-
Technetium 99 metastable
- UT:
-
Untreated cells
- W/O:
-
Water/organic emulsion
- W/O/W:
-
Water/organic solvent/water emulsion
References
Brereton MF, Vergari E, Zhang Q, Clark A. Alpha-, Delta- and PP-cells: are they the architectural cornerstones of islet structure and co-ordination? J Histochem Cytochem. 2015;63(8):575–91.
Vinik A, Feliberti Z, Perry RR. Pancreatic Polypeptide (ppoma). In: Feingold KR, Anawalt B, Boyce A, et al., editors. Source Endotext [Internet]. South Dartmouth: mdtext.com; 2017, Jun 12. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279067/. Accessed 18 August 2018.
American Cancer Society. Cancer Facts & Figures 2019. Atlanta: American Cancer Society; 2019.
Instituto Nacional de Câncer José Alencar Gomes da Silva. Dados de incidência e mortalidade. Available from: https://www.inca.gov.br/tipos-de-cancer/cancer-de-pancreas. Accessed 4 March 2019.
Jensen RT. Endocrine tumors of the gastrointestinal tract and pancreas. In: Kasper DL, Braunwald E, Fauci AS, et al., editors. Harrison's principles of internal medicine. New York: Mcgraw-Hill Medical Publishing Division; 2008. p. 2347–58.
Mullan MH, Gauger PG, Thompson NW. Endocrine tumours of the pancreas: review and recent advances. ANZ J Surg. 2001;71(8):475–82.
Oberg K, Eriksson B. Endocrine tumours of the pancreas. Best Pract Res Clin Gastroenterol. 2005;19(5):753–81.
Alexakis N, Neoptolemos JP. Pancreatic neuroendocrine tumours. Best Pract Res Clin Gastroenterol. 2008;22(1):183–205.
Maxwell JE, O’Dorisio TM, Howe JR. Biochemical diagnosis and preoperative imaging of gastroenteropancreatic neuroendocrine tumors. Surg Oncol Clin N Am. 2016;25(1):171–94.
Santos AP. Tumores neuroendócrinos: requesitos mínimos para o diagnóstico clínico. Rev Port Cir. 2011;16(2):28–34.
PRRNT. Practical guidance on peptide receptor radionuclide therapy (PRRNT) for neuendocrinetumours. Vienna: IAEA; 2013.
Ligiero Braga T, Santos-Oliveira R. Ppoma review: epidemiology, aetiopathogenesis, prognosis and treatment. Diseases. 2018;6(8):20.
Barakat MT, Meeran K, Bloom SR. Neuroendocrine tumours. Endocr Relat Cancer. 2004;11:1–18.
Metz DC, Jensen RT. Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology. 2008;135(5):1469–92.
Yao JC, Hoff PM, Hoff AO. Neuroendocrine tumors. New York: Humana Press; 2011. p. 221–43.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Paragliola RM, Salvatori R. Novel somatostatin receptor ligands therapies for acromegaly. Front Endocrinol (Lausanne). 2018;9(78):8.
Papanagnou P, Papadopoulos GE, Stivarou T, Pappas A. Toward fully exploiting the therapeutic potential of marketed pharmaceuticals: the use of octreotide and chloroquine in oncology. Onco Targets Ther. 2018;12:319–39.
Patricio BFC, Albernaz MS, Sarcinelli MA, Carvalho SM, Santos-Oliveira R, Weissmuller G. Development of novel nanoparticle for bone Cancer. J Biomed Nanotechnol. 2014;10(7):1242–8.
Gradiz R, Silva HC, Carvalho L, Botelho MF, Mota-Pinto A. MIA paca-2 and PANC-1 – pancreas ductal adenocarcinoma cell lines with neuroendocrine differentiation and somatostatin receptors. Sci Rep. 2016;6(21648):14.
Moatassim-Billah S, Duluc C, Samain R, Jean C, Perraud A, Decaup E, et al. Anti-metastatic potential of somatostatin analog SOM230: indirect pharmacological targeting of pancreatic cancer-associated fibroblasts. Oncotarget. 2016;7(27):41584–98.
Pinto SR, Helal-Neto E, Paumgartten F, Felzenswalb I, Araujo-Lima CF, Martinez-Manez R, et al. Cytotoxicity, genotoxicity, transplacental transfer and tissue disposition in pregnant rats mediated by nanoparticles: the case of magnetic core mesoporous silica nanoparticles. Artif Cells Nanomed Biotechnol. 2018;46(sup2):527–38.
De Souza Albernaz M, Toma SH, Clanton J, Araki K, Santos-Oliveira R. Decorated superparamagnetic Iron oxide nanoparticles with monoclonal antibody and diethylene-Triamine-Pentaacetic acid labeled with Thechnetium-99m and Galium-68 for breast Cancer imaging. Pharm Res. 2018;35(1):24.
Portilho FL, Pinto SR, de Barros AODS, Helal-Neto E, Dos Santos SN, Bernardes ES, et al. In loco retention effect of magnetic core mesoporous silica nanoparticles doped with trastuzumab as intralesional nanodrug for breast cancer. Artif Cells Nanomed Biotechnol. 2018;46(sup3):S725–33.
Sousa-Batista AJ, Cerqueira-Coutinho C, do Carmo FS, Albernaz MS, Santos-Oliveira R. Polycaprolactone antimony nanoparticles as drug delivery system for Leishmaniasis. Am J Ther. 2019;26(1):e12–7.
Rosa TG, Dos Santos SN, de Jesus Andreoli Pinto T, DDM G, Barja-Fidalgo TC, Ricci-Junior E, et al. Microradiopharmaceutical for metastatic melanoma. Pharm Res. 2017;34(12):2922–30.
Pascual L, Cerqueira-Coutinho C, García-Fernández A, de Luis B, Bernardes ES, Albernaz MS, et al. MUC1 aptamer-capped mesoporous silica nanoparticles for controlled drug delivery and radio-imaging applications. Nanomedicine. 2017;13(8):2495–505.
Ricci-Junior E, de Oliveira de Siqueira LB, RAS R, Sancenon F, Martinez-Manez R, de Moraes JA, et al. Nanocarriers as phototherapeutic drug delivery system: appraisal of three different nanosystems in an in vivo and in vitro exploratory study. Photodiagn Photodyn Ther. 2018;21:43–9.
Oberg K, Kvols L, Caplin M, Delle Fave G, de Herder W, Rindj G, et al. Consensus report on the use of somatostatin analogs for the management of neuroendocrine tumors of the gastroenteropancreatic system. Ann Oncol. 2004;15(6):966–73.
Volante M, Brizzi MP, Faggiano A, La Rosas S, Rapa I, Ferrero A, et al. Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy. Mod Pathol. 2007;20(11):1172–82.
Ito T, Igarashi H, Jensen RT. Pancreatic neuroendocrine tumors: clinical features, diagnosis and medical treatment: advances. Best Pract Res Clin Gastroenterol. 2012;26(6):737–53.
de Jesus Felismino C, Helal-Neto E, Portilho FL, Rocha Pinto S, Sancenon F, Martinez-Manez R, et al. Effect of obesity on biodistribution of nanoparticles. J Control Release. 2018;281:11–8.
Salvi R, Cerqueira-Coutinho C, Ricci-Junior E, Dos Santos SN, Bernardes ES, Barros de Araujo PL, et al. Diagnosing lung cancer using etoposide microparticles labeled with 99mtc. Artif Cells Nanomed Biotechnol. 2018;46(2):341–5.
Benna-Zayani M, Kbir-Ariguib N, Trabelsi-Ayadi M, Grossiord L. Stabilisation of W/O/W double emulsion by polysaccharides as weak gels. Colloids Surf A Physicochem Eng Asp. 2008;316(1–3):46–54.
Mora-Huertas CE, Fessi H, Elaissari A. Polymer-based nanocapsules for drug delivery. Int J Pharm. 2010;385(1–2):113–42.
Danaei M, Dehghankhold M, Ataei S, Hasanzadeh Davarani F, Javanmard R, Dokhani A, et al. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics. 2018;10(57):17.
Schaffazick SR, Guterres SS. Caracterização e estabilidade físico-química de sistemas poliméricosnanoparticulados para administração de fármacos. Quim Nova. 2003;26(5):726–37.
Gaumet M, Vargas A, Gurny R, Delie F. Nanoparticles for drug delivery: the need for precision in reporting particle size parameters. Eur J Pharm Biopharm. 2008;69(1):1–9.
Alexis F, Rhee JW, Richie JP, Radovic-Moreno AF, Langer R, Farokhzad OC. New frontiers in nanotechnology for cancer treatment. Urol Oncol. 2008;26(1):74–85.
Cho K, Wang X, Nie S, Chen ZG, Shin DM. Therapeutic nanoparticles for drug delivery in cancer. Clin Cancer Res. 2008;14(5):1310–6.
Acharya S, Sahoo SK. PLGA nanoparticles containing various anticancer agents and tumour delivery by EPR effect. Adv Drug Deliv Rev. 2011;63(3):170–83.
Oliveira LC, Taveira EJF, Souza LG, Marreto RN, Lima EM, Taveira SF. Aplicações das Nanopartículas Lipídicas no Tratamento de Tumores Sólidos: Revisão de Literatura. Rev Bras Cancerol. 2012;58(4):695–701.
Sadat Tabatabaei Mirakabad F, Nejati-Koshki K, Akbarzadeh A, Yamchi MR, Milanj M, Zarghami N, et al. PLGA-based nanoparticles as cancer drug delivery systems. Asian Pac J Cancer Prev. 2014;15(2):517–35.
Liechty WB, Peppas NA. Expert opinion: responsive polymer nanoparticles in Cancer therapy. Eur J Pharm Biopharm. 2012;80(2):241–6.
SAHA GB. Fundamentals of nuclear pharmacy. New York: Springer Verlag; 2018.
Guimarães TT, Bordim A, Albernaz MS, Santos-Oliveira R. Quality control of radiopharmaceutical 99mtc-MAG3. Lat Am J Pharm. 2011;30(7):1437–9.
Almeida RS, Guimaraes TT, Albernaz MS, Bordim A, Ferro JP, Mamede M, et al. Can quality control of radiopharmaceuticals be done using water and ethanol? Adv Sci Lett. 2012;10(1):140–2.
Alvarez-Lorenzo C, Concheiro A. Smart materials for drug delivery. United Kingdom: Royal Society of Chemistry; 2013.
Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33(9):941–51.
Gustafson HH, Holt-Casper D, Grainger DW, Ghandehari H. Nanoparticle uptake: the phagocyte problem. Nano Today. 2015;10(4):487–510.
Hoshyar N, Gray S, Han H, Bao G. The effect of nanoparticle size on in vivo pharmacokinetics and cellular interaction. Nanomedicine (London). 2016;11(6):673–92.
Li M, Li W, Kim HJ, Yao Q, Chen C, Fisher WE. Characterization of somatostatin receptor expression in human pancreatic cancer using real-time RT-PCR. J Surg Res. 2004;119(2):130–7.
Longmire M, Choyke PL, Kobayashi H. Clearance properties of Nano-sized particles and molecules as imaging agents: considerations and caveats. Nanomedicine (London). 2008;3(5):703–17.
Pinto SR, Sarcinelle MA, de Souza Albernaz M, da Silva FM, Seabra SH, Almeida Nascimento P, et al. In vivo studies: comparing the administration via and the impact on the biodistribution of radiopharmaceuticals. Nucl Med Biol. 2014;41(9):772–4.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Braga, T.L., Pinto, S.R., dos Reis, S.R.R. et al. Octreotide Nanoparticles Showed Affinity for In Vivo MIA Paca-2 Inducted Pancreas Ductal Adenocarcinoma Mimicking Pancreatic Polypeptide-Secreting Tumor of the Distal Pancreas (PPoma). Pharm Res 36, 143 (2019). https://doi.org/10.1007/s11095-019-2678-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-019-2678-4