Abstract
Purpose
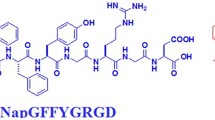
Localized chemotherapy has gained significant impetus for the management of malignant brain tumors. In the present study, we appraised the versatility of an in-situ gel forming self-assembling peptide, ac-(RADA)4-CONH2, as a biocompatible delivery depot of the chemotherapeutic drug doxorubicin (DOX) and the anticancer agent curcumin (CUR), respectively.
Methods
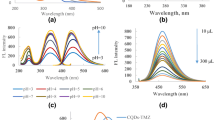
The morphology and mechanical properties of ac-(RADA)4-CONH2 were assessed with scanning electron microscopy (SEM) and rheological studies. The in vitro drug release from ac-(RADA)4-CONH2 was monitored in phosphate-buffered saline pH 7.4. Distribution of the fluorescent actives within the peptide matrix was visualized with confocal laser scanning microscopy (CLSM). The in vitro biological performance of the ac-(RADA)4-CONH2-DOX and ac-(RADA)4-CONH2-CUR was evaluated on the human glioblastoma U-87 MG cell line.
Results
SEM studies revealed that the ac-(RADA)4-CONH2 hydrogel contains an entangled nanofiber network. Rheology studies showed that the more hydrophobic CUR resulted in a stiffer hydrogel compared with ac-(RADA)4-CONH2 and ac-(RADA)4-CONH2-DOX, due to the interaction of CUR with the hydrophobic domains of the peptide nanofibers as confirmed by CLSM. In vitro release studies showed a complete DOX release from ac-(RADA)4-CONH2 within 4 days and a prolonged release for ac-(RADA)4-CONH2-CUR over 20 days. An increased cellular uptake and a higher cytotoxic effect were observed for ac-(RADA)4-CONH2-DOX, compared with DOX solution. Higher levels of early apoptosis were observed for the cells treated with the ac-(RADA)4-CONH2-CUR, compared to CUR solution.
Conclusions
The current findings highlight the potential utility of the in-situ depot forming ac-(RADA)4-CONH2 hydrogel for the local delivery of both water soluble and insoluble chemotherapeutic drugs.








Similar content being viewed by others
Abbreviations
- BBB:
-
Blood brain barrier
- CLSM:
-
Confocal laser scanning microscopy
- CUR:
-
Curcumin
- DOX:
-
Doxorubicin
- GBM:
-
Glioblastoma multiforme
- IC50 :
-
Half-maximal inhibitory concentration
- PBS:
-
Phosphate-buffered saline
- SEM:
-
Scanning electron microscopy
References
Bastiancich C, Danhier P, Préat V, Danhier F. Anticancer drug-loaded hydrogels as drug delivery systems for the local treatment of glioblastoma. J Control Release. 2016;243:29–42.
Stupp R, Brada M, van den Bent MJ, Tonn JC, Pentheroudakis G. High-grade glioma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25:93–101.
Patel DM, Agarwal N, Tomei KL, Hansberry DR, Goldstein IM. Optimal timing of whole-brain radiation therapy following craniotomy for cerebral malignancies. World Neurosurg. 2015;84(2):412–9.
Hervey-Jumper SL, Berger MS. Maximizing safe resection of low- and high-grade glioma. J Neuro-Oncol. 2016;130(2):269–82.
Holland EC. Glioblastoma multiforme: the terminator. Proc Natl Acad Sci U S A. 2000;97(12):6242–4.
Jelsma R, Bucy PC. The treatment of glioblastoma multiforme of the brain. J Neurosurg. 1967;27(5):388–400.
Reardon DA, Wucherpfennig KW, Freeman G, Chiocca EA, Wen PY, Curry WT Jr, et al. An update of vaccine therapy and other immunotherapeutic approaches for glioblastoma. Expert Rev Vaccines. 2014;12(6):597–615.
Karim R, Palazzo C, Evrard B, Piel G. Nanocarriers for the treatment of glioblastoma multiforme: current state-of-the-art. J Control Release. 2016;227:23–37.
Wolinsky JB, Colson YL. Local drug delivery strategies for cancer treatment: gels, nanoparticles, polymeric films, rods and wafers. J Control Release. 2012;159(1):14–26.
Chakroun RW, Zhang P, Lin R, Schiapparelli P, Quinones-Hinojosa A, Cui H. Nanotherapeutic systems for local treatment of brain tumors. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2017;10(1):e1479. https://doi.org/10.1002/wnan.1479.
Tian R, Chen J, Niu R. The development of low-molecular weight hydrogels for applications in cancer therapy. Nano. 2014;6(7):3474–82.
Yu L, Ding J. Injectable hydrogels as unique biomedical materials. Chem Soc Rev. 2008;37(8):1473–81.
Fourniols T, Randolph LD, Staub A, Vanvarenberg K, Leprince JG, Préat V, et al. Temozolomide-loaded photopolymerizable PEG-DMA-based hydrogel for the treatment of glioblastoma. J Control Release. 2015;210:95–104.
Bastiancich C, Vanvarenberg K, Ucakar B, Pitorre M, Bastiat G, Lagarce F, et al. Lauroyl-gemcitabine-loaded lipid nanocapsule hydrogel for the treatment of glioblastoma. J Control Release. 2016;225:283–93.
Tauro JR, Gemeinhart RA. Matrix metalloproteinase triggered delivery of cancer chemotherapy from hydrogel matrixes. Bioconjug Chem. 2005;16(5):1133–9.
Meenach SA, Shapiro JM, Hilt JZ, Anderson KW. Characterization of PEG-iron oxide hydrogel nanocomposites for dual hyperthermia and paclitaxel delivery. J Biomater Sci Polym. 2013;24(9):1112–26.
Tsao CT, Kievit FM, Ravanpay A, Erickson AE, Jensen MC, Ellenbogen RG, et al. Thermoreversible poly(ethylene glycol)-g-chitosan hydrogel as a therapeutic T lymphocyte depot for localized glioblastoma immunotherapy. Biomacromolecules. 2014;15(7):2656–62.
Jain A, Betancur M, Patel GD, Valmikinathan CM, Mukhatyar VJ, Vakharia A, et al. Guiding intracortical brain tumour cells to an extracortical cytotoxic hydrogel using aligned polymeric nanofibres. Nat Mater. 2014;13(3):308–16.
Koutsopoulos S, Unsworth LD, Nagai Y, Zhang SG. Controlled release of functional proteins through designer self-assembling peptide nanofiber hydrogel scaffold. Proc Natl Acad Sci U S A. 2009;106(12):4623–8.
Nagai Y, Unsworth LD, Koutsopoulos S, Zhang S. Slow release of molecules in self-assembling peptide nanofiber scaffold. J Control Release. 2006;115(1):18–25.
Thota CK, Yadav N, Chauhan VS. A novel highly stable and injectable hydrogel based on a conformationally restricted ultrashort peptide. Sci Rep. 2016;6:31167.
Li X, Fu M, Wu J, Zhang CY, Deng X, Dhinakar A, et al. pH-sensitive peptide hydrogel for glucose-responsive insulin delivery. Acta Biomater. 2017;51:294–303.
Kopesky PW, Byun S, Vanderploeg EJ, Kisiday JD, Frisbie DD, Grodzinsky AJ. Sustained delivery of bioactive TGF-beta 1 from self-assembling peptide hydrogels induces chondrogenesis of encapsulated bone marrow stromal cells. J Biomed Mater Res A. 2014;102(5):1275–85.
Liebesny PH, Byun S, Hung HH, Pancoast JR, Mroszczyk KA, Young WT, et al. Growth factor-mediated migration of bone marrow progenitor cells for accelerated scaffold recruitment. Tissue Eng A. 2016;22(13–14):917–27.
Koutsopoulos S. Self-assembling peptide nanofiber hydrogels in tissue engineering and regenerative medicine: progress, design guidelines, and applications. J Biomed Mater Res A. 2016;104(4):1002–16.
Acar H, Srivastava S, Chung EJ, Schnorenberg MR, Barrett JC, LaBelle JL, et al. Self-assembling peptide-based building blocks in medical applications. Adv Drug Deliv Rev. 2017;110-111:65–79.
Cormier AR, Pang X, immerman MI, Zhou HX, Paravastu AK. Molecular structure of RADA16-I designer self-assembling peptide nanofibers. ACS Nano. 2013;7:7562–72.
Momparler RL, Karon M, Siegel SE, Avila F. Effect of adriamycin on DNA, RNA, and protein synthesis in cell-free systems and intact cells. Cancer Res. 1976;36:2891–5.
Sordillo LA, Sordillo PP, Helson L. Curcumin for the treatment of glioblastoma. Anticancer Res. 2015;35(8):6373–8.
Cajot S, Van Butsele K, Paillard A, Passirani C, Garcion E, Benoit JP, et al. Smart nanocarriers for pH-triggered targeting and release of hydrophobic drugs. Acta Biomater. 2012;8(12):4215–23.
Manchun S, Dass CR, Sriamornsak P. Targeted therapy for cancer using pH-responsive nanocarrier systems. Life Sci. 2012;90(11–12):381–7.
Ritger PL, Peppas NA. A simple equation for description of solute release ii. Fickian and anomalous release from swellable devices. J Control Release. 1987;5(1):37–42.
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C, et al. DDSolver: an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010;12(3):263–71.
Altunbas A, Lee SJ, Rajasekaran SA, Schneider JP, Pochan DJ. Encapsulation of curcumin in self-assembling peptide hydrogels as injectable drug delivery vehicles. Biomaterials. 2011;32(25):5906–14.
Liu J, Zhang L, Yang Z, Zhao X. Controlled release of paclitaxel from a self-assembling peptide hydrogel formed in situ and antitumor study in vitro. Int J Nanomedicine. 2011;6:2143–53.
Li I-C, Moore AN, Hartgerink JD. “Missing tooth” multidomain peptide nanofibers for delivery of small molecule drugs. Biomacromolecules. 2016;17:2087–95.
Liu J, Liu J, Xu H, Zhang Y, Chu L, Liu Q, et al. Novel tumor-targeting, self-assembling peptide nanofiber as a carrier for effective curcumin delivery. Int J Nanomedicine. 2014;9:197–207.
Koutsopoulos S, Zhang S. Long-term three-dimensional neural tissue cultures in functionalized self-assembling peptide hydrogels, Matrigel and Collagen I. Acta Biomater. 2013;9(2):5162–9.
Cheng TY, Chen MH, Chang WH, Huang MY, Wang TW. Neural stem cells encapsulated in a functionalized self-assembling peptide hydrogel for brain tissue engineering. Biomaterials. 2013;34(8):2005–16.
Wang X, Wang J, Guo L, Wang X, Chen H, Wang X, et al. Self-assembling peptide hydrogel scaffolds support stem cell-based hair follicle regeneration. Nanomed Nanotechnol Biol Med. 2016;12(7):2115–25.
Koutsopoulos S, Zhang S. Two-layered injectable self-assembling peptide scaffold hydrogels for long-term sustained release of human antibodies. J Control Release. 2012;160(3):451–8.
Zhou A, Chen S, He B, Zhao W, Chen X. Controlled release of TGF-beta 1 from RADA self-assembling peptide hydrogel scaffolds. Drug Des Devel Ther. 2016;10:3043–51.
Karavasili C, Komnenou A, Katsamenis OL, Charalampidou G, Kofidou E, Andreadis D, et al. Self-assembling peptide nanofiber hydrogels for controlled ocular delivery of timolol maleate. ACS Biomater Sci Eng. 2017;3(12):3386–94.
Brosseau N, Andreev E, Ramotar D. Complementation of the yeast model system reveals that caenorhabditis elegans OCT-1 is a functional transporter of anthracyclines. PLoS One. 2015;10(7):e0133182.
Kunwar A, Barik A, Mishra B, Rathinasamy K, Pandey R, Priyadarsini KI. Quantitative cellular uptake, localization and cytotoxicity of curcumin in normal and tumor cells. Biochim Biophys Acta Gen Subj. 2008;1780(4):673–9.
Sun J, Bi C, Chan HM, Sun S, Zhang Q, Zheng Y. Curcumin-loaded solid lipid nanoparticles have prolonged in vitro antitumour activity, cellular uptake and improved in vivo bioavailability. Colloids Surf B Biointerfaces. 2013;111:367–75.
ACKNOWLEDGMENTS AND DISCLOSURES
C.K. is supported by the Onassis Foundation with a PhD scholarship. We thank Orestis L. Katsamenis from μ-VIS X-ray Imaging Centre, Faculty of Engineering and the Environment, University of Southampton, Southampton for the SEM studies. We would like to thank Dr. A. Lazaridou from Department of Food Science and Technology, School of Agriculture, Aristotle University of Thessaloniki, Greece for her assistance in the rheology measurements. The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript.
Corresponding author
Rights and permissions
About this article
Cite this article
Karavasili, C., Panteris, E., Vizirianakis, I.S. et al. Chemotherapeutic Delivery from a Self-Assembling Peptide Nanofiber Hydrogel for the Management of Glioblastoma. Pharm Res 35, 166 (2018). https://doi.org/10.1007/s11095-018-2442-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-018-2442-1