Abstract
Purpose
The ability of human melanotransferrin (hMTf) to carry a therapeutic concentration of trastuzumab (BTA) in the brain after conjugation (in the form of trastuzumab-melanotransferrin conjugate, BT2111 conjugate) was investigated by measuring the reduction of the number and size of metastatic human HER2+ breast cancer tumors in a preclinical model of brain metastases of breast cancer.
Methods
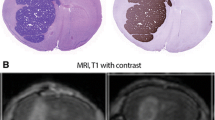
Human metastatic brain seeking breast cancer cells were injected in NuNu mice (n = 6–12 per group) which then developed experimental brain metastases. Drug uptake was analyzed in relation to metastasis size and blood-tumor barrier permeability. To investigate in-vivo activity against brain metastases, equimolar doses of the conjugate, and relevant controls (hMTf and BTA) in separate groups were administered biweekly after intracardiac injection of the metastatic cancer cells.
Results
The trastuzumab-melanotransferrin conjugate (BT2111) reduced the number of preclinical human HER2+ breast cancer metastases in the brain by 68% compared to control groups. Tumors which remained after treatment were 46% smaller than the control groups. In contrast, BTA alone had no effect on reducing number of metastases, and was associated with only a minimal reduction in metastasis size.
Conclusions
The results suggest the novel trastuzumab-melanotransferrin conjugate (BT2111) may have utility in treating brain metastasis and validate hMTf as a potential vector for antibody transport across the Blood Brain Barrier (BBB).




Similar content being viewed by others
Abbreviations
- BBB:
-
Blood brain barrier
- BDT:
-
Brain distant to tumor
- BT2111 BTA-MTf:
-
Antibody trastuzumab-melanotransferrin conjugate
- BTA:
-
Trastuzumab
- BTB:
-
Blood tumor barrier
- CT:
-
Computed tomography
- ER:
-
Estrogen receptor
- FDA:
-
Food and drug administration
- HER2 HER-2/neu or c-erbB-2:
-
Human epidermal growth factor receptor 2
- hMTf:
-
human Melanotransferrin
- Kin :
-
Drug uptake
- LRP:
-
Low density lipoprotein receptor related protein
- MDA-MB-231-Her2:
-
Metastatic brain seeking breast cancer cells
- MNF:
-
Anti-cytokeratin mouse monoclonal IgG antibody
- MRI:
-
Magnetic resonance imaging
- p97:
-
Melanoma tumor antigen
- PBS:
-
Phosphate buffered saline
- Tf:
-
Transferrin
References
Leone JP, Lee AV, Brufsky AM. Prognostic factors and survival of patients with brain metastasis from breast cancer who underwent craniotomy. Cancer Med. 2015;4(7):989–94.
Colzani E, Liljegren A, Johansson AL, Adolfsson J, Hellborg H, Hall PF, et al. Prognosis of patients with breast cancer: causes of death and effects of time since diagnosis, age, and tumor characteristics. J Clin Oncol. 2011;29(30):4014–21.
Zimm S, Wampler GL, Stablein D, Hazra T, Young HF. Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer. 1981;48(2):384–94.
Miller KD, Weathers T, Haney LG, Timmerman R, Dickler M, Shen J, et al. Occult central nervous system involvement in patients with metastatic breast cancer: prevalence, predictive factors and impact on overall survival. Ann Oncol. 2003;14(7):1072–7.
Tsukada Y, Fouad A, Pickren JW, Lane WW. Central nervous system metastasis from breast carcinoma. Autopsy Study Cancer. 1983;52(12):2349–54.
Riihimaki M, Thomsen H, Brandt A, Sundquist J, Hemminki K. Death causes in breast cancer patients. Ann Oncol. 2012;23(3):604–10.
Sanchez-Munoz A, Plata-Fernandez Y, Fernandez M, Jaen-Morago A, Fernandez-Navarro M, de la Torre-Cabrera C, Ramirez-Tortosa C, Pascual J, Alba E, Sanchez-Rovira P. Tumor histological subtyping determined by hormone receptors and HER2 status defines different pathological complete response and outcome to dose-dense neoadjuvant chemotherapy in breast cancer patients. Clin Transl Oncol. 2013.
de la Monte SM, Hutchins GM, Moore GW. Estrogen and progesterone receptors in prediction of metastatic behavior of breast carcinoma. Am J Med. 1984;76(1):11–7.
Knight WA, Livingston RB, Gregory EJ, McGuire WL. Estrogen receptor as an independent prognostic factor for early recurrence in breast cancer. Cancer Res. 1977;37(12):4669–71.
Sugimoto H, Nakagawa T, Sato T, Nagahara M, Ishiba T, Kasahara M, et al. A long-surviving case of HER2-positive breast cancer with brain metastasis treated by multidisciplinary therapy. Gan to Kagaku Ryoho. 2012;39(12):2071–3.
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235(4785):177–82.
Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, et al. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244(4905):707–12.
Park YH, Park MJ, Ji SH, Yi SY, Lim DH, Nam DH, et al. Trastuzumab treatment improves brain metastasis outcomes through control and durable prolongation of systemic extracranial disease in HER2-overexpressing breast cancer patients. Br J Cancer. 2009;100(6):894–900.
Blumenthal GM, Scher NS, Cortazar P, Chattopadhyay S, Tang S, Song P, et al. First FDA approval of dual anti-HER2 regimen: pertuzumab in combination with trastuzumab and docetaxel for HER2-positive metastatic breast cancer. Clin Cancer Res. 2013;19(18):4911–6.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Olson EM, Abdel-Rasoul M, Maly J, Wu CS, Lin NU, Shapiro CL. Incidence and risk of central nervous system metastases as site of first recurrence in patients with HER2-positive breast cancer treated with adjuvant trastuzumab. Ann Oncol. 2013;24(6):1526–33.
Rothenberger S, Food MR, Gabathuler R, Kennard ML, Yamada T, Yasuhara O, et al. Coincident expression and distribution of melanotransferrin and transferrin receptor in human brain capillary endothelium. Brain Res. 1996;712(1):117–21.
Suryo Rahmanto Y, Dunn LL, Richardson DR. The melanoma tumor antigen, melanotransferrin (p97): a 25-year hallmark--from iron metabolism to tumorigenesis. Oncogene. 2007;26(42):6113–24.
Yi X, Manickam DS, Brynskikh A, Kabanov AV. Agile delivery of protein therapeutics to CNS. J Control Release. 2014;190:637–63.
Demeule M, Poirier J, Jodoin J, Bertrand Y, Desrosiers RR, Dagenais C, et al. High transcytosis of melanotransferrin (P97) across the blood-brain barrier. J Neurochem. 2002;83(4):924–33.
Moroo I, Ujiie M, Walker BL, Tiong JW, Vitalis TZ, Karkan D, et al. Identification of a novel route of iron transcytosis across the mammalian blood-brain barrier. Microcirculation. 2003;10(6):457–62.
Karkan D, Pfeifer C, Vitalis TZ, Arthur G, Ujiie M, Chen Q, et al. A unique carrier for delivery of therapeutic compounds beyond the blood-brain barrier. PLoS One. 2008;3(6), e2469.
Demeule M, Regina A, Jodoin J, Laplante A, Dagenais C, Berthelet F, et al. Drug transport to the brain: key roles for the efflux pump P-glycoprotein in the blood-brain barrier. Vasc Pharmacol. 2002;38(6):339–48.
Tang Y, Han T, Everts M, Zhu ZB, Gillespie GY, Curiel DT, et al. Directing adenovirus across the blood-brain barrier via melanotransferrin (P97) transcytosis pathway in an in vitro model. Gene Ther. 2007;14(6):523–32.
biOasis. biOasis’s Herceptin®-BT2111 Stops Human Breast Cancer Tumor Growth in Animals. biOasis Technologies Inc.; Available from: http://www.bioasis.ca/news/2012/120905.htm.
Hutchison R, Vitalis TZ, Gabathuler R. P97-antibody conjugates and methods of use. In. USA: Bioasis Technologies Inc.; 2013. US Patent; WO2013006706 A1, CA2840221A1, CN103747807A, EP2717917A1, EP2717917B1, US9150846, US20130183368, US20160053237.
Charles River Laboratories International I. NU/NU Nude Mouse (Crl:NU-Foxn1nu). Charles River Laboratories International, Inc.; Available from: http://www.criver.com/products-services/basic-research/find-a-model/nu-nu-nude-mouse.
Lockman PR, Mittapalli RK, Taskar KS, Rudraraju V, Gril B, Bohn KA, et al. Heterogeneous blood-tumor barrier permeability determines drug efficacy in experimental brain metastases of breast cancer. Clin Cancer Res. 2010;16(23):5664–78.
Goldstein J, Jerian S, Schechter G, Neeman T, Green MD. FDA clinical review of BLA 98-0369 (Herceptin®, Trastuzumab, rhuMAb HER2). In: Food and Drug Administration (FDA) CfBEaR, editor. Product approval information, licensing action. USA: CBER; 1998. p. 49.
Jay TM, Lucignani G, Crane AM, Jehle J, Sokoloff L. Measurement of local cerebral blood flow with [14C]iodoantipyrine in the mouse. J Cereb Blood Flow Metab. 1988;8(1):121–9.
Williams JL, Shea M, Furlan AJ, Little JR, Jones SC. Importance of freezing time when iodoantipyrine is used for measurement of cerebral blood flow. Am J Physiol. 1991;261(1 Pt 2):H252–6.
de Boer AG, Gaillard PJ. Strategies to improve drug delivery across the blood-brain barrier. Clin Pharmacokinet. 2007;46(7):553–76.
Lillis AP, Van Duyn LB, Murphy-Ullrich JE, Strickland DK. LDL receptor-related protein 1: unique tissue-specific functions revealed by selective gene knockout studies. Physiol Rev. 2008;88(3):887–918.
Olson EM, Najita JS, Sohl J, Arnaout A, Burstein HJ, Winer EP, et al. Clinical outcomes and treatment practice patterns of patients with HER2-positive metastatic breast cancer in the post-trastuzumab era. Breast. 2013;22(4):525–31.
Loi S, de Azambuja E, Pugliano L, Sotiriou C, Piccart MJ. HER2-overexpressing breast cancer: time for the cure with less chemotherapy? Curr Opin Oncol. 2011;23(6):547–58.
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis. 2010;37(1):13–25.
Pestalozzi B, Brignoli S. Traztuzumab in CSF. J Clin Oncol. 2000;18(11):2349–51.
Rossi M, Carioli G, Bonifazi M, Zambelli A, Franchi M, Moja L, et al. Trastuzumab for HER2+ metastatic breast cancer in clinical practice: Cardiotoxicity and overall survival. Eur J Cancer. 2016;52:41–9.
Saini KS, Azim Jr HA, Metzger-Filho O, Loi S, Sotiriou C, de Azambuja E, et al. Beyond trastuzumab: new treatment options for HER2-positive breast cancer. Breast. 2011;20 Suppl 3:S20–7.
Kennard ML, Feldman H, Yamada T, Jefferies WA. Serum levels of the iron binding protein p97 are elevated in Alzheimer’s disease. Nat Med. 1996;2(11):1230–5.
Lambert LA, Perri H, Halbrooks PJ, Mason AB. Evolution of the transferrin family: conservation of residues associated with iron and anion binding. Comp Biochem Physiol B Biochem Mol Biol. 2005;142(2):129–41.
Pardridge WM. Advances in cell biology of blood-brain barrier transport. Semin Cell Biol. 1991;2(6):419–26.
Fillebeen C, Descamps L, Dehouck MP, Fenart L, Benaissa M, Spik G, et al. Receptor-mediated transcytosis of lactoferrin through the blood-brain barrier. J Biol Chem. 1999;274(11):7011–7.
Friden PM, Walus LR. Transport of proteins across the blood-brain barrier via the transferrin receptor. Adv Exp Med Biol. 1993;331:129–36.
Pardridge WM, Eisenberg J, Yang J. Human blood-brain barrier transferrin receptor. Metabolism. 1987;36(9):892–5.
Demeule M, Bertrand Y, Michaud-Levesque J, Jodoin J, Rolland Y, Gabathuler R, et al. Regulation of plasminogen activation: a role for melanotransferrin (p97) in cell migration. Blood. 2003;102(5):1723–31.
Villanueva MT. Drug therapy: smuggling trastuzumab into the brain. Nat Rev Clin Oncol. 2013;10(12):669.
biOasis. Transcend Platform. biOasis Technologies Inc.; 2016 Available from: http://www.bioasis.ca/transcend/.
Sendur MA, Uncu D, Zengin N. Longest progression-free survival with lapatinib and capecitabine combination followed by trastuzumab in HER2-positive brain metastatic breast cancer. Med Oncol. 2014;31(4):890.
Mutlu H, Buyukcelik A. The combination of weekly trastuzumab plus vinorelbine may be preferable regimen in HER-2 positive breast cancer patients with brain metastasis. J Oncol Pharm Pract. 2015;21(4):310–2.
Kodack DP, Chung E, Yamashita H, Incio J, Duyverman AM, Song Y, et al. Combined targeting of HER2 and VEGFR2 for effective treatment of HER2-amplified breast cancer brain metastases. Proc Natl Acad Sci. 2012;109(45):E3119–27.
Tamura K, Kurihara H, Yonemori K, Tsuda H, Suzuki J, Kono Y, et al. 64Cu-DOTA-trastuzumab PET imaging in patients with HER2-positive breast cancer. J Nucl Med. 2013;54(11):1869–75.
Kurihara H, Hamada A, Yoshida M, Shimma S, Hashimoto J, Yonemori K, et al. (64)Cu-DOTA-trastuzumab PET imaging and HER2 specificity of brain metastases in HER2-positive breast cancer patients. EJNMMI Res. 2015;5:8.
Lambert JM, Chari RV. Ado-trastuzumab Emtansine (T-DM1): an antibody-drug conjugate (ADC) for HER2-positive breast cancer. J Med Chem. 2014;57(16):6949–64.
Krop IE, Modi S, LoRusso PM, Pegram M, Guardino E, Althaus B, et al. Phase 1b/2a study of trastuzumab emtansine (T-DM1), paclitaxel, and pertuzumab in HER2-positive metastatic breast cancer. Breast Cancer Res. 2016;18(1):34.
Bartsch R, Berghoff AS, Vogl U, Rudas M, Bergen E, Dubsky P, et al. Activity of T-DM1 in Her2-positive breast cancer brain metastases. Clin Exp Metastasis. 2015;32(7):729–37.
Bergstrom DA, Bodyak N, Yurkovetskiy A, Park PU, DeVit M, Yin M, et al. Abstract LB-231: a novel, highly potent HER2-targeted antibody-drug conjugate (ADC) for the treatment of low HER2-expressing tumors and combination with trastuzumab-based regimens in HER2-driven tumors. Cancer Res. 2015;75(15 Supplement):LB-231.
ACKNOWLEDGMENTS AND DISCLOSURES
This research was supported by grants from the National Cancer Institute (R01CA166067-01A1), Department of Defense Breast Cancer Research Program (W81XWH-062-0033), and BiOasis awarded to P. Lockman. Additional support for this research was provided through the National Institute of General Medical Sciences of the National Institutes of Health (CTSI Award: U54GM104942, and the CoBRE P30 GM103488).
Author information
Authors and Affiliations
Corresponding author
Additional information
Mohamed Ismail Nounou and Chris E. Adkins are both considered as first authors.
Mohamed Ismail Nounou and Chris E. Adkins contributed equally to this work.
Rights and permissions
About this article
Cite this article
Nounou, M.I., Adkins, C.E., Rubinchik, E. et al. Anti-cancer Antibody Trastuzumab-Melanotransferrin Conjugate (BT2111) for the Treatment of Metastatic HER2+ Breast Cancer Tumors in the Brain: an In-Vivo Study. Pharm Res 33, 2930–2942 (2016). https://doi.org/10.1007/s11095-016-2015-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-2015-0