ABSTRACT
Purpose
The main objective of this study was to develop and evaluate therapeutic efficacy and safety following systemic delivery of a peptide analgesic into the CNS using an oil-in-water nanoemulsion system.
Methods
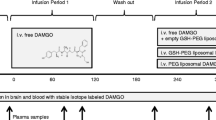
We have formulated a safe and effective, omega-3 rich polyunsaturated fatty acid containing oil-in-water nanoemulsion formulation, for encapsulating and delivering chemically-modified DALDA, a potent mu-opioid peptide analogue, to the CNS. One of the challenges with CNS delivery is the lack of a non-invasive bioanalytical technique to confirm CNS uptake and therapeutic efficacy. Using blood oxygen-level dependent (BOLD) functional magenetic resonance imaging (fMRI), we provide quantitative evidence of nanoemulsion-based delivery and analgesic activity of DALDA analogue in capsaicin-induced awake rat model of pain.
Results
Nanoemulsion formulation effectively encapsulated the modified analgesic peptide and demonstrated efficacy in the capsaicin- pain induced functional magnetic resonance imaging model in rodents. Preliminary safety evaluations show that the nanoemulsion system was well tolerated and did not cause any acute negative effects.
Conclusions
Overall, these results show tremendous opportunity for the development of modified peptide analgesic-encapsulated nanoemulsion formulations for CNS delivery and therapeutic efficacy.






Similar content being viewed by others
REFERENCES
Prokai L. Peptide drug delivery into the central nervous system. Prog Drug Res. 1998;51:95–131.
Wolburg H, Lippoldt A. Tight junctions of the blood-brain barrier: development, composition and regulation. Vasc Pharmacol. 2002;38:323–37.
Shah L, Yadav S, Amiji M. Nanotechnology for CNS delivery of bio-therapeutic agents. Drug Deliv Transl Res. 2013;10:957–72. 3.
Aldrich JV, McLaughlin JP. Opioid peptides: potential for drug development. Drug Discov Today Technol. 2012;9:e23–31.
Pasero C. Introduction. In: Pasero C, McCaffery M, editors. Pain assessment and pharmacologic management. St. Louis: Mosby Inc, Elsevier Inc.; 2011. p. 1–12.
Schiller PW, Nguyen TM, Berezowska I, Dupuis S, Weltrowska G, Chung NN, et al. Synthesis and in vitro opioid activity profiles of DALDA analogues. Eur J Med Chem. 2000;35:895–901.
Farooqui AA. n-3 fatty acid-derived lipid mediators in the brain: new weapons against oxidative stress and inflammation. Curr Med Chem. 2012;19:532–43.
Farooqui AA. Recent development on the neurochemistry of docosanoids. In: Farooqui AA, editor. Lipid mediators and their metabolism in the brain. New York: Springer Science+Business Media, LLC; 2011. p. 49.
Hamilton JA, Brunaldi K. A model for fatty acid transport into the brain. J Mol Neurosci. 2007;33:12–7.
Sarker DK. Engineering of nanoemulsions for drug delivery. Curr Drug Deliv. 2005;2:297–310.
Ganta S, Deshpande D, Korde A, Amiji M. A review of multifunctional nanoemulsion systems to overcome oral and CNS drug delivery barriers. Mol Membr Biol. 2010;27:260–73.
Vyas TK, Shahiwala A, Amiji MM. Improved oral bioavailability and brain transport of Saquinavir upon administration in novel nanoemulsion formulations. Int J Pharm. 2008;347:93–101.
Tiwari SB, Amiji MM. A review of nanocarrier-based CNS delivery systems. Curr Drug Deliv. 2006;3:219–32.
Le B. Looking into the functional architecture of the brain with diffusion MRI. Nat Rev Neurosci. 2003;4:469–80.
Ferris CF, Febo M, Luo F, Schmidt K, Brevard M, Harder JA, et al. Functional magnetic resonance imaging in conscious animals: a new tool in behavioural neuroscience research. J Neuroendocrinol. 2006;18:307–18.
Borsook D, Becerra L, Hargreaves R. Biomarkers for chronic pain and analgesia. Part 1: the need, reality, challenges, and solutions. Discov Med. 2011;11:197–207.
Shah L, Gattacceca F, Amiji MM. CNS delivery and pharmacokinetic evaluations of DALDA analgesic peptide analog administered in nano-sized oil-in-water emulsion formulation. Pharm Res 2013. doi:10.1007/s11095-013-1252-8
Malisza KL, Docherty JC. Capsaicin as a source for painful stimulation in functional MRI. J Magn Reson Imaging. 2001;14:341–7.
McCleskey EW, Gold MS. Ion channels of nociception. Annu Rev Physiol. 1999;61:835–56.
Mogil JS. Animal models of pain: progress and challenges. Nat Rev Neurosci. 2009;10:283–94.
Bie B, Brown DL, Naguib M. Synaptic plasticity and pain aversion. Eur J Pharmacol. 2011;667:26–31.
Ferris CF, Smerkers B, Kulkarni P, Caffrey M, Afacan O, Toddes S, et al. Functional magnetic resonance imaging in awake animals. Rev Neurosci. 2011;22:665–74.
Ferris CF, Stolberg T, Kulkarni P, Murugavel M, Blanchard R, Blanchard DC, et al. Imaging the neural circuitry and chemical control of aggressive motivation. BMC Neurosci. 2008;9:111.
King JA, Garelick TS, Brevard ME, Chen W, Messenger TL, Duong TQ, et al. Procedure for minimizing stress for fMRI studies in conscious rats. J Neurosci Methods. 2005;148:154–60.
Limdi JK, Hyde GM. Evaluation of abnormal liver function tests. Postgrad Med J. 2003;79:307–12.
Gutkowska J, Mukaddam-Daher S, Jankowski M, Schiller PW. The cardiovascular and renal effects of the potent and highly selective mu opioid agonist [Dmt1]DALDA. J Cardiovasc Pharmacol. 2004;44:651–8.
Raboisson P, Dallel R, Clavelou P, Sessle BJ, Woda A. Effects of subcutaneous formalin on the activity of trigeminal brain stem nociceptive neurones in the rat. J Neurophysiol. 1995;73:496–505.
Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9:463–84.
Ganta S, Devalapally H, Amiji M. Curcumin enhances oral bioavailability and anti-tumor therapeutic efficacy of paclitaxel upon administration in nanoemulsion formulation. J Pharm Sci. 2010;99:4630–41.
Sundermann B, Maul C. Opioid peptides. In: Buschmann H, Christoph T, Friderichs E, Maul C, Sundermann B, editors. Analgesics: From chemistry and pharmacology to clinical application. Weinheim: Wiley; 2002. p. 127.
Gauriau C, Bernard JF. Pain pathways and parabrachial circuits in the rat. Exp Physiol. 2002;87:251–8.
Kupers R, Kehlet H. Brain imaging of clinical pain states: a critical review and strategies for future studies. Lancet Neurol. 2006;5:1033–44.
ACKNOWLEDGMENTS AND DISCLOSURES
This study was partially supported by a grant (R21-NS066984) from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. We would like to thank Dr. Jing Xu for her assistance with transmission electron microscopy. Dr. Jerry Lyon at the Tufts University’s Veterinary School is deeply appreciated for his assistance with the tissue histology and analysis. We also appreciate the intellectual feedback from Dr. Anand Subramony of Novartis Institutes for Biomedical Research Inc. to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, L., Kulkarni, P., Ferris, C. et al. Analgesic Efficacy and Safety of DALDA Peptide Analog Delivery to the Brain Using Oil-in-Water Nanoemulsion Formulation. Pharm Res 31, 2724–2734 (2014). https://doi.org/10.1007/s11095-014-1370-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1370-y