ABSTRACT
Purpose
The expression of P-glycoprotein (Pgp) is increased in brain capillary endothelial cells (BCECs) of patients with pharmacoresistant epilepsy. This may restrict the penetration of antiepileptic drugs (AEDs) into the brain. However, the mechanisms underlying increased Pgp expression in epilepsy patients are not known. One possibility is that AEDs induce the expression and functionality of Pgp in BCECs. Several older AEDs that induce human cytochrome P450 enzymes also induce Pgp in hepatocytes and enterocytes, but whether this extends to Pgp at the human BBB and to newer AEDs is not known.
Methods
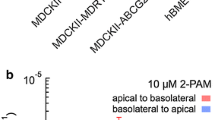
This prompted us to study the effects of various old and new AEDs on Pgp functionality in the human BCEC line, hCMEC/D3, using the rhodamine 123 (Rho123) efflux assay. For comparison, experiments were performed in two rat BCEC lines, RBE4 and GPNT, and primary cultures of rat and pig BCECs. Furthermore, known Pgp inducers, such as dexamethasone and several cytostatic drugs, were included in our experiments.
Results
Under control conditions, GPNT cells exhibited the highest and RBE4 the lowest Pgp expression and Rho123 efflux, while intermediate values were determined in hCMEC/D3. Known Pgp inducers increased Rho123 efflux in all cell lines, but marked inter-cell line differences in effect size were observed. Of the various AEDs examined, only carbamazepine (100 μM) moderately increased Pgp functionality in hCMEC/D3, while valproate (300 μM) inhibited Pgp.
Conclusions
These data do not indicate that treatment with AEDs causes a clinically relevant induction in Pgp functionality in BCECs that form the BBB.








Similar content being viewed by others
Abbreviations
- AEDs:
-
antiepileptic drugs
- ANOVA:
-
analysis of variance
- BBB:
-
blood–brain barrier
- BCEC:
-
brain capillary endothelial cell
- CAR:
-
constitutive androstane receptor
- DMSO:
-
dimethylsulfoxide
- pBCEC:
-
porcine brain capillary endothelial cell
- PBS:
-
phosphate-buffered saline
- Pgp:
-
P-glycoprotein
- PXR:
-
pregnane X receptor
- rBCEC:
-
rat brain capillary endothelial cell
- Rho123:
-
rhodamine 123
- RT:
-
room temperature
References
Schinkel AH. P-Glycoprotein, a gatekeeper in the blood–brain barrier. Adv Drug Deliv Rev. 1999;36:179–94.
Fromm MF. Importance of P-glycoprotein at blood-tissue barriers. Trends Pharmacol Sci. 2004;25:423–9.
Miller DS. Regulation of P-glycoprotein and other ABC drug transporters at the blood–brain barrier. Trends Pharmacol Sci. 2010;31:246–54.
Löscher W, Potschka H. Drug resistance in brain diseases and the role of drug efflux transporters. Nat Rev Neurosci. 2005;6:591–602.
Marquez B, Van Bambeke F. ABC multidrug transporters: target for modulation of drug pharmacokinetics and drug-drug interactions. Curr Drug Targets. 2011;12:600–20.
Lombardo L, Pellitteri R, Balazy M, Cardile V. Induction of nuclear receptors and drug resistance in the brain microvascular endothelial cells treated with antiepileptic drugs. Curr Neurovasc Res. 2008;5:82–92.
Ambroziak K, Kuteykin-Teplyakov K, Luna-Tortós C, Al Falah M, Fedrowitz M, Löscher W. Exposure to antiepileptic drugs does not alter the functionality of P-glycoprotein in brain capillary endothelial and kidney cell lines. Eur J Pharmacol. 2010;628:57–66.
Kullak-Ublick GA, Becker MB. Regulation of drug and bile salt transporters in liver and intestine. Drug Metab Rev. 2003;35:305–17.
Xu C, Li CY, Kong AN. Induction of phase I, II and III drug metabolism/transport by xenobiotics. Arch Pharm Res. 2005;28:249–68.
Urquhart BL, Tirona RG, Kim RB. Nuclear receptors and the regulation of drug-metabolizing enzymes and drug transporters: implications for interindividual variability in response to drugs. J Clin Pharmacol. 2007;47:566–78.
Martin P, Riley R, Back DJ, Owen A. Comparison of the induction profile for drug disposition proteins by typical nuclear receptor activators in human hepatic and intestinal cells. Br J Pharmacol. 2008;153:805–19.
Köhle C, Bock KW. Coordinate regulation of human drug-metabolizing enzymes, and conjugate transporters by the Ah receptor, pregnane X receptor and constitutive androstane receptor. Biochem Pharmacol. 2009;77:689–99.
Chen T. Overcoming drug resistance by regulating nuclear receptors. Adv Drug Deliv Rev. 2010;62:1257–64.
Timsit YE, Negishi M. CAR and PXR: the xenobiotic-sensing receptors. Steroids. 2007;72:231–46.
di Masi A, Marinis ED, Ascenzi P, Marino M. Nuclear receptors CAR and PXR: molecular, functional, and biomedical aspects. Mol Aspects Med. 2009;30:297–343.
Roux F, Durieu-Trautmann O, Chaverot N, Claire M, Mailly P, Bourre JM, et al. Regulation of gamma-glutamyl transpeptidase and alkaline phosphatase activities in immortalized rat brain microvessel endothelial cells. J Cell Physiol. 1994;159:101–13.
Régina A, Romero IA, Greenwood J, Adamson P, Bourre JM, Couraud PO, et al. Dexamethasone regulation of P-glycoprotein activity in an immortalized rat brain endothelial cell line, GPNT. J Neurochem. 1999;73:1954–63.
Weksler BB, Subileau EA, Perrière N, Charneau P, Holloway K, Leveque M, et al. Blood–brain barrier-specific properties of a human adult brain endothelial cell line. FASEB J. 2005;19:1872–4.
Roux F, Couraud PO. Rat brain endothelial cell lines for the study of blood–brain barrier permeability and transport functions. Cell Mol Neurobiol. 2005;25:41–58.
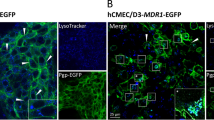
Dauchy S, Miller F, Couraud PO, Weaver RJ, Weksler B, Romero IA, et al. Expression and transcriptional regulation of ABC transporters and cytochromes P450 in hCMEC/D3 human cerebral microvascular endothelial cells. Biochem Pharmacol. 2009;77:897–909.
Demeuse P, Fragner P, Leroy-Noury C, Mercier C, Payen L, Fardel O, et al. Puromycin selectively increases mdr1a expression in immortalized rat brain endothelial cell lines. J Neurochem. 2004;88:23–31.
Male DK. Expression and induction of p-glycoprotein-1 on cultured human brain endothelium. J Cereb Blood Flow Metab. 2009;29:1760–3.
Zastre JA, Chan GN, Ronaldson PT, Ramaswamy M, Couraud PO, Romero IA, et al. Up-regulation of P-glycoprotein by HIV protease inhibitors in a human brain microvessel endothelial cell line. J Neurosci Res. 2009;87:1023–36.
Bachmeier CJ, Beaulieu-Abdelahad D, Ganey NJ, Mullan MJ, Levin GM. Induction of drug efflux protein expression by venlafaxine but not desvenlafaxine. Biopharm Drug Dispos. 2011;32:233–44.
Perloff MD, von Moltke LL, Greenblatt DJ. Ritonavir and dexamethasone induce expression of CYP3A and P-glycoprotein in rats. Xenobiotica. 2004;34:133–50.
Fox E, Bates SE. Tariquidar (XR9576): a P-glycoprotein drug efflux pump inhibitor. Expert Rev Anticancer Ther. 2007;7:447–59.
Weiss J, Kerpen CJ, Lindenmaier H, Dormann SM, Haefeli WE. Interaction of antiepileptic drugs with human P-glycoprotein in vitro. J Pharmacol Exp Ther. 2003;307:262–7.
Perrière N, Demeuse P, Garcia E, Regina A, Debray M, Andreux JP, et al. Puromycin-based purification of rat brain capillary endothelial cell cultures. Effect on the expression of blood–brain barrier-specific properties. J Neurochem. 2005;93:279–89.
Patabendige A, Skinner RA, Abbott NJ. Establishment of a simplified in vitro porcine blood–brain barrier model with high transendothelial electrical resistance. Brain Res. 2013;1521:1–15.
Patabendige A, Skinner RA, Morgan L, Abbott NJ. A detailed method for preparation of a functional and flexible blood–brain barrier model using porcine brain endothelial cells. Brain Res. 2013;1521:16–30.
Smith AJ, Mayer U, Schinkel AH, Borst P. Availability of PSC833, a substrate and inhibitor of P-glycoproteins, in various concentrations of serum. J Natl Cancer Inst. 1998;90:1161–6.
Baltes S, Gastens AM, Fedrowitz M, Potschka H, Kaever V, Löscher W. Differences in the transport of the antiepileptic drugs phenytoin, levetiracetam and carbamazepine by human and mouse P-glycoprotein. Neuropharmacology. 2007;52:333–46.
Baltes S, Fedrowitz M, Luna-Tortós C, Potschka H, Löscher W. Valproic acid is not a substrate for P-glycoprotein or multidrug resistance proteins 1 and 2 in a number of in vitro and in vivo transport assays. J Pharmacol Exp Ther. 2007;320:331–43.
Luna-Tortós C, Fedrowitz M, Löscher W. Several major antiepileptic drugs are substrates for human P-glycoprotein. Neuropharmacology. 2008;55:1364–75.
Efferth T, Lohrke H, Volm M. Reciprocal correlation between expression of P-glycoprotein and accumulation of rhodamine 123 in human tumors. Anticancer Res. 1989;9:1633–7.
Vautier S, Milane A, Fernandez C, Buyse M, Chacun H, Farinotti R. Interactions between antiparkinsonian drugs and ABCB1/P-glycoprotein at the blood–brain barrier in a rat brain endothelial cell model. Neurosci Lett. 2008;442:19–23.
Tai LM, Reddy PS, Lopez-Ramirez MA, Davies HA, Male DK, Loughlin AJ, et al. Polarized P-glycoprotein expression by the immortalised human brain endothelial cell line, hCMEC/D3, restricts apical-to-basolateral permeability to rhodamine 123. Brain Res. 2009;1292:14–24.
Yang L, Fawcett JP, Ostergaard J, Zhang H, Tucker IG. Mechanistic studies of the effect of bile salts on rhodamine 123 uptake into RBE4 cells. Mol Pharm. 2012;9:29–36.
Perrière N, Yousif S, Cazaubon S, Chaverot N, Bourasset F, Cisternino S, et al. A functional in vitro model of rat blood–brain barrier for molecular analysis of efflux transporters. Brain Res. 2007;1150:1–13.
Maines LW, Antonetti DA, Wolpert EB, Smith CD. Evaluation of the role of P-glycoprotein in the uptake of paroxetine, clozapine, phenytoin and carbamazapine by bovine retinal endothelial cells. Neuropharmacology. 2005;49:610–7.
Lee JS, Paull K, Alvarez M, Hose C, Monks A, Grever M, et al. Rhodamine efflux patterns predict P-glycoprotein substrates in the National Cancer Institute drug screen. Mol Pharmacol. 1994;46:627–38.
Löscher W, Luna-Tortos C, Römermann K, Fedrowitz M. Do ATP-binding cassette transporters cause pharmacoresistance in epilepsy? Problems and approaches in determining which antiepileptic drugs are affected. Curr Pharm Des. 2011;17:2808–28.
Zhang C, Kwan P, Zuo Z, Baum L. The transport of antiepileptic drugs by P-glycoprotein. Adv Drug Deliv Rev. 2012;64:930–42.
Robey RW, Honjo Y, van de Laar A, Miyake K, Regis JT, Litman T, et al. A functional assay for detection of the mitoxantrone resistance protein, MXR (ABCG2). Biochim Biophys Acta. 2001;1512:171–82.
Aschner M, Fitsanakis VA, dos Santos AP, Olivi L, Bressler JP. Blood–brain barrier and cell-cell interactions: methods for establishing in vitro models of the blood–brain barrier and transport measurements. Methods Mol Biol. 2006;341:1–15.
Miller DS, Bauer B, Hartz AMS. Modulation of P-glycoprotein at the blood–brain barrier: opportunities to improve CNS pharmacotherapy. Pharmacol Rev. 2008;60:196–209.
Poller B, Drewe J, Krahenbuhl S, Huwyler J, Gutmann H. Regulation of BCRP (ABCG2) and P-glycoprotein (ABCB1) by cytokines in a model of the human blood–brain barrier. Cell Mol Neurobiol. 2010;30:63–70.
Forster C, Burek M, Romero IA, Weksler B, Couraud PO, Drenckhahn D. Differential effects of hydrocortisone and TNFalpha on tight junction proteins in an in vitro model of the human blood–brain barrier. J Physiol. 2008;586:1937–49.
Matheny CJ, Ali RY, Yang X, Pollack GM. Effect of prototypical inducing agents on P-glycoprotein and CYP3A expression in mouse tissues. Drug Metab Dispos. 2004;32:1008–14.
Bauer B, Hartz AM, Fricker G, Miller DS. Pregnane X receptor up-regulation of P-glycoprotein expression and transport function at the blood–brain barrier. Mol Pharmacol. 2004;66:413–9.
Bauer B, Yang X, Hartz AM, Olson ER, Zhao R, Kalvass JC, et al. In vivo activation of human pregnane X receptor tightens the blood–brain barrier to methadone through P-glycoprotein up-regulation. Mol Pharmacol. 2006;70:1212–9.
Wang X, Sykes DB, Miller DS. Constitutive androstane receptor-mediated up-regulation of ATP-driven xenobiotic efflux transporters at the blood–brain barrier. Mol Pharmacol. 2010;78:376–83.
Seegers U, Potschka H, Löscher W. Lack of effects of prolonged treatment with phenobarbital or phenytoin on the expression of P-glycoprotein in various rat brain regions. Eur J Pharmacol. 2002;451:149–55.
Gladding GD, Kupferberg HJ, Swinyard EA. Antiepileptic drug development program. In: Frey H-H, Janz D, editors. Antiepileptic drugs. Berlin: Springer; 1985. p. 341–50.
Cerveny L, Svecova L, Anzenbacherova E, Vrzal R, Staud F, Dvorak Z, et al. Valproic acid induces CYP3A4 and MDR1 gene expression by activation of constitutive androstane receptor and pregnane X receptor pathways. Drug Metab Dispos. 2007;35:1032–41.
Faucette SR, Zhang TC, Moore R, Sueyoshi T, Omiecinski CJ, LeCluyse EL, et al. Relative activation of human pregnane X receptor versus constitutive androstane receptor defines distinct classes of CYP2B6 and CYP3A4 inducers. J Pharmacol Exp Ther. 2007;320:72–80.
Wang X, Hawkins BT, Miller DS. Aryl hydrocarbon receptor-mediated up-regulation of ATP-driven xenobiotic efflux transporters at the blood–brain barrier. FASEB J. 2011;25:644–52.
Xu Y, Jiang Z, Yin P, Li Q, Liu J. Role for class I histone deacetylases in multidrug resistance. Exp Cell Res. 2012;318:177–86.
Eyal S, Lamb JG, Smith-Yockman M, Yagen B, Fibach E, Altschuler Y, et al. The antiepileptic and anticancer agent, valproic acid, induces P-glycoprotein in human tumour cell lines and in rat liver. Br J Pharmacol. 2006;149:250–60.
Narang VS, Fraga C, Kumar N, Shen J, Throm S, Stewart CF, et al. Dexamethasone increases expression and activity of multidrug resistance transporters at the rat blood–brain barrier. Am J Physiol Cell Physiol. 2008;295(2):C440–50.
Lemmen J, Tozakidis IE, Galla HJ. Pregnane X receptor upregulates ABC-transporter Abcg2 and Abcb1 at the blood–brain barrier. Brain Res. 2013;1491:1–13.
Yang HW, Liu HY, Liu X, Zhang DM, Liu YC, Liu XD, et al. Increased P-glycoprotein function and level after long-term exposure of four antiepileptic drugs to rat brain microvascular endothelial cells in vitro. Neurosci Lett. 2008;434:299–303.
Bauer B, Hartz AM, Fricker G, Miller DS. Modulation of P-glycoprotein transport function at the blood–brain barrier. Exp Biol Med (Maywood). 2005;230:118–27.
Giessmann T, May K, Modess C, Wegner D, Hecker U, Zschiesche M, et al. Carbamazepine regulates intestinal P-glycoprotein and multidrug resistance protein MRP2 and influences disposition of talinolol in humans. Clin Pharmacol Ther. 2004;76:192–200.
Löscher W, Langer O. Imaging of P-glycoprotein function and expression to elucidate mechanisms of pharmacoresistance in epilepsy. Curr Top Med Chem. 2010;10:1785–91.
Patsalos PN, Berry DJ, Bourgeois BF, Cloyd JC, Glauser TA, Johannessen SI, et al. Antiepileptic drugs–best practice guidelines for therapeutic drug monitoring: a position paper by the subcommission on therapeutic drug monitoring, ILAE Commission on Therapeutic Strategies. Epilepsia. 2008;49:1239–76.
Acknowledgments and Disclosures
We thank Dr. Pierre-Olivier Couraud (Institut Cochin, Paris, France) for providing hCMEC/D3 cells and Prof. Francoise Roux (INSERM U26, Paris, France) for providing GPNT and RBE4 cells. The study was supported by a grant (Lo 274/10) from the Deutsche Forschungsgemeinschaft (Bonn, Germany). Dana Alms received a PhD scholarship from the FAZIT-Stiftung (Frankfurt am Main, Germany).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alms, D., Fedrowitz, M., Römermann, K. et al. Marked Differences in the Effect of Antiepileptic and Cytostatic Drugs on the Functionality of P-Glycoprotein in Human and Rat Brain Capillary Endothelial Cell Lines. Pharm Res 31, 1588–1604 (2014). https://doi.org/10.1007/s11095-013-1264-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-013-1264-4