No Heading
The esophagus as a site for drug delivery has been much overlooked in comparison to the remainder of the gastrointestinal tract. The low permeability and transient nature of the esophagus means that it is unsuitable for delivery of drugs for systemic action. However, esophageal disorders including fungal infection, cancers, motility dysfunction, and damage due to gastric reflux may be treated using locally acting agents that offer benefits of reduced dosage and decreased side effects. Bioadhesive dosage forms that adhere to the esophageal mucosa and prolong contact have been investigated to improve the efficacy of locally acting agents. The rationale for local esophageal drug delivery and its limitations, the factors that determine adhesion to this organ, and the experimental models used in esophageal drug delivery research are reviewed.
Similar content being viewed by others
References
1. Q. Li, J. A. Castell, and D. O. Castell. Manometric determination of esophageal length. Am. J. Gastroenterol. 89:722–725 (1994).
2. N. Washington, C. Washington, and C. G. Wilson. Oesophageal transit. In N. Washington, C. Washington, and C. G. Wilson (eds.), Physiological Pharmaceutics; Barriers to Drug Absorption, Taylor & Francis, London, 2001, pp. 59–73.
3. S. Kuna. The pH of gastric juice in the normal resting state. Arch. Int. Pharmacodyn. 151:79–97 (1964).
4. P. J. Kahrilas. Functional anatomy and physiology of the esophagus. In: D.O. Castell (ed.), The Esophagus, 2nd ed., Little, Brown, Boston, 1995, pp. 1–28.
5. J. L. O’Neill and T. L. Remington. Drug-induced esophageal injuries and dysphagia. Ann. Pharmacother. 37:1675–1683 (2003).
6. T. A. Woltman, B. K. Oelschlager, and C. A. Pellegrini. Surgical management of esophageal motility disorders. J. Surg. Res. 117:34–43 (2004).
7. J. W. Kikendall, A. C. Friedman, M. A. Oyewole, D. Fleischer, and L. F. Johnson. Pill-induced oesophageal injury: case reports and review of the medical literature. Dig. Dis. Sci. 28:174–182 (1983).
8. S. Nandurkar and N. J. Talley. Epidemiology and natural history of reflux disease. Best Pract. Res. Cl. Ga. 15(5):743–757 (2000).
9. A. Van der Burgh, J. Dees, W. C. J. Hop, and M. van Blankenstein. Oesophageal cancer is an uncommon cause of death in patients with Barrett’s esophagus. Gut 39:5–8 (1996).
10. M. Conio, G. Lapertosa, S. Blanchi, and R. Filiberti. Barrett’s esophagus: an update. Crit. Rev. Oncol. Hematol. 46:187–206 (2003).
11. I. T. Johnson. New approaches to the role of diet in the prevention of cancers of the alimentary tract. Mutat. Res. 551:9–28 (2004).
12. J. P. Moorman. Diagnosis and pharmacotherapy of infectious esophagitis. In G. Friedman, E. D. Jacobson, and R. W. McCallum (eds.), Gastrointestinal Pharmacology and Therapeutics, Lippincott-Raven, New York, 1997 pp. 201–213.
13. Wellmark Report 2003. Available at http://www.wellmark.com/health_improvement/reports/ppi/about.htm#prior (accessed 14/10/2004).
14. C. O. H. Russell, L. D. Hill, E. R. Holmes, D. A. Hull, R. Gannon, and C. E. Pope. Radionuclide transit: a sensitive screening test for esophageal dysfunction. Gastroenterology 80:887–892 (1981).
15. K. T. Evans and G. M. Roberts. The ability of patients to swallow capsules. J. Clin. Hosp. Pharm. 6:207–208 (1981).
16. G. S. McCord and R. E. Clouse. Pill-induced esophageal strictures: clinical features and risk factors for development. Am. J. Med. 88:512–518 (1990).
17. M. Marvola, K. Vahervuo, A. Sothmann, E. Martilla, and M. Rajaniemi. Development of a method for study of the tendency of drug products to adhere to the esophagus. J. Pharm. Sci. 71:975–977 (1982).
18. H. Al-Dujaili, A. T. Florence, and E. G. Salole. The adhesiveness of proprietary tablets and capsules to porcine oesophageal tissue. Int. J. Pharm. 34:75–79 (1986).
19. M. Weinbeck, W. Berges, and H. J. Lubke. Drug-induced oesophageal lesions. Balliere Clin. Gastr. 2:263–274 (1988).
20. O. Honkanen, P. Laaksonen, J. Marvola, S. Eerikainene, R Tuominen, and M. Marvola. Bioavailability and in vitro oesophageal sticking tendancy of hydroxypropyl methylcellulose capsule formulations and corresponding gelatine capsule formulations. Eur. J. Pharm. Sci. 15:479–488 (2002).
21. L. McCargar, D. Crail, R. Dansereau, W. Myers, and M. Lane. The in-vitro porcine adhesion model is not predictive of the esophageal transit of risedronate tablets in humans. Int. J. Pharm. 222:191–197 (2001).
22. D. A. Swisher, S. L. Sendelbeck, and J. W. Fara. Adherence of various oral dosage forms to the esophagus. Int. J. Pharm. 22:219–228 (1984).
23. M. Marvola, M. Rajaniemi, E. Martilla, K. Vahervuo, and A. Sothmann. Effect of dosage form and formulation factors on the adherence of drugs to the esophagus. J. Pharm. Sci. 72:1034–1036 (1983).
24. S. Mathias, S. A. Young, J. Tsibouklis, and J. D. Smart. Adhesion of formulation coatings to the oesophagus: a novel in vitro test system. J. Pharm. Pharmacol. 54:34 (2002).
25. A. C. Perkins, C. G. Wilson, M. Frier, P. E. Blackshaw, R. J. Dansereau, R. M. Vincent, D. Wenderoth, S. Hathaway, Z. Li, and R. C. Spiller. The use of scintigraphy to demonstrate the rapid esophageal transit of the oval film-coated placebo risedronate tablet compared to a round uncoated placebo tablet when administered with minimal volumes of water. Int. J. Pharm. 222:295–303 (2001).
26. O. Honkanen, J. Marvola, H. Kanerva, K. Lindevall, M. Lipponene, T. Kekki, A. Ahonen, and M. Marvola. Gamma scintigraphic evaluation of the fate of hydroxypropyl methyl cellulose capsules in the human gastrointestinal tract. Eur. J. Pharm. Sci. 21:671–678 (2004).
27. M. Sakkinen, J. Marvola, H. Kanerva, K. Lindevall, M. Lipponene, A. Ahonen, and M. Marvola. Scintigraphic verification of adherence of a chitosan formulation to the human oesophagus. Eur. J. Pharm. Biopharm. 57:145–147 (2004).
28. K. S. Channer and J. P. Virdee. The effect of formulation on oesophageal transit. J. Pharm. Pharmacol. 37:126–129 (1985).
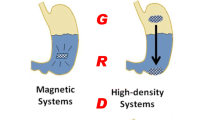
29. R. Ito, Y. Machida, T. Sannan, and T. Nagai. Magnetic granules: a novel system for specific drug delivery to esophageal mucosa in oral administration. Int. J. Pharm. 61:109–117 (1990).
30. V. Vonarx, S. Eleouet, J. Carre, P. Ioss, A. Gouyette, A. M. Leray, C. Merle, Y. Lajat, and T. Patrice. Potential efficacy of a delta 5-aminolevulinic acid bioadhesive gel formulation for the photodynamic treatment of lesions of the gastrointestinal tract in mice. J. Pharm. Pharmacol. 49:652–656 (1997).
31. A. M. Potts, S. Jackson, N. Washington, P. Gilchrist, E. S. Ron, M. Schiller, and C. Wilson. The oesophageal retention of a thermally sensitive hydrogel. J. Pharm. Pharmacol. 49:77 (1997).
32. D. J. Dobrozsi, R. L. Smith, and A. A. Sakr. Comparative mucoretention of sucralfate suspensions in an everted rat esophagus model. Int. J. Pharm. 189:81–89 (1999).
33. H. K. Batchelor, D. Banning, P. W. Dettmar, F. C. Hampson, I. G. Jolliffe, and D. Q. M. Craig. An in vitro mucosal model for prediction of the bioadhesion of alginate solutions to the oesophagus. Int. J. Pharm. 238:123–132 (2002).
34. D. Banning, D. Q. M. Craig, P. W. Dettmar, F. C. Hampson, and E. Onsoyen. An in vitro evaluation of the bioadhesive properties of sodium alginate solution on porcine esophagus. Annual Meeting Abstracts, American Association of Pharmaceutical Scientists. Pharm. Sci. Suppl. 1:S426 (1997).
35. S. A. Young and J. D. Smart. The porcine oesophageal mucoadhesive test system: a novel in vitro apparatus for the evaluation of liquid and semisolid formulations. J. Pharm. Pharmacol. 20:167 (1998).
36. J. D. Smart, R. G. Riley, J. Tsibouklis, S. A. Young, F. C. Hampson, J. A. Davies, G. Kelly, P. W. Dettmar, and W. R. Wilber. The retention of 14 C-labelled poly(acrylic acids) on gastric and oesophageal mucosa: an in vitro study. Eur. J. Pharm. Sci. 20:83–90 (2004).
37. A. M. Potts, B. O’Mahony, J. Foster, C. G. Wilson, and H. N. E. Stevens. The use of magnetic resonance imaging (MRI) to visualise the oesophageal transit of liquid and gel formulations. J. Pharm. Pharmacol. 52:18 (2000).
38. S. A. Mortazavi and J. D. Smart. An investigation of some factors influencing the in vitro assessment of mucoadhesion. Int. J. Pharm. 116:223–230 (1995).
39. J. C. Richardson, P. W. Dettmar, F. C. Hampson, and C. D. Melia. Oesophageal bioadhesion of sodium alginate suspensions: 2. Suspension behaviour on oesophageal mucosa. Eur. J. Pharm. Sci. 23:49–56 (2004).
40. I. D. Hill, P. P. Walters, and D. G. Brown. Ultramulsion based ingestible compositions. U.S. Patent No. 5711936 (1998).
41. R. C. Cuca, K. S. Lienhop, T. C. Riley, M. I. Kirschner, and R. S. Levinson. Long acting GI and esophageal protectant. U.S. Patent No. 5858391 (1999).
42. T. H. Stanley and B. Hague. Non-dissolvable drug-containing dosage-forms for use in the transmucosal delivery of a drug to a patient. U.S. Patent No. 5855908 (1999).
43. S. E. Ron, L. Bromberg, and M. Temchenko. End modified thermal responsive hydrogels. U.S. Patent No. 6316011 (2001).
44. D. J. Dobrozsi. Oral liquid mucoadhesive compounds. U.S. Patent No. 6319513 (2001).
45. P. W. Dettmar, P. A. Dickinson, F. C. Hampson, and I. G. Jolliffe. Compositions for treatment of disorders of the oesophagus. U.S. Patent No. 6610667 (2003).
46. S. I. Pather, J. R. Robinson, J. D. Eichman, R. K. Khankari, J. Honz, and S. V. Gupte. Effervescent drug delivery system for oral administration. U.S. Patent No. 6641838 (2003).
47. P. Iooss, A Gouyette, A. M. LeRay, T. Patrice, and C. Merle. Bioadhesive polymers as platforms for oral Barrett’s oesophagus treatment, formulation and evaluation of various water-soluble bioadhesive polymers. Proceedings 1st World Meeting APGI/APV. APV Press, Budapest, 1995, pp. 829–830.
48. H. Nagano, Y. Machida, M. Iwata, T. Imada, Y. Noguchi, A. Matsumoto, and T. Nagai. Preparation of magnetic granules containing bleomycin and its evaluation using model esophageal cancer. Int. J. Pharm. 147:119–125 (1997).
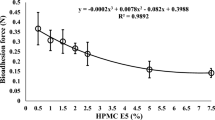
49. H. K. Batchelor, M. Tang, P. W. Dettmar, F. C. Hampson, I. G. Jolliffe, and D. Q. M. Craig. Feasibility of a bioadhesive drug delivery system targeted to oesophageal tissue. Eur. J. Pharm. Biopharm. 57:295–298 (2004).
50. B. Vandergam, D. Gibbs, M. Valtonene, H. Jager, and O. Armignacco. Fluconazole orally dispersible tablets for the treatment of patients with oropharyngeal candidiasis. J. Int. Med. Res. 26:209–218 (1998).
51. L. Zhang and H. K. Batchelor. A bioadhesive formulation for the delivery of anti-fungal agents to the oesophagus. J. Pharm. Pharmacol. 56:44 (2004).
52. J. W. Kikendall and M. H. Mellow. Effect of sublingual nitroglycerin and long-acting nitrate preparations on esophageal motility. Gasteroenterology 79:703–706 (1980).
53. A. M. Potts, G. G. Wilson, H. N. E. Stevens, D. J. Dobrozsi, N. Washington, M. Frier, and A. C. Perkins. Oesophageal bandaging: a new opportunity for thermosetting polymers. STP Pharm. Sci. 10:293–301 (2000).
54. M. Tang, P. W. Dettmar, and H. K. Batchelor. A bioadhesive alginate layer on the oesophagus can reduce damage caused by acid reflux. Proceedings of Pharmaceutical Sciences World Congress, Kyoto, PSWC, Japan, 2004, p. 214.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Batchelor, H. Bioadhesive Dosage Forms for Esophageal Drug Delivery. Pharm Res 22, 175–181 (2005). https://doi.org/10.1007/s11095-004-1183-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-004-1183-5