Abstract
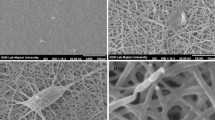
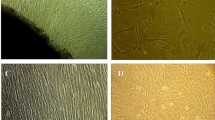
The field of tissue engineering exploits living cells in a variety of ways to restore, maintain, or enhance tissues and organs. Between stem cells, human induced pluripotent stem cells (hiPSCs), are very important due to their wide abilities. Growth factors can support proliferation, differentiation, and migration of hiPSCs. Platelet-rich plasma (PRP) could be used as the source of growth factors for hiPSCs. In the present study, proliferation and neural differentiation of hiPSCs on surface-modified nanofibrous Poly-l-lactic acid (PLLA) coated with platelet-rich plasma was investigated. The results of in vitro analysis showed that on the surface, which was modified nanofibrous scaffolds coated with platelet-rich plasma, significantly enhanced hiPSCs proliferation and neural differentiation were observed. Whereas the MTT ([3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide]) results showed biocompatibility of surface-modified nanofibrous scaffolds coated with platelet-rich plasma and the usage of these modified nanoscaffolds in neural tissue engineering in vivo is promising for the future.





Similar content being viewed by others
Data Availability
Not applicable.
References
Tresco PA (2000) Tissue engineering strategies for nervous system repair. Prog Brain Res 128:349
Stoica BA, Byrnes KR, Faden AI (2009) Cell cycle activation and CNS injury. Neurotox Res 16(3):221–237
Dahlin L (2008) Techniques of peripheral nerve repair. Scand J Surg 97(4):310–316
Cao Q, Benton RL, Whittemore SR (2002) Stem cell repair of central nervous system injury. J Neurosci Res 68(5):501–510
Vacanti JP, Langer R (1999) Tissue engineering: the design and fabrication of living replacement devices for surgical reconstruction and transplantation. Lancet 354:S32–S34
Donaghue IE et al (2014) Cell and biomolecule delivery for tissue repair and regeneration in the central nervous system. J Control Release 190:219–227
Stadtfeld M, Hochedlinger K (2010) Induced pluripotency: history, mechanisms, and applications. Genes Dev 24(20):2239–2263
Pfannkuche K et al (2010) Induced pluripotent stem cells: a new approach for physiological research. Cell Physiol Biochem 26(2):105–124
Kim C (2014) Disease modeling and cell based therapy with iPSC: future therapeutic option with fast and safe application. Blood Res 49(1):7–14
Israel MA et al (2012) Probing sporadic and familial Alzheimer/’s disease using induced pluripotent stem cells. Nature 482(7384):216–220
Soldner F et al (2009) Parkinson’s disease patient-derived induced pluripotent stem cells free of viral reprogramming factors. Cell 136(5):964–977
Zhang N, et al (2010) Characterization of human Huntington’s disease cell model from induced pluripotent stem cells. PLOS Curr Huntingt Dis
Yang J et al (2010) Induced pluripotent stem cells can be used to model the genomic imprinting disorder Prader-Willi syndrome. J Biol Chem 285(51):40303–40311
Murray A et al (2015) Brief report: isogenic induced pluripotent stem cell lines from an adult with mosaic down syndrome model accelerated neuronal ageing and neurodegeneration. Stem Cells 33(6):2077–2084
Hu B-Y et al (2010) Neural differentiation of human induced pluripotent stem cells follows developmental principles but with variable potency. Proc Natl Acad Sci 107(9):4335–4340
Ho SM, Topol A, Brennand KJ (2015) From" directed differentiation" to" neuronal induction": modeling neuropsychiatric disease. Biomark Insights 2015(Suppl. 1):31
Ogawa Y et al (2013) Impaired neural differentiation of induced pluripotent stem cells generated from a mouse model of Sandhoff disease. PLoS ONE 8(1):e55856
Blakeney BA et al (2011) Cell infiltration and growth in a low density, uncompressed three-dimensional electrospun nanofibrous scaffold. Biomaterials 32(6):1583–1590
Mansourizadeh F, Oryan S, Dodel M, Asghari-vostakolaei M (2013) PLLA/HA Nano composite scaffolds for stem cell proliferation and differentiation in tissue engineering. Mol Biol Res Commun 2:1–10
Griffith LG, Naughton G (2002) Tissue engineering–current challenges and expanding opportunities. Science 295(5557):1009–1014
Oberpenning F et al (1999) De novo reconstitution of a functional mammalian urinary bladder by tissue engineering. Nat Biotechnol 17(2):149–155
Yang F et al (2004) Fabrication of nano-structured porous PLLA scaffold intended for nerve tissue engineering. Biomaterials 25(10):1891–1900
Bognitzki M et al (2001) Nanostructured fibers via electrospinning. Adv Mater 13(1):70–72
Lysaght MJ, Reyes J (2001) The growth of tissue engineering. Tissue Eng 7(5):485–493
Domb AJ, Kost J, Wiseman D (1998) Handbook of biodegradable polymers, vol 7. CRC Press, Boca Raton
Vleggaar D, Fitzgerald R, Lorenc ZP (2014) Composition and mechanism of action of poly-L-lactic acid in soft tissue augmentation. J Drugs Dermatol 13(4 Suppl):s29-31
Wu Y-Y et al (2019) Opportunities and challenges for the use of induced pluripotent stem cells in modelling neurodegenerative disease. Open Biol 9(1):180177–180177
Cervelli V, et al (2010) Use of platelet rich plasma and hyaluronic acid on exposed tendons of the foot and ankle. J Wound Care 19(5):186, 188–190.
Shehadat SA et al (2018) Optimization of scanning electron microscope technique for amniotic membrane investigation: a preliminary study. Eur J Dent 12(4):574–578
Halabian R et al (2019) Composite nanoscaffolds modified with bio-ceramic nanoparticles (Zn2SiO4) prompted osteogenic differentiation of human induced pluripotent stem cells. Int J Mol Cell Med 8(1):24
Hejazian LB et al (2012) The role of biodegradable engineered nanofiber scaffolds seeded with hair follicle stem cells for tissue engineering. Iran Biomed J 16(4):193
Wernig M et al (2008) Neurons derived from reprogrammed fibroblasts functionally integrate into the fetal brain and improve symptoms of rats with Parkinson’s disease. Proc Natl Acad Sci 105(15):5856–5861
Mertens J et al (2016) Evaluating cell reprogramming, differentiation and conversion technologies in neuroscience. Nat Rev Neurosci 17(7):424–437
Fawcett JW, Asher RA (1999) The glial scar and central nervous system repair. Brain Res Bull 49(6):377–391
Kim BJ et al (2004) Forskolin promotes astroglial differentiation of human central neurocytoma cells. Exp Mol Med 36(1):52–56
Ruggieri M et al (2014) Induced neural stem cells: methods of reprogramming and potential therapeutic applications. Prog Neurobiol 114:15–24
Tio M et al (2010) Roles of db-cAMP, IBMX and RA in aspects of neural differentiation of cord blood derived mesenchymal-like stem cells. PLoS ONE 5(2):e9398
Zhang L et al (2011) cAMP initiates early phase neuron-like morphology changes and late phase neural differentiation in mesenchymal stem cells. Cell Mol Life Sci 68(5):863–876
Salimi A et al (2014) Comparison of different protocols for neural differentiation of human induced pluripotent stem cells. Mol Biol Rep 41(3):1713–1721
Kim S-S et al (2005) cAMP induces neuronal differentiation of mesenchymal stem cells via activation of extracellular signal-regulated kinase/MAPK. NeuroReport 16(12):1357–1361
Kao H-T et al (2002) A protein kinase A–dependent molecular switch in synapsins regulates neurite outgrowth. Nat Neurosci 5(5):431–437
Sugimoto N et al (2016) Protein kinase A and Epac activation by cAMP regulates the expression of glial fibrillary acidic protein in glial cells. Arch Biol Sci 68(4):795–801
Sanchez C, Dıaz-Nido J, Avila J (2000) Phosphorylation of microtubule-associated protein 2 (MAP2) and its relevance for the regulation of the neuronal cytoskeleton function. Prog Neurobiol 61(2):133–168
Lee MK et al (1990) The expression and posttranslational modification of a neuron-specific β-tubulin isotype during chick embryogenesis. Cell Motil Cytoskelet 17(2):118–132
Farrag TY et al (2007) Effect of platelet rich plasma and fibrin sealant on facial nerve regeneration in a rat model. Laryngoscope 117(1):157–165
Sariguney Y et al (2008) Effect of platelet-rich plasma on peripheral nerve regeneration. J Reconstr Microsurg 24(03):159–167
Zheng C et al (2016) Effect of platelet-rich plasma (PRP) concentration on proliferation, neurotrophic function and migration of Schwann cells in vitro. J Tissue Eng Regen Med 10(5):428–436
Amable PR et al (2013) Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther 4(3):67
Bieback K (2013) Platelet lysate as replacement for fetal bovine serum in mesenchymal stromal cell cultures. Transfus Med Hemother 40(5):326–335
Rauch C et al (2014) Human platelet lysates successfully replace fetal bovine serum in adipose-derived adult stem cell culture. J Adv Biotechnol Bioeng 2:1–11
Basu A et al (2016) Poly (α-hydroxy acid) s and poly (α-hydroxy acid-co-α-amino acid) s derived from amino acid. Adv Drug Deliv Rev 107:82–96
Castro AG, et al (2016) Top-down approach for the preparation of highly porous PLLA microcylinders. ACS Biomater Sci Eng
Narayanan G et al (2016) Poly (lactic acid)-based biomaterials for orthopaedic regenerative engineering. Adv Drug Deliv Rev 107:247–276
Jang S et al (2010) Functional neural differentiation of human adipose tissue-derived stem cells using bFGF and forskolin. BMC Cell Biol 11(1):1
Mansourizadeh F et al (2013) PLLA/HA Nano composite scaffolds for stem cell proliferation and differentiation in tissue engineering. Mol Biol Res Commun 2(1):1–10
Johansson F et al (2006) Axonal outgrowth on nano-imprinted patterns. Biomaterials 27(8):1251–1258
Chow WN et al (2007) Evaluating neuronal and glial growth on electrospun polarized matrices: bridging the gap in percussive spinal cord injuries. Neuron Glia Biol 3(02):119–126
Englund-Johansson U, Netanyah E, Johansson F (2017) Tailor-made electrospun culture scaffolds control human neural progenitor cell behavior—studies on cellular migration and phenotypic differentiation. J Biomater Nanobiotechnol 8:1–21
Yang J, Bei J, Wang S (2002) Improving cell affinity of poly (D, L-lactide) film modified by anhydrous ammonia plasma treatment. Polym Adv Technol 13(3–4):220–226
Nagai A et al (2007) Multilineage potential of stable human mesenchymal stem cell line derived from fetal marrow. PLoS ONE 2(12):e1272
Mahoney MJ, Saltzman WM (2001) Transplantation of brain cells assembled around a programmable synthetic microenvironment. Nat Biotechnol 19(10):934–939
Ardhani R, Susilowati R, Ana ID (2015) Functional recovery of axonal injury induced by gelatin-hydrogel film and PRP: an initial study in rats. J Biomed Sci Eng 8(3):160
Qi C et al (2015) Biomaterials as carrier, barrier and reactor for cell-based regenerative medicine. Protein Cell 6(9):638–653
Schense JC, Hubbell JA (2000) Three-dimensional migration of neurites is mediated by adhesion site density and affinity. J Biol Chem 275(10):6813–6818
Koh H et al (2008) Enhancement of neurite outgrowth using nano-structured scaffolds coupled with laminin. Biomaterials 29(26):3574–3582
Swindle CS et al (2001) Epidermal growth factor (EGF)-like repeats of human tenascin-C as ligands for EGF receptor. J Cell Biol 154(2):459–468
Lee K, Silva EA, Mooney DJ (2011) Growth factor delivery-based tissue engineering: general approaches and a review of recent developments. J R Soc Interface 8(55):153–170
Acknowledgements
The authors thank the Nanobiotechnology Research Center of Baqiyatallah University of Medical Sciences for their valuable contributions to this research.
Funding
There is no funding.
Author information
Authors and Affiliations
Contributions
RM, RH, and MG reviewed the literature, outlined, wrote the manuscript. SEE, ME edited the manuscript and DP prepared figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moazamiyanfar, R., Halabian, R., Ghollasi, M. et al. Neural Differentiation of Human-Induced Pluripotent Stem Cells (hiPSc) on Surface-Modified Nanofibrous Scaffolds Coated with Platelet-Rich Plasma. Neurochem Res 47, 1991–2001 (2022). https://doi.org/10.1007/s11064-022-03584-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-022-03584-2