Abstract
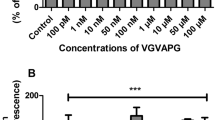
Astrocytes play many distinct roles in the nervous system providing structural support for neurons and maintaining blood-brain barrier integrity. Steroid hormones exhibit a broad spectrum of actions in the central and peripheral nervous system, acting as trophic factors affecting cell differentiation and synaptic plasticity. In steroidogenesis, astrocytes play a key role by producing cholesterol, progesterone (P4), testosterone (T), and estradiol (E2). Currently there are only few studies which show that the Gly-Val-Ala-Pro-Gly (VGVAPG) peptide may affect the metabolism of astrocytes. Therefore, due to the role of neurosteroids, it is necessary to determine whether VGVAPG affects the level of E2, P4, and T in astrocytes. Primary mouse astrocytes were maintained in DMEM/F12 without phenol red, and supplemented with 10% charcoal/dextran-treated fetal bovine serum. Cells were exposed to 10 nM and 1 µM VGVAPG peptide and co-treated with cSrc kinase inhibitor I. After cell stimulation, we measured the Ki67 protein level and the production and secretion of P4, T, and E2. Our report presents the novel finding that the VGVAPG peptide affects the production and secretion of neurosteroids in astrocytes in vitro. The VGVAPG peptide increases the production of P4; however, at the same time, it decreases the secretion of P4 by astrocytes. On the other hand, it stimulates the production and secretion of T. Interestingly, the production of E2 did not change in any studied time interval. The expression of Ki67 protein increased after 48 h of exposition to the VGVAPG peptide. The cSrc kinase inhibitor I prevented most of the effects of VGVAPG peptide. Therefore, we postulate that T and cSrc kinase may be responsible for increasing astrocyte proliferation.




Similar content being viewed by others
Abbreviations
- DMSO:
-
Dimethyl sulfoxide
- EBPs:
-
Elastin-binding protein
- EDPs:
-
Elastin-derived peptides
- FBS:
-
Fetal bovine serum
- VGVAPG–Gly:
-
Val-Ala-Pro-Gly
- BBB:
-
Blood–brain barrier
- E2 :
-
Estradiol
- T:
-
Testosterone
- P4 :
-
Progesterone
References
Verkhratsky A, Nedergaard M, Hertz L (2014) Why are astrocytes important? Neurochem Res.https://doi.org/10.1007/s11064-014-1403-2
Stoffel-Wagner B (2001) Neurosteroid metabolism in the human brain. Eur J Endocrinol 145:669–679. https://doi.org/10.1530/eje.0.1450669
Micevych PE, Chaban V, Ogi J et al (2007) Estradiol stimulates progesterone synthesis in hypothalamic astrocyte cultures. Endocrinology 148:782–789. https://doi.org/10.1210/en.2006-0774
Zwain IH, Yen SS (1999) Neurosteroidogenesis in astrocytes, oligodendrocytes, and neurons of cerebral cortex of rat brain. Endocrinology 140:3843–3852. https://doi.org/10.1210/endo.140.8.6907
Diotel N, Charlier TD, Lefebvre d’Hellencourt C et al (2018) Steroid transport, local synthesis, and signaling within the brain: roles in neurogenesis, neuroprotection, and sexual behaviors. Front Neurosci 12:1–27. https://doi.org/10.3389/fnins.2018.00084
Zwain IH, Yen SS, Cheng CY (1997) Astrocytes cultured in vitro produce estradiol-17beta and express aromatase cytochrome P-450 (P-450 AROM) mRNA. Biochim Biophys Acta 1334:338–348
Ferris HA, Perry RJ, Moreira GV et al (2017) Loss of astrocyte cholesterol synthesis disrupts neuronal function and alters whole-body metabolism. Proc Natl Acad Sci 114:1189–1194. https://doi.org/10.1073/pnas.1620506114
Baeten KM, Akassoglou K (2011) Extracellular matrix and matrix receptors in blood-brain barrier formation and stroke. Dev Neurobiol 71:1018–1039. https://doi.org/10.1002/dneu.20954
Fukuda S, Fini CA, Mabuchi T et al (2004) Focal cerebral ischemia induces active proteases that degrade microvascular matrix. Stroke 35:998–1004. https://doi.org/10.1161/01.STR.0000119383.76447.05
Yamagata K, Tagami M, Takenaga F et al (2004) Hypoxia-induced changes in tight junction permeability of brain capillary endothelial cells are associated with IL-1beta and nitric oxide. Neurobiol Dis 17:491–499. https://doi.org/10.1016/j.nbd.2004.08.001
Agrawal S, Anderson P, Durbeej M et al (2006) Dystroglycan is selectively cleaved at the parenchymal basement membrane at sites of leukocyte extravasation in experimental autoimmune encephalomyelitis. J Exp Med 203:1007–1019. https://doi.org/10.1084/jem.20051342
Baumann E, Preston E, Slinn J, Stanimirovic D (2009) Post-ischemic hypothermia attenuates loss of the vascular basement membrane proteins, agrin and SPARC, and the blood-brain barrier disruption after global cerebral ischemia. Brain Res 1269:185–197. https://doi.org/10.1016/j.brainres.2009.02.062
Cardoso FL, Brites D, Brito MA (2010) Looking at the blood-brain barrier: molecular anatomy and possible investigation approaches. Brain Res Rev 64:328–363. https://doi.org/10.1016/j.brainresrev.2010.05.003
Gutierrez J, Honig L, Elkind MSV et al (2016) Brain arterial aging and its relationship to Alzheimer dementia. Neurology 86:1507–1515. https://doi.org/10.1212/WNL.0000000000002590
Senior RM, Griffin GL, Mecham RP et al (1984) Val-Gly-Val-Ala-Pro-Gly, a repeating peptide in elastin, is chemotactic for fibroblasts and monocytes. J Cell Biol 99:870–874. https://doi.org/10.1083/jcb.99.3.870
Gminski J, Mykala-Ciesla J, Machalski M, Drozdz M (1993) Elastin metabolism parameters in sera of patients with lung cancer. Neoplasma 40:41–44
Blood CH, Sasse J, Brodt P, Zetter BR (1988) Identification of a tumor cell receptor for VGVAPG, an elastin-derived chemotactic peptide. J Cell Biol 107:1987–1993. https://doi.org/10.1083/jcb.107.5.1987
Pocza P, Süli-Vargha H, Darvas Z, Falus A (2008) Locally generated VGVAPG and VAPG elastin-derived peptides amplify melanoma invasion via the galectin-3 receptor. Int J Cancer 122:1972–1980. https://doi.org/10.1002/ijc.23296
Rodgers UR, Weiss AS (2004) Integrin αvβ3 binds a unique non-RGD site near the C-terminus of human tropoelastin. Biochimie 86:173–178. https://doi.org/10.1016/j.biochi.2004.03.002
Lee P, Bax DV, Bilek MMM, Weiss AS (2014) A novel cell adhesion region in tropoelastin mediates attachment to integrin αvβ5. J Biol Chem 289:1467–1477. https://doi.org/10.1074/jbc.M113.518381
Mochizuki S, Brassart B, Hinek A (2002) Signaling pathways transduced through the elastin receptor facilitate proliferation of arterial smooth muscle cells. J Biol Chem 277:44854–44863. https://doi.org/10.1074/jbc.M205630200
Le Page A, Khalil A, Vermette P et al (2019) The role of elastin-derived peptides in human physiology and diseases. Matrix Biol. https://doi.org/10.1016/j.matbio.2019.07.004
Szychowski KA, Gmiński J (2019) Impact of elastin-derived VGVAPG peptide on bidirectional interaction between peroxisome proliferator-activated receptor gamma (Pparγ) and beta-galactosidase (β-Gal) expression in mouse cortical astrocytes in vitro. Naunyn Schmiedebergs Arch Pharmacol 392:405–413. https://doi.org/10.1007/s00210-018-1591-4
Szychowski KA, Gmiński J (2019) The VGVAPG peptide regulates the production of nitric oxide synthases and reactive oxygen species in mouse astrocyte cells in vitro. Neurochem Res 44:1127–1137. https://doi.org/10.1007/s11064-019-02746-z
Szychowski KA, Rombel-Bryzek A, Dołhańczuk-Śródka A, Gmiński J (2019) Antiproliferative effect of elastin-derived peptide VGVAPG on SH-SY5Y neuroblastoma cells. Neurotox Res 36:503–514. https://doi.org/10.1007/s12640-019-00040-y
Szychowski KA, Wójtowicz AK, Gmiński J (2019) Impact of elastin-derived peptide VGVAPG on matrix metalloprotease-2 and – 9 and the tissue inhibitor of metalloproteinase-1, -2, -3 and – 4 mRNA expression in mouse cortical glial cells in vitro. Neurotox Res 35:100–110. https://doi.org/10.1007/s12640-018-9935-x
Garcia-Segura LM, Melcangi RC (2006) Steroids and glial cell function. Glia 54:485–498. https://doi.org/10.1002/glia.20404
Djebaili M, Guo Q, Pettus EH et al (2005) The neurosteroids progesterone and allopregnanolone reduce cell death, gliosis, and functional deficits after traumatic brain injury in rats. J Neurotrauma 22:106–118. https://doi.org/10.1089/neu.2005.22.106
Jones KJ, Kinderman NB, Oblinger MM (1997) Alterations in glial fibrillary acidic protein (GFAP) mRNA levels in the hamster facial motor nucleus: effects of axotomy and testosterone. Neurochem Res 22:1359–1366
Jung-Testas I, Schumacher M, Bugnard H, Baulieu EE (1993) Stimulation of rat Schwann cell proliferation by estradiol: synergism between the estrogen and cAMP. Brain Res Dev Brain Res 72:282–290
Ganter S, Northoff H, Männel D, Gebicke-Härter PJ (1992) Growth control of cultured microglia. J Neurosci Res 33:218–230. https://doi.org/10.1002/jnr.490330205
Si D, Li J, Liu J et al (2014) Progesterone protects blood-brain barrier function and improves neurological outcome following traumatic brain injury in rats. Exp Ther Med 8:1010–1014. https://doi.org/10.3892/etm.2014.1840
Ishrat T, Sayeed I, Atif F et al (2010) Progesterone and allopregnanolone attenuate blood-brain barrier dysfunction following permanent focal ischemia by regulating the expression of matrix metalloproteinases. Exp Neurol 226:183–190. https://doi.org/10.1016/j.expneurol.2010.08.023
Pettus EH, Wright DW, Stein DG, Hoffman SW (2005) Progesterone treatment inhibits the inflammatory agents that accompany traumatic brain injury. Brain Res 1049:112–119. https://doi.org/10.1016/j.brainres.2005.05.004
Stein DG (2008) Progesterone exerts neuroprotective effects after brain injury. Brain Res Rev 57:386–397. https://doi.org/10.1016/j.brainresrev.2007.06.012
Hammond J, Le Q, Goodyer C et al (2001) Testosterone-mediated neuroprotection through the androgen receptor in human primary neurons. J Neurochem 77:1319–1326. https://doi.org/10.1046/j.1471-4159.2001.00345.x
Rubinow DR, Schmidt PJ (1996) Androgens, brain, and behavior. Am J Psychiatry 153:974–984. https://doi.org/10.1176/ajp.153.8.974
Estrada M, Varshney A, Ehrlich BE (2006) Elevated testosterone induces apoptosis in neuronal cells. J Biol Chem 281:25492–25501. https://doi.org/10.1074/jbc.M603193200
Chen Z, Xi G, Mao Y et al (2011) Effects of progesterone and testosterone on ICH-induced brain injury in rats. Acta neurochirurgica. Springer, Vienna, pp 289–293
Nierwińska K, Nowacka-Chmielewska M, Bernacki J et al (2019) The effect of endurance training and testosterone supplementation on the expression of blood spinal cord barrier proteins in rats. PLoS ONE 14:1–14. https://doi.org/10.1371/journal.pone.0211818
Szychowski KA, Gmiński J (2020) Elastin-derived peptide VGVAPG affects the proliferation of mouse cortical astrocytes with the involvement of aryl hydrocarbon receptor (Ahr), peroxisome proliferator-activated receptor gamma (Pparγ), and elastin-binding protein (EBP). Cytokine 126:154930. https://doi.org/10.1016/j.cyto.2019.154930
McCARTHY MMM (2008) Estradiol and the developing brain. Physiol Rev 88:91–134. https://doi.org/10.1152/physrev.00010.2007
Villa A, Vegeto E, Poletti A, Maggi A (2016) Estrogens, neuroinflammation, and neurodegeneration. Endocr Rev 37:372–402. https://doi.org/10.1210/er.2016-1007
Matthews J, Gustafsson J-A (2006) Estrogen receptor and aryl hydrocarbon receptor signaling pathways. Nucl Recept Signal 4:e016. https://doi.org/10.1621/nrs.04016
Safe S, Wormke M (2003) Inhibitory aryl hydrocarbon receptor-estrogen receptor α cross-talk and mechanisms of action. Chem Res Toxicol 16:807–816. https://doi.org/10.1021/tx034036r
Craig ZR, Wang W, Flaws JA (2011) Endocrine-disrupting chemicals in ovarian function: effects on steroidogenesis, metabolism and nuclear receptor signaling. Reproduction 142:633–646. https://doi.org/10.1530/REP-11-0136
Ghotbaddini M, Powell JB (2015) The AhR ligand, TCDD, regulates androgen receptor activity differently in androgen-sensitive versus castration-resistant human prostate cancer cells. Int J Environ Res Public Health 12:7506–7518. https://doi.org/10.3390/ijerph120707506
Endl E, Gerdes J (2000) The Ki-67 protein: fascinating forms and an unknown function. Exp Cell Res 257:231–237. https://doi.org/10.1006/excr.2000.4888
Tajima S, Wachi H, Uemura Y, Okamoto K (1997) Modulation by elastin peptide VGVAPG of cell proliferation and elastin expression in human skin fibroblasts. Arch Dermatol Res 289:489–492. https://doi.org/10.1007/s004030050227
Péterszegi G, Robert AM, Robert L (1996) Presence of the elastin-laminin receptor on human activated lymphocytes. C R Acad Sci III 319:799–803
Devy J, Duca L, Cantarelli B et al (2010) Elastin-derived peptides enhance melanoma growth in vivo by upregulating the activation of Mcol-A (MMP-1) collagenase. Br J Cancer 103:1562–1570. https://doi.org/10.1038/sj.bjc.6605926
Jung S, Rutka JT, Hinek A (1998) Tropoelastin and Elastin Degradation Products Promote Proliferation of Human Astrocytoma Cell Lines. J Neuropathol Exp Neurol 57:439–448. https://doi.org/10.1097/00005072-199805000-00007
Hinek A, Jung S, Rutka JT (1999) Cell surface aggregation of elastin receptor molecules caused by suramin amplified signals leading to proliferation of human glioma cells. Acta Neuropathol 97:399–407
Dutoya S, Lefeèbvre F, Rabaud M, Verna A (2000) Elastin-derived protein coating onto poly(ethylene terephthalate). Technical, microstructural and biological studies. Biomaterials 21:1521–1529. https://doi.org/10.1016/S0142-9612(99)00274-4
Barbosa-Desongles A, Hernández C, Simó R, Selva DM (2013) Testosterone induces cell proliferation and cell cycle gene overexpression in human visceral preadipocytes. Am J Physiol Physiol 305:C355–C359. https://doi.org/10.1152/ajpcell.00019.2013
Bielecki B, Mattern C, Ghoumari AM et al (2016) Unexpected central role of the androgen receptor in the spontaneous regeneration of myelin. Proc Natl Acad Sci 113:14829–14834. https://doi.org/10.1073/pnas.1614826113
Lange CA (2008) Integration of progesterone receptor action with rapid signaling events in breast cancer models. J Steroid Biochem Mol Biol 108:203–212. https://doi.org/10.1016/j.jsbmb.2007.09.019
Liu X, Du L, Feng R (2013) C-Src regulates cell cycle proteins expression through protein kinase B/glycogen synthase kinase 3 beta and extracellular signal-regulated kinases 1/2 pathways in MCF-7 cells. Acta Biochim Biophys Sin (Shanghai) 45:586–592. https://doi.org/10.1093/abbs/gmt042
Migliaccio A, Piccolo D, Castoria G et al (1998) Activation of the Src/p21(ras)/Erk pathway by progesterone receptor via cross-talk with estrogen receptor. EMBO J 17:2008–2018. https://doi.org/10.1093/emboj/17.7.2008
Zhao X, Wu T, Chang CF, et al (2015) Toxic role of prostaglandin E < inf > 2</inf > receptor EP1 after intracerebral hemorrhage in mice. Brain Behav Immun 46:293–310. https://doi.org/10.1016/j.bbi.2015.02.011
Zan L, Wu H, Jiang J et al (2011) Temporal profile of Src, SSeCKS, and angiogenic factors after focal cerebral ischemia: correlations with angiogenesis and cerebral edema. Neurochem Int 58:872–879. https://doi.org/10.1016/j.neuint.2011.02.014
Li P, Chen D, Cui Y et al (2018) Src plays an important role in AGE-induced endothelial cell proliferation, migration, and tubulogenesis. Front Physiol 9:1–14. https://doi.org/10.3389/fphys.2018.00765
Tian H-P, Huang B-S, Zhao J et al (2009) Non-receptor tyrosine kinase Src is required for ischemia-stimulated neuronal cell proliferation via Raf/ERK/CREB activation in the dentate gyrus. BMC Neurosci 10:139. https://doi.org/10.1186/1471-2202-10-139
Jacob MP, Fülöp T, Foris G, Robert L (1987) Effect of elastin peptides on ion fluxes in mononuclear cells, fibroblasts, and smooth muscle cells. Proc Natl Acad Sci U S A 84:995–999. https://doi.org/10.1073/pnas.84.4.995
Faury G, Usson Y, Robert-Nicoud M et al (1998) Nuclear and cytoplasmic free calcium level changes induced by elastin peptides in human endothelial cells. Proc Natl Acad Sci U S A 95:2967–2972. https://doi.org/10.1073/pnas.95.6.2967
Faury G, Garnier S, Weiss AS et al (1998) Action of tropoelastin and synthetic elastin sequences on vascular tone and on free Ca2 + level in human vascular endothelial cells. Circ Res 82:328–336
Coquerel B, Poyer F, Torossian F et al (2009) Elastin-derived peptides: matrikines critical for glioblastoma cell aggressiveness in a 3-D system. Glia 57:1716–1726. https://doi.org/10.1002/glia.20884
Rothhammer V, Quintana FJ (2019) The aryl hydrocarbon receptor: an environmental sensor integrating immune responses in health and disease. Nat Rev Immunol 19:184–197. https://doi.org/10.1038/s41577-019-0125-8
Boonyaratanakornkit V, Scott MP, Ribon V et al (2001) Progesterone receptor contains a proline-rich motif that directly interacts with SH3 domains and activates c-Src family tyrosine kinases. Mol Cell 8:269–280. https://doi.org/10.1016/S1097-2765(01)00304-5
Acknowledgments
This work was supported by statutory funds from the University of Information Technology and Management in Rzeszow, Poland (DS MN 503-05-02-03).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures were approved by the Bioethics Commission (no. 46/2014, First Local Ethical Committee on Animal Testing at the Jagiellonian University in Krakow), as compliant with European Union law.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Szychowski, K.A., Pomianek, T. & Gmiński, J. Elastin-Derived Peptide VGVAPG Affects Production and Secretion of Testosterone in Mouse Astrocyte In Vitro. Neurochem Res 45, 385–394 (2020). https://doi.org/10.1007/s11064-019-02920-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-019-02920-3