Abstract
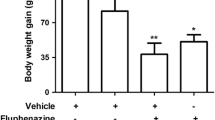
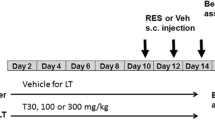
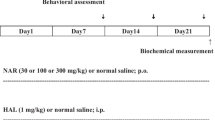
Long-term treatment with fluphenazine is associated with manifestation of extrapyramidal side effects, such as tardive dyskinesia. The molecular mechanisms related to the pathophysiology of TD remain unclear, and several hypotheses, including a role for oxidative stress, have been proposed. Harpagophytum procumbens is an herbal medicine used mainly due to anti-inflammatory effects, but it also exhibits antioxidant effects. We investigated the effect of ethyl acetate fraction of H. procumbens (EAF HP) in fluphenazine-induced orofacial dyskinesia by evaluating behavioral parameters at different times (vacuous chewing movements (VCM’s) and locomotor and exploratory activity), biochemical serological analyses, and biochemical markers of oxidative stress of the liver, kidney, cortex, and striatum. Chronic administration of fluphenazine (25 mg/kg, intramuscular (i.m) significantly increased the VCMs at all analyzed times (2, 7, 14, and 21 days), and this was inhibited by EAF HP (especially at a dose of 30 mg/kg). Fluphenazine decreased locomotion and exploratory activity, and EAF HP did not improve this decrease. Fluphenazine induced oxidative damage, as identified by changes in catalase activity and ROS levels in the cortex and striatum, which was reduced by EAF HP, especially in the striatum. In the cortex, EAF HP was protective against fluphenazine-induced changes in catalase activity but not against the increase in ROS level. Furthermore, EAF HP was shown to be safe, since affected serum biochemical parameters or parameters of oxidative stress in the liver and kidney. These findings suggest that the H. procumbens is a promising therapeutic agent for the treatment of involuntary oral movements.









Similar content being viewed by others
References
Matar HE, Almerie MQ, Sampson S (2013) Fluphenazine (Oral) Versus Placebo for Schizophrenia. Schizophr Bull 39:1187–1188
Park EJ, Amatya S, Kim MS, Park JH, Seol E, Lee H, Shin Y, Hee Na D (2013) Long-acting injectable formulations of antipsychotic drugs for the treatment of schizophrenia. Arch Pharm Res 36:651–659
Lister J, Nobrega JN, Fletcher PJ, Remington G (2014) Oxidative stress and the antipsychotic-induced vacuous chewing movement model of tardive dyskinesia: evidence for antioxidant-based prevention strategies. Psychopharmacology 231:2237–2249
Loonen AJ, Van Praag HM (2007) Measuring movement disorders in antipsychotic drug trials: the need to define a new standard. J Clin Psychopharmacol 27:423–430
Andreassen OA, Jorgensen HA (2000) Neurotoxicity associated with neuroleptic induced oral dyskinesias in rats. Implications for tardive dyskinesia? Prog Neurobiol 61:525–541
Sachdev PS (2000) The current status of tardive dyskinesia. Aust NZ J Psychiat 34:355–369
Lohr JB, Kuczenski R, Niculescu AB (2003) Oxidative mechanisms and tardive dyskinesia. CNS Drugs 17:47–62
Paterson GJ, Ohashi Y, Reynolds GP, Pratt JA, Morris BJ (2006) Selective increases in the cytokine, TNFalpha, in the prefrontal cortex of PCP-treated rats and human schizophrenic subjects: influence of antipsychotic drugs. J. Psychopharmacol 20:636–642
Bishnoi M, Chopra K, Kulkarni SK (2008) Activation of striatal inflammatory mediators and caspase-3 is central to haloperidol-induced orofacial dyskinesia. Eur J Pharmacol 590:241–245
Bishnoi M, Chopra K, Kulkarni SK (2008) Protective effect of Curcumin, the active principle of turmeric (Curcuma longa) in haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes in rat brain. Pharmacol Biochem Behav 88:511–522
Lau YS, Petroske E, Meredith GE, Wang JQ (2003) Elevated neuronal nitric oxide synthase expression in chronic haloperidol-treated rats. Neuropharmacology 45:986–994
Burger ME, Fachinetto R, Zeni G, Rocha JB (2005) Ebselen attenuates haloperidollnduced orofacial dyskinesia and oxidative stress in rat brain. Pharmacol Biochem Behav 81(3):608–615
Fachinetto R, Villarinho JG, Wagner C, Pereira RP, Puntel RL, Paixão MW, Braga AL, Calixto JB, Rocha JB, Ferreira J (2007) Diphenyl diselenide decreases the prevalence of vacuous chewing movements induced by fluphenazine in rats. Psychopharmacology 194:423–432
Nade VS, Kawale LA, Yadav AV (2010) Protective effect of Morus alba leaves on haloperidol-induced orofacial dyskinesia and oxidative stress. Pharm Biol 48:17–22
Daya RP, Tan ML, Sookram CD, Skoblenick K, Mishra RK (2011) Alpha-phenyl-N-tert-butylnitrone prevents oxidative stress in a haloperidol-induced animal model of tardive dyskinesia: investigating the behavioural and biochemical changes. Brain Res 1412:28–36
Busanello A, Peroza LR, Wagner C, Sudati JH, Pereira RP, Prestes Ade S, Rocha JB, Fachinetto R, Barbosa NB (2012) Resveratrol reduces vacuous chewing movements induced by acute treatment with fluphenazine. Pharmacol Biochem Behav 101:307–310
Peroza LR, Busanello A, Leal CQ, Röpke J, Boligon AA, Meinerz D, Libardoni M, Athayde ML, Fachinetto R (2013) Bauhinia forficata prevents vacuous chewing movements induced by haloperidol in rats and has antioxidant potential in vitro. Neurochem Res 38:789–796
Wegener T (2000) Devil’s Claw: from African traditional remedy to modern analgesic and antiinflammatory. Herbal Gram 50:47–54
Gericke N (2012) Plants, products and people” Southern African perspectives. Ethnomed Drug Discov 13:155–162
Grant L, McBean DE, Fyfe L, Warnock AM (2007) A Review of the biological and potential therapeutic actions of Harpagophytum procumbens. Phytother Res 21:199–209
Mncwangi N, Chen W, Vermaak I, Viljoen AM, Gericke N (2012) Devil’s Claw—a review of the ethnobotany, phytochemistry and biological activity of Harpagophytum procumbens. J Ethnopharm 143:755–771
Wegener T, Lupke NP (2003) Treatment of patients with arthrosis of hip or knee with an aqueous extract of devil’s claw (Harpagophytum procumbens DC. Phytother Res 17(10):1165–1172
Mahomed IM, Ojewole JAO (2004) Analgesic, antiinflammatory and antidiabetic properties of Harpagophytum procumbens DC (Pedaliaceae) secondary root aqueous extract. Phytother Res 18:982–989
Kundu J-K, Mossanda KS, Na HK, Surh YJ (2005) Inhibitory effects of the extracts of Sutherlandia frutescens (L.) R.Br.and Harpagophytum procumbens DC. On phorbolester-induced COX-2 expression in mouse skin: AP-1 and CREB as potential upstream targets. Cancer Lett 218:21–31
Huang TH, Tran VH, Duke RK, Tan S, Chrubasik S, Roufogalis BD, Duke CC (2006) Harpagoside suppresses lipopolysaccharide-induced iNOS and COX-2 expression through inhibition of NF-κB activation. J Ethnopharmacol 104:149–155
Warnock M, McBean D, Suter A, Tan J, Whittaker P (2007) Effectiveness and safety of devil’s claw tablets in patients with general rheumatic disorders. Phytoter Res 21:1228–1233
Fiebich BL, Muñoz E, Rose T, Weiss G, McGregor GP (2011) Molecular targets of the antiinflammatory Harpagophytum procumbens (Devil’s claw): inhibition of TNFa and COX-2 gene expression by preventing activation of AP-1. Phytother Res 26(6):806–811
Wachsmuth L, Lindhorst E, Wrubel S, Hadzhiyski H, Hudelmaier M, Eckstein F, Chrubasik S (2011) Micro-morphometrical assessment of the effect of Harpagophytum procumbens extract on articular cartilage inrabbits with experimental osteoarthritis using magnetic resonance imaging. Phytother Res 25(8):1133–1140
Clarkson C, Campbell WE, Smith P (2003) In vitro antiplasmodial activity of abietane and totarane diterpenes isolated from Harpagophytum procumbens (Devil’s Claw). Planta Med 69:720–724
Mahomed IM, Ojewole JAO (2006) Anticonvulsant activity of Harpagophytum procumbens DC [Pedaliaceae] secondary root aqueous extract in mice. Brain Res Bull 69:57–62
Mahomed IM, Ojewole JAO (2009) Uterotonic effect of Harpagophytum procumbens DC (Pedaliaceae) secondary root aqueous extract on rat isolated uterine horns. J Smooth Muscle Res 45:231–239
Uchida S, Hirai K, Hatanaka J, Hanato J, Umegaki K, Yamada S (2008) Antinociceptive effects of St. John’s Wort, Harpagophytum Procumbens extract and grape seed proanthocyanidins extract in mice. Biol Pharm Bull 31:240–245
Georgiev MI, Alipieva K, Orhan IE (2012) Cholinesterases inhibitory and antioxidant activities of Harpagophytum procumbens from in vitro systems. Phytother Res 26:313–316
Schaffer LF, Peroza LR, Boligon AA, Athayde ML, Alves SH, Fachinetto R, Wagner C (2013) Harpagophytum procumbens prevents oxidative stress and loss of cell viability in vitro. Neurochem Res 38:2256–2267
Parenti C, Aricò G, Chiechio S, Di Benedetto G, Parenti R, Scoto GM (2015) Involvement of the heme-oxygenase pathway in the antiallodynic and antihyperalgesic activity of Harpagophytum procumbens in rats. Molecules 20(9):16758–16769
Sun X, Xiong Z, Zhang Y, Meng Y, Xu G, Xia Z, Li J, Zhang R, Ke Z, Xia Z, Hu Y (2012) Harpagoside attenuates MPTP/MPP induced dopaminergic neurodegeneration and movement disorder via elevating glial cell line-derived neurotrophic factor. J Neurochem 120:1072–1083
Bhattacharya A, Bhattacharya S (1998) Anti-oxidant activity of Harpagophytum procumbens. Br J Phytother 5:2
Liang HW, Qiu SF, Shen J, Sun LN, Wang JY, Bruce IC, Xia Q (2008) Genistein attenuates oxidative stress and neuronal damage following transient global cerebral ischemia in rat hippocampus. Neurosci Lett 438:116–120
Babili FE, Fouraste I, Rougaignon C, Moulis C, Chatelain C (2012) Anatomical study of secondary tuberized roots of Harpagophytum procumbens DC and quantification of harpagoside by high-performance liquid chromatography method. Pharmacogn Mag 8:175–180
Boligon AA, Kubiça TF, Mario DN, Brum TF, Piana M, Weiblen R, Lovato L, Alves SH, Santos RCV, Alves CFS, Athayde ML (2013) Antimicrobial and antiviral activity-guided fractionation from Scutia buxifolia Reissek extracts. Acta Physiol Plant 35:2229–2239
Choi CW, Kim SC, Hwang SS, Choi BK, Ahn HJ, Lee MY, Paerk SH, Kim SK (2002) Antioxidant activity and free radical scavenging capacity between Korean medicinal plants and flavonoids by assay-guided comparison. Plant Sci 153:1161–1168
Van Kampen JM, Stoessl AJ (2000) Dopamine D1A receptor function in a rodent model of tardive dyskinesia. Neuroscience 101:629–635
Soulimani R, Younos C, Mortier F, Derrieu C (1994) The role of stomachal digestion on the pharmacological activity of plant extracts, using as an example, extracts of Harpagophytum procumbens. Can J Physiol Pharmacol 72:1532–1536
Chrubasik S, Sporer F, Dillmann-Marschner R, Friedmann A, Wink M (2000) Physicochemical properties of harpagoside and its in vitro release from Harpagophytum procumbens extract tablets. Phytomedicine 6:469–473
Fachinetto R, Villarinho JG, Wagner C, Pereira RP, Avila DS, Burger ME, Calixto JB, Rocha JB, Ferreira J (2007) Valeriana officinalis does not alter the orofacial dyskinesia induced by haloperidol in rats: role of dopamine transporter. Prog Neuropsychopharmacol Biol Psychiatry 31:1478–1486
Fachinetto R, Burger ME, Wagner C, Wondracek DC, Brito VB, Nogueira CW, Ferreira J, Rocha JB (2005) High fat diet increases the incidence of orofacial dyskinesia and oxidative stress in specific brain regions of rats. Pharmacol Biochem Behav 81(3):585–592
Busanello A, Barbosa NB, Peroza LR, Farias LE, Burger ME, Barreto KP, Fachinetto R (2011) Resveratrol protects against a model of vacuous chewing movements induced by reserpine in mice. Behav Pharmacol 22(1):71–75
Reckziegel P, Peroza LR, Schaffer LF, Ferrari MC, Freitas CM, Bürger ME, Fachinetto R (2013) Gallic acid decreases vacuous chewing movements induced by reserpine in rats Pharmacology. Biochem Behav 104:132–137
Röpke J, Busanello A, Leal CQ, de Moraes Reis E, de Freitas CM, Villarinho JG, Figueira FH, Mello CF, Ferreira J, Fachinetto R (2014) Anandamide attenuates haloperidol-induced vacuous chewing movements in rats. Prog Neuropsychopharmacol Biol Psychiatry 3(54):195–199
Broadhurst PL (1960) Experiments in psychogenetics. In: Eysenk HJ (ed) Experiments in personality. Routledge & Kegan Paul, London, p 76
Ohkawa H, Ohishi H, Yagi K (1979) Assay for lipid peroxide in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Pérez-Severiano F, Rodríguez-Pérez M, Pedraza-Chaverrí J, Maldonado PD, Medina-Campos ON, Ortíz-Plata A, Sánchez-García A, Villeda-Hernández J, Galván-Arzate S, Aguilera P, Santamaría A (2004) S-Allylcysteine, a garlic-derived antioxidant, ameliorates quinolinic acid-induced neurotoxicity and oxidative damage in rats. Neurochem Int 45:1175–1183
Aebi H (1984) Catalase in vitro‖ on antioxidative defenses. Methods Enzymol 105:121–127
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Frangou S (2008) Schizophrenia. Psychiatric disorders 36:405–409
Alabed S, Latifeh Y, Mohammad HA, Rifai A (2011) Gamma-aminobutyric acid agonists for neuroleptic-induced tardive dyskinesia. Cochrane Database Syst Rev 13:1–40
Laudahn D, Walper A (2001) Efficacy and tolerance of Harpagophytum Extract LI 174 in patients with chronic non-radicular back pain. Phytother Res 15:621–624
Grant L, McBean DE, Fyfe L, Warnock AM (2009) The inhibition of free radical generation by preparations of Harpagophytum procumbens In Vitro. Phytother Res 23:104–110
Stewart KM, Cole D (2005) The commercial harvest of Devil’s Claw (Harpagophytum spp.) in southern Africa: the devil’s in the details. J Ethnopharmcol 100:225–236
Schimidt AH (2005) Fast HPLC for quality control of Harpagophytum procumbens by using a monolithic silica column: method transfer from conventional particle-based silica column. J Chromatoqr 1073:377–381
Abdelouahad N, Head C (2008) Dermal and transcutaneous delivery of the major glycoside constituents of Harpagophytum procumbens (Devil’s Claw) in vitro. Planta Med 74:527–531
Rice-Evans CA, Miller NJ, Paganga G (1996) Structure–antioxidant activity relationships of flavonoids and phenolic acids. Free Radic Biol Med 20:933–956
Boligon AA, Pereira RP, Feltrin AC, Machado MM, Janovik V, Rocha JB, Athayde ML (2009) Antioxidant activities of flavonol derivatives from the leaves and stem bark of Scutia buxifolia Reiss. Bioresour Technol 100:6592–6598
Son TG, Camandola S, Mattson MP (2008) Hormetic dietary phytochemicals. Neuromolecular Med 10:236–246
Bao J, Huang B, Zou L, Chen S, Zhang C, Zhang Y, Chen M, Wan JB, Su H, Wang Y, He C (2015) Hormetic effect of berberine attenuates the anticancer activity of chemotherapeutic agents. PlosOne 10(9):e0139298. doi:10.1371/journal.pone.0139298
Calabrese EJ, Bachmann KA, Bailer AJ, Bolger PM, Borak J et al (2007) Biological stress response terminology: integrating the concepts of adaptive response and preconditioning stress within a hormetic dose-response framework. Toxicol Appl Pharmacol 222:122–128
Casey DE (2000) Tardive dyskinesia: pathophysiology and animal models. J Clin Psychiat 61(Suppl 4):5–9
Turrone P, Remington G, Nobrega JN (2002) The vacuous chewing movement (VCM) model of tardive dyskinesia revisited: is there a relationship to dopamine D2 receptor occupancy? Neurosci Biobehav 26:361–380
Lerner P, Nose P, Gordon EK, Lovenberg W (1977) Haloperidol: effect of long-term treatment on rat striatal dopamine synthesis and turnover. Science 197:181–183
Spina MB, Cohen G (1989) Dopamine turnover and glutathione oxidation: implications for Parkinson disease. Proc Nat Acad Sci USA 86:1398–1400
Rogoza RM, Fairfax DF, Henry P, N-Marandi S, Khan RF, Gupta SK, Mishra RK (2004) Electron spin resonance spectroscopy reveals alpha-phenyl-N-tert-butylnitrone spin-traps free radicals in rat striatum and prevents haloperidol-induced vacuous chewing movements in the rat model of human tardive dyskinesia. Synapse 54:156–163
Lohr JB, Kuczenski R, Bracha HS, Moir M, Jeste DV (1990) Increased indices of free radical activity in the cerebrospinal fluid of patients with tardive dyskinesia. Biol Psychiatry 28:535–539
Tsai L, Ikonomidou C (1995) Toward an understanding of tardive dyskinesia: chronic haloperidol enhances NMDA toxicity in mouse striatum. Soc Neurosci Abstr 1721:1744
Brown K, Reid A, White T, Hukin S, Jonhstone C, Glen A (1998) Vitamin E, lipids, and lipid peroxidation products in tardive dyskinesia. Biol Psychiatry 43:863–867
Flatow J, Buckley P, Miller BJ (2013) Meta-analysis of oxidative stress in schizophrenia. Biol Psychiat 74:400–409
Merrill RM, Lyon JL, Matiaco PM (2013) Tardive and spontaneous dyskinesia in the general population. BMC Psychiatry 13:152
Egan MF, Hyde TM, Albers GW, Elkashef A, Alexander RC, Reeve A, Blum A, Saenz RE, Wyatt RJ (1992) Treatment of tardive dyskinesia with vitamin E. Am J Psychiatry 149:773–777
Adler LA, Peselow E, Rotrosen J, Duncam E, Lee M, Rosenthal BA, Angrist B (1993) Vitamine E treatment of tardive dyskinesia. Am J Psychiatry 150:1405–1407
Pathan AA, Mohan M, Kasture AS, Kasture SB (2011) Mucuna pruriens attenuates haloperidol-induced orofacial dyskinesia in rats. Nat Prod Res 25:764–771
Patil R, Hiray Y, Shinde S, Langade P (2012) Reversal of haloperidolinduced orofacial dyskinesia by Murraya koenigii leaves in experimental animals. Pharm Biol 50:691–697
Chaudière J, Ferrari-iliou R (1999) Intracellular antioxidants: from chemical to biochemical mechanisms. Food Chem Toxicol 37:949–962
Calabrese EJ, Canada AT (1989) Catalase: its role in xenobiotic detoxification. Pharmac Ther 44:297–307
Fernandes VS, Santos JR, Leão AHFF, Medeiros AM, Melo TG, Izídio GS, Cabral A, Ribeiro RA, Abílio VC, Ribeiro AM, Silva RH (2012) Repeated treatment with a low dose of reserpine as a progressive model of Parkinson’s disease. Behav Brain Res 231:154–163
Kelley AE, Bakshi VP, Delfs JM, Lang CG (1989) Cholinergic stimulation of the ventrolateral striatum elicits mouth movements in rats: pharmacological and regional specificity. Psychopharmacology 99:542–549
Salamone JD, Ishiwari K, Betz AJ, Farrar AM, Mingote SM, Font L, Hockemeyer J, Müller CE, Correa M (2008) Dopamine/adenosine interactions related to locomotion and tremor in animal models: possible relevance to parkinsonism. Parkinsonism Relat Disord 2(Suppl):S130–S134
Acknowledgments
Coordination of Improvement of Higher Education Personnel (CAPES), National Council for Scientific and Technological Development (CNPq - Universal - 475210/2013-1), Foundation for Research of the State of Rio Grande do Sul (FAPERGS- PRONEM #11/2029-1 and PqG - 2080-2551/13-5), Department of Science and Technology (DECIT), and Secretariat of Science and Technology and Strategic Inputs. R.F. has received fellowship from CNPq. L.F.S.,C.M.F., A.P.C., L.R.P., E.M.R., B.N.K., and A.B. are recipient of fellowships from CAPES. Sincere posthumous thanks to our beloved professor in memorian Margareth Linde Athayde.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Schaffer, L.F., de Freitas, C.M., Chiapinotto Ceretta, A.P. et al. Harpagophytum Procumbens Ethyl Acetate Fraction Reduces Fluphenazine-Induced Vacuous Chewing Movements and Oxidative Stress in Rat Brain. Neurochem Res 41, 1170–1184 (2016). https://doi.org/10.1007/s11064-015-1811-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-015-1811-y