Abstract
Purpose
The postoperative period after laser interstitial thermal therapy (LITT) is marked by a temporary increase in volume, which can impact the accuracy of radiographic assessment. The current criteria for progressive disease (PD) suggest that a 20% increase in size of brain metastasis (BM) assessed in 6–12 weeks intervals should be considered as local progression (LP). However, there is no agreement on how LP should be defined in this context. In this study, we aimed to statistically analyze which tumor volume variations were associated with LP.
Methods
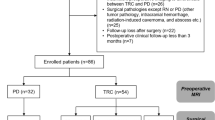
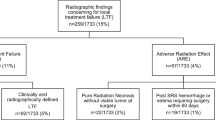
We analyzed 40 BM that underwent LITT between 2013 and 2022. For this study, LP was defined following radiographic features. A ROC curve was generated to evaluate volume change as a predictor of LP and find the optimal cutoff point. A logistic regression analysis and Kaplan Meier curves were performed to assess the impact of various clinical variables on LP.
Results
Out of 40 lesions, 12 (30%) had LP. An increase in volume of 25.6% from baseline within 120–180 days after LITT presented a 70% sensitivity and 88.9% specificity for predicting LP (AUC: 0.78, p = 0.041). The multivariate analysis showed a 25% increase in volume between 120 and 180 days as a negative predictive factor (p = 0.02). Volumetric changes within 60–90 days after LITT did not predict LP (AUC: 0.57; p = 0.61).
Conclusion
Volume changes within the first 120 days after the procedure are not independent indicators of LP of metastatic brain lesions treated with LITT.


Similar content being viewed by others
Data Availability
Data will be made available upon reasonable request.
References
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. Cancer J Clin 73(1):17–48
Levy C et al (2014) REBECA: a phase I study of bevacizumab and whole-brain radiation therapy for the treatment of brain metastasis from solid tumours. Ann Oncol 25(12):2351–2356
Olson JJ, Kalkanis SN, Ryken TC (2019) Congress of neurological surgeons systematic review and evidence-based guidelines for the treatment of adults with metastatic brain tumors: executive summary, Neurosurgery, vol. 84, no. 3, pp. 550–552
Jethwa PR, Barrese JC, Gowda A, Shetty A, Danish SF (2012) Magnetic resonance thermometry-guided laser-induced thermal therapy for intracranial neoplasms: initial experience, Operative Neurosurg, vol. 71, no. suppl_1, pp. ons133-ons145
Salem U et al (2019) Neurosurgical applications of MRI guided laser interstitial thermal therapy (LITT). Cancer Imaging 19(1):1–13
Shah AH et al (2020) The role of laser interstitial thermal therapy in surgical neuro-oncology: series of 100 consecutive patients, Neurosurgery, vol. 87, no. 2, pp. 266–275
Eichberg DG, VanDenBerg R, Komotar RJ, Ivan ME (2018) Quantitative volumetric analysis following magnetic resonance–guided laser interstitial thermal ablation of cerebellar metastases. World Neurosurg 110:e755–e765
Lin NU et al (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16(6):e270–e278
Carpentier A et al (2011) Laser thermal therapy: real-time MRI‐guided and computer‐controlled procedures for metastatic brain tumors. Lasers Surg Med 43(10):943–950
Ahluwalia M et al (2018) Laser ablation after stereotactic radiosurgery: a multicenter prospective study in patients with metastatic brain tumors and radiation necrosis. J Neurosurg 130(3):804–811
Rubino F et al (2022) Robotic guidance platform for laser interstitial thermal ablation and stereotactic needle biopsies: a single center experience. J robotic Surg 16(3):549–557
Levy AS et al (2023) Development of an enhanced recovery protocol after laser ablation surgery protocol: a preliminary analysis, Neuro-Oncology Pract p. npad007
Merenzon MA et al (2022) Newly diagnosed adult basal ganglia gliomas treated with laser interstitial thermal therapy: a comparative cohort with needle biopsy, Operative Neurosurgery, p. 10.1227
Sun G-W, Shook TL, Kay GL (1996) Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol 49(8):907–916
Sankey EW et al (2022) Time to steroid independence after laser interstitial thermal therapy vs medical management for treatment of biopsy-proven radiation necrosis secondary to stereotactic radiosurgery for brain metastasis, Neurosurgery, vol. 90, no. 6, pp. 684–690
Sujijantarat N et al (2020) Laser interstitial thermal therapy (LITT) vs. bevacizumab for radiation necrosis in previously irradiated brain metastases. J Neurooncol 148:641–649
de Almeida Bastos DC et al (2020) Predictors of local control of brain metastasis treated with laser interstitial thermal therapy, Neurosurgery, vol. 87, no. 1, pp. 112–122
Rao MS, Hargreaves EL, Khan AJ, Haffty BG, Danish SF (2014) Magnetic resonance-guided laser ablation improves local control for postradiosurgery recurrence and/or radiation necrosis, Neurosurgery, vol. 74, no. 6, pp. 658–667
Chaunzwa TL et al (2018) Laser thermal ablation for metastases failing radiosurgery: a multicentered retrospective study, Neurosurgery, vol. 82, no. 1, pp. 56–63
Alattar AA et al (2019) Stereotactic laser ablation as treatment of brain metastases recurring after stereotactic radiosurgery: a systematic literature review. World Neurosurg 128:134–142
Wen PY et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28(11):1963–1972
Okada H et al (2015) Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol 16(15):e534–e542
Beechar VB et al (2018) Volumetric response of progressing post-SRS lesions treated with laser interstitial thermal therapy, Journal of Neuro-oncology, vol. 137, pp. 57–65,
Funding
This study did not receive any funding or financial support.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception or design of the work: A.H.S., M.E.I., M.A.M., R.J.K. Acquisition, analysis, or interpretation of data for the work: M.A.M., A. S., A.S.L., S.B., C.R., A.S., A.A.M., L.C.D., E.L. Drafting the work: M.A.M., A. S., A.S.L., S.B., C.R. Revising it critically for important intellectual content: M.A.M., A.S.L., S.B., C.R., A.A.M., L.C.D., E.L., R.J.K., A.H.S., M.E.I. Final approval of the version to be published: M.A.M., A.S.L., S.B., C.R., A.A.M., A.S., L.C.D., E.L., R.J.K., A.H.S., M.E.I. Agreement to be accountable for all aspects of the work: M.A.M., A.S.L., S.B., C.R., A.A.M., A.S., L.C.D., E.L., R.J.K., A.H.S., M.E.I.
Corresponding author
Ethics declarations
Competing interests
M Ivan is a consultant and grant recipient from Medtronic. The other authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Financial interests
M Ivan is a consultant and grant recipient from Medtronic. The other authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merenzon, M.A., Levy, A.S., Bhatia, S. et al. Towards the definition of progressive disease in brain metastasis treated with laser ablation: an evidence-based study. J Neurooncol 163, 463–471 (2023). https://doi.org/10.1007/s11060-023-04360-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04360-0