Abstract
Introduction
Glioblastoma (GBM) is an aggressive primary brain cancer. Lack of effective therapy is related to its highly invasive nature. GBM invasion has been studied with reductionist systems that do not fully recapitulate the cytoarchitecture of the brain. We describe a human-derived brain organotypic model to study the migratory properties of GBM IDH-wild type ex vivo.
Methods
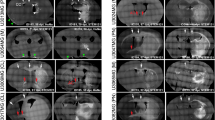
Non-tumor brain samples were obtained from patients undergoing surgery (n = 7). Organotypic brain slices were prepared, and green fluorescent protein (GFP)-labeled primary human GBM IDH-wild type cells (GBM276, GBM612, GBM965) were placed on the organotypic slice. Migration was evaluated via microscopy and immunohistochemistry.
Results
After placement, cells migrated towards blood vessels; initially migrating with limited directionality, sending processes in different directions, and increasing their speed upon contact with the vessel. Once merged, migration speed decreased and continued to decrease with time (p < 0.001). After perivascular localization, migration is limited along the blood vessels in both directions. The percentage of cells that contact blood vessels and then continue to migrate along the vessel was 92.5% (− 3.9/ + 2.9)% while the percentage of cells that migrate along the blood vessel and leave was 7.5% (− 2.9/ + 3.9) (95% CI, Clopper-Pearson (exact); n = 256 cells from six organotypic cultures); these percentages are significantly different from the random (50%) null hypothesis (z = 13.6; p < 10–7). Further, cells increase their speed in response to a decrease in oxygen tension from atmospheric normoxia (20% O2) to anoxia (1% O2) (p = 0.033).
Conclusion
Human organotypic models can accurately study cell migration ex vivo. GBM IDH-wild type cells migrate toward the perivascular space in blood vessels and their migratory parameters change once they contact vascular structures and under hypoxic conditions. This model allows the evaluation of GBM invasion, considering the human brain microenvironment when cells are removed from their native niche after surgery.
Graphical Abstract






Similar content being viewed by others
Data availability
Not applicable.
References
Marenco-Hillembrand L, Wikjesekera O, Suarez-Meade P, Mampre D, Jackson C, Peterson J, Trifiletti D, Hammack J, Ortiz K, Lesser E, Spiegel M, Prevatt C, Hawayek M, Quinones-Hinojosa A, Chaichana K (2020) Trends in Glioblastoma: outcomes over time and type of intervention: a systematic evidence based analysis. J Neuro-Oncol 147:297–307
Stupp R, Mason WP, Van Den Bent MJ, Wller M, Fischer B, Taphoorn MJB, Belanger K, Brandea AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacomber D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups National Cancer Institute of Canada Clinical Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Eng J Med 352(10):987–996
Chaichana KL, Jusue-Torres I, Navarro-Ramirez R, Raza SM, Pascual-Gallego M, Ibrahim A, Hernandez-Hermann M, Gomez L, Ye X, Weingart JD, Olivi A, Blakeley J, Gallia GL, Lim M, Brem H, Quinones-Hinojosa A (2014) Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol 16(1):113–122
Okolie O, Bago JR, Schmid RS, Irvin DM, Bash RE, Miller CR, Hingtgen SD (2016) Reactive astrocytes potentiate tumor aggressiveness in a murine glioma resection and recurrence model. Neuro Oncol 18(12):1622–1633
Mohyeldin A, Garzón-Muvdi T, Quiñones-Hinojosa A (2010) Oxygen in stem cell biology: a critical component of the stem cell niche. Cell Stem Cell 7(2):150–161
Rape A, Ananthanarayanan B, Kumar S (2014) Engineering strategies to mimic the glioblastoma microenvironment. Adv Drug Del Rev 79:172–183
Lefranc F, Le Rhun E, Kiss R, Weller M (2018) Glioblastoma quo vadis: will migration and invasiveness reemerge as therapeutic agents? Cancer Treat Rev 68:145–154
Paw I, Carpenter RC, Watabe K, Debinski W, Lo HW (2015) Mechanisms regulating glioma invasion. Cancer Lett 362:1–7
Nobes CD, Hall A (1999) Rho GTPases control polarity, protrusion, and adhesion during cell movement. J Cell Biol 144(6):1235–1244
McDonough W, Tran N, Giese A, Norman SA, Berens ME (1998) Altered gene expression in human astrocytoma cells selected for migration: I. Thromboxane synthase. J Neuropathol Exp Neurol 57(5):449–455
Albini A, Iwamoto Y, Kleinman H, Martin GR, Sa A, Kozlowski JM, McEwan RN (1987) A rapid in vitro assay for quantitating the invasive potential of tumor cells. Cancer Res 47(12):3239–3245
Ohnishi T, Matsumura H, Izumoto S, Hiraga S, Hayakawa T (1998) A novel model of glioma cell invasion using organotypic brain slice culture. Cancer Res 58(14):2935–2940
Abbadi S, Rodarte JJ, Abutaleb A, Lavell E, Smith CL, Ruff W, Schiller J, Olivi A, Levchenko A, Guerrero-Cazares H, Quinones-Hinojosa A (2014) Glucose-6–phosphatase is a key metabolic regulator of glioblastoma invasion. Mol Cancer Res 12(11):1547–1559
Schiapparelli P, Pirman NL, Mohler K, Miranda-Herrera PA, Zarco N, Kilic O, Miller C, Shah SR, Rogulina S, Hungerford W, Abriola L, Hoyer D, Turk BE, Guerrero-Cazares H, Isaacs FJ, Quinones-Hinojosa A, Levchenko A, Rinehart J (2021) Phosphorylated WNK kinase networks in recoded bacteria recapitulate physiological function. Cell Rep 36(3):109416
Smith CL, Kilic O, Schiapparelli P, Guerrero-Cazares H, Kim DH, Sedora-Roman NI, Gupta S, O’Donnel T, Chaichana KL, Rodriguez FJ, Abbadi S, Park J, Quinones-Hinojosa A, Levchenko A (2016) Migration phenotype of brain-cancer cells predicts patient outcomes. Cell Rep 15(12):2616–2624
Neufeld L, Yeini E, Reisman N, Shtilerman Y, Ben-Shushan D, Pozzi S, Madi A, Tiram G, Eldar-Boock A, Ferber S, Grossman R, Ram Z, Satchi-Fainaro R (2021) Microengineered perfusable 3D-bioprinted glioblastoma model for in vivo mimicry of tumor microenvironment. Sci Adv 7(34):1–19
Kilic O, Pamies D, Lavell E, Schiapparelli P, Feng Y, Hartung T, Bal-Price A, Hogberg HT, Quinones-Hinojosa A, Guerrero-Cazares H, Levchenko A (2016) Brain-on-a-chip model enables analysis of human neuronal differentiation and chemotaxis. Lab Chip 16(21):4152–4162
Wong BS, Shah SR, Tankaskas CL, Bajpai VK, Wu PH, Chin D, Ifemembi B, ReFaey K, Schiapparelli P, Zheng X, Martin SS, Fan CM, Quinones-Hinojosa A, Konstantopoulos K (2021) A microfluidic cell-migration assay for the prediction of progression-free survival and recurrence time of patients with glioblastoma. Nat Biomed Eng 5(1):26–40
Chaichana KL, Guerrero-Cazares H, Capilla-Gonzalez V, Zamora-Berridi G, Achanya P, Gonzalez-Perez O, Jallo GI, Garcia-Verdugo JM, Quinones-Hinojosa A (2009) Intra-operatively obtained human tissue: protocols and techniques for the study of neural stem cells. J Neurosci Methods 180(1):116–125
Quiñones-Hinojosa A, Chaichana K (2007) The human subventricular zone: a source of new cells and a potential source of brain tumors. Exp Neurol 205(2):313–324
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675
Chaichana KL, Capilla-Gonzalez V, Gonzalez-Perez O, Pradilla G, Han J, Olivi A, Brem H, Garcia-Verdugo JM, Quinones-Hinojosa A (2007) Preservation of glial cytoarchitecture from ex vivo human tumor and non-tumor cerebral cortical explants: a human model to study neurological diseases. J Neurosci Methods 164(2):261–270
Guerrero-Cázares H, Chaichana KL, Quiñones-Hinojosa A (2009) Neurosphere culture and human organotypic model to evaluate brain tumor stem cells. Cancer Stem Cells. https://doi.org/10.1007/978-1-59745-280-9_6
Ravi VM, Joseph K, Wurm J, Behringer S, Garrelfs N, d’Errico P, Naseri Y, Franco P, Meyer-Luehmann M, Sankowski R, Johannes Shah M, Mader I, Delev D, Follo M, Beck J, Schnell O, Hofmann UG, Heiland DH (2019) Human organotypic brain slice culture: a novel framework for environmental research in neuro-oncology. Life Sci Alliance 2(4):1–15
Vivas-Buitrago T, Domingo RA, Tripathi S, De Biase G, Brown D, Akinduro OO, Ramos-Fresnedo A, Sabsevitz DS, Bendok BR, Sherman W, Parney IF, Jentoft ME, Middlebrooks EH, Meyer FB, Chaichana KL, Quinones-Hinojosa A (2021) Influence of supramarginal resection on survival outcomes after gross-total resection of IDH-wild-type glioblastoma. J Neurosurg 136(1):1–8
Tripathi S, Vivas-Buitrago T, Domingo RA, De Biase G, Brown D, Akinduro OO, Ramos-Fresnedo A, Sherman W, Gupta V, Middlebooks EH, Sabsevitz DS, Porter AB, Uhm JH, Bendok BR, Parney I, Meyer FB, Chaichana KL, Swanson KR, Quinones-Hinojosa A (2021) IDH-wild-type glioblastoma cell density and infiltration distribution influence on supramarginal resection and its impact on overall survival: a mathematical model. J Neurosurg. https://doi.org/10.3171/2021.6.JNS21925
Shah AH, Mahavadi A, Di L, Sanjurjo A, Eichberg DG, Borowy V, Figueroa J, Luther E, de la Fuente MI, Semonche A, iVan ME Komotar RJ (2020) Survival Benefit of Lobectomy for Glioblastoma: moving towards radical supramaximal resection. J Neurooncol 148(3):501–508
Ruiz-Garcia H, Zarco N, Watanabe F, De Araujo FV, Suarez-Meade P, Guerrero-Cazares H, Imitola J, Quinones-Hinojosa A, Trifiletti D (2023) Development of experimental three-dimensional tumor models to study glioblastoma cancer stem cells and tumor microenvironment. Methods Mol Biol. https://doi.org/10.1007/978-1-0716-2703-7_9
Garcia CA, Bhargav AG, Brooks M, Suarez-Meade P, Bhargav AG, Brooks M, Suarez-Meade P, Mondal SK, Zarco N, ReFaey K, Jentoft M, Middlebrooks EH, Snuderl M, Carrano A, Guerrero-Cazares H, Schiapparelli P, Sarabia-Estrada R, Quinones-Hinojosa A (2021) Functional characterization of brain tumor-initiating cells and establishment of GBM preclinical models that incorporate heterogeneity, therapy, and sex differences. Mol Cancer Ther 20(12):2585–2597
Garzon-Muvdi T, Schiapparelli P, ap Rhys, C., Guerrero-Cazares, H., Smith, C., Kim, D. H., ... Quiñones-Hinojosa, A. (2012) Regulation of brain tumor dispersal by NKCC1 through a novel role in focal adhesion regulation. PLoS Biol 10(5):e1001320
Lowe DG (2004) Distinctive image features from scale-invariant keypoints. Int J Computer Vision 60(2):91–110
Kucharzewska P, Christianson HC, Welch JE, Svensson KJ, Fredlund E, Ringner M, Morgelin M, Bourseau-Guilmain BJ, Belting M (2013) Exosomes reflect the hypoxic status of glioma cells and mediate hypoxia-dependent activation of vascular cells during tumor development. Proc Natl Acad Sci 110(18):7312–7317
Suzuki SO, Goldman JE (2003) Multiple cell populations in the early postnatal subventricular zone take distinct migratory pathways: a dynamic study of glial and neuronal progenitor migration. J Neurosci 23(10):4240–4250
Tanaka M, Tomita A, Yoshida S, Yano M, Shimizu H (1994) Observation of the highly organized development of granule cells in rat cerebellar organotypic cultures. Brain Res 641(2):319–327
Holopainen IE (2005) Organotypic hippocampal slice cultures: a model system to study basic cellular and molecular mechanisms of neuronal cell death, neuroprotection, and synaptic plasticity. Neurochem Res 30(12):1521–1528
Holtkamp N, Afanasieva A, Elstner A, van Landeghem FKH, Konnejer M, Kuhn SA, Kettenmann H, von Deimling A (2005) Brain slice invasion model reveals genes differentially regulated in glioma invasion. Biochem Biophys Res Commun 336(4):1227–1233
Valster A, Tran NL, Nakada M, Berens ME, Chan AY, Symons M (2005) Cell migration and invasion assays. Methods 37(2):208–215
Cavaliere F, Dinkel K, Reymann K (2006) The subventricular zone releases factors which can be protective in oxygen/glucose deprivation-induced cortical damage: an organotypic study. Exp Neurol 201(1):66–74
Scherer H (1940) The forms of growth in gliomas and their practical significance. Brain 63(1):1–35
Goldbrunner R, Bernstein J, Tonn J (1999) Cell-extracellular matrix interaction in glioma invasion. Acta Neurochir 141(3):295
Lugassy C, Haroun RI, Brem H, Tyler BM, Jones RV, Fernandez PM, Patierno SR, Kleinman HK, Barnhill RL (2002) Pericytic-like angiotropism of glioma and melanoma cells. Am J Dermatopathol 24(6):473–478
von Bülow C, Hayen W, Hartmann A, Mueller-Klieser W, Allolio B, Nehls V (2001) Endothelial capillaries chemotactically attract tumor cells. J pathol 193(3):367–376
Farin A, Suzuki SO, Weiker M, Goldman JE, Bruce JN, Canoll P (2006) Transplanted glioma cells migrate and proliferate on host brain vasculature: a dynamic analysis. Glia 53(8):799–808
Winkler F, Kienast Y, Fuhrmann M, Von Baumgarten L, Burgold S, Mitteregger G, Kretzschmar H, Herms J (2009) Imaging glioma cell invasion in vivo reveals mechanisms of dissemination and peritumoral angiogenesis. Glia 57(12):1306–1315
Funding
AQH was supported by the following: (i) Mayo Clinic Clinician Investigator award; (ii) State of Florida Department of Health Endowed Cancer Chair; (iii) William J. and Charles H. Mayo Professor; (iv) Monica Flynn Jacoby Endowed Chair.
Author information
Authors and Affiliations
Contributions
Conception and Design: RR, HGC, JZ, AQH. Data Collection: RR, PSM, HGC, BB, PSB, SG, KLC, LB, JZ, AQH. Analysis and Interpretation: RR, PSM, HGC, BB, PSB, ESN, TVB, LB, JZ, AQH. Manuscript Writing: RR, PSM, HGC. Manuscript Revision: RR, PSM, HGC, BB, ESN, KLC, PSB, JZ, AQH. All authors approved the final version of this manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Video 1 (MOV 23795 KB)
Supplementary Video 2 (MOV 23581 KB)
Supplementary Video 3 (MP4 5144 KB)
Supplementary Video 4 (MP4 7548 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ravin, R., Suarez-Meade, P., Busse, B. et al. Perivascular invasion of primary human glioblastoma cells in organotypic human brain slices: human cells migrating in human brain. J Neurooncol 164, 43–54 (2023). https://doi.org/10.1007/s11060-023-04349-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04349-9