Abstract
Background
The HIT-SKK protocol is used for low/standard-risk medulloblastomas in young children with the aim to eliminate cranial irradiation and its neuropsychological (NP) sequelae. This therapy includes IV and intraventricular (ITV) methotrexate (MTX) potentially responsible for leukoencephalopathy (LE) and neurocognitive disorders. This study describes the risk factors and course of LE, and investigates its correlation with neurocognitive impact.
Methods
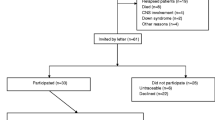
A retrospective, multicenter study was conducted in 35 children under 5 years old, with a median follow-up of 72 months (range 14 to 130). The main analysis was performed in 30 patients who received cumulative doses of MTX as per-protocol (group 1). Five patients who received higher cumulative doses of MTX were analyzed separately. All follow-up MRIs and NP assessments were centrally reviewed by experts.
Results
Twenty patients in group 1 developed LE, grade 2 and 3 abnormalities did not correlate with higher cumulative doses of ITV-MTX (p = 0.698). Considering the most recent NP evaluation, the Full-Scale IQ (FSIQ) and Wechsler indices were in the average to lower average range. The FSIQ was deficient in 6/17 evaluable patients. Cumulative dose of ITV-MTX was almost associated with decreased processing speed competence (p = 0.055) which was the most frequently impaired neurocognitive domain. Neuropsychological assessment scores were not statistically lower in patients with persistent grade 2 LE at the end of follow-up.
Conclusion
This study described that the use of cumulative dose of MTX (IV and ITV) according to the HIT-SKK protocol resulted in LE that tented to decrease over time, without significant correlation with a decline in neuro-intellectual skills.


Similar content being viewed by others
References
Lafay-Cousin L, Bouffet E, Hawkins C, Amid A, Huang A, Mabbott DJ (2009) Impact of radiation avoidance on survival and neurocognitive outcome in infant medulloblastoma. Curr Oncol Tor Ont Dec 16(6):21–28
Zeltzer PM, Boyett JM, Finlay JL, Albright AL, Rorke LB, Milstein JM et al (1999) Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the children’s Cancer Group 921 randomized phase III study. J Clin Oncol Off J Am Soc Clin Oncol Mar 17(3):832–845
Kellie SJ (1999) Chemotherapy of central nervous system tumours in infants. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg Oct 15(10):592–612
Merchant TE, Schreiber JE, Wu S, Lukose R, Xiong X, Gajjar A (2014) Critical combinations of radiation dose and volume predict intelligence quotient and academic achievement scores after craniospinal irradiation in children with medulloblastoma. Int J Radiat Oncol Biol Phys 1 Nov 90(3):554–561
Mulhern RK, Kepner JL, Thomas PR, Armstrong FD, Friedman HS, Kun LE (1998) Neuropsychologic functioning of survivors of childhood medulloblastoma randomized to receive conventional or reduced-dose craniospinal irradiation: a Pediatric Oncology Group study. J Clin Oncol Off J Am Soc Clin Oncol May 16(5):1723–1728
Grill J, Sainte-Rose C, Jouvet A, Gentet JC, Lejars O, Frappaz D et al (2005) Treatment of medulloblastoma with postoperative chemotherapy alone: an SFOP prospective trial in young children. Lancet Oncol Aug 6(8):573–580
Grundy RG, Wilne SA, Weston CL, Robinson K, Lashford LS, Ironside J et al (2007) Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: the UKCCSG/SIOP prospective study. Lancet Oncol Aug 8(8):696–705
Geyer JR, Sposto R, Jennings M, Boyett JM, Axtell RA, Breiger D et al (2005) Multiagent Chemotherapy and Deferred Radiotherapy in Infants with malignant brain tumors: a Report from the children’s Cancer Group. J Clin Oncol 20 Oct 23(30):7621–7631
Dhall G, Grodman H, Ji L, Sands S, Gardner S, Dunkel IJ et al (2008) Outcome of children less than three years old at diagnosis with non-metastatic medulloblastoma treated with chemotherapy on the « Head Start » I and II protocols. Pediatr Blood Cancer Jun 50(6):1169–1175
Cohen BH, Geyer JR, Miller DC, Curran JG, Zhou T, Holmes E et al (2015) Pilot Study of Intensive Chemotherapy with Peripheral hematopoietic cell support for children less than 3 years of Age with malignant brain tumors, the CCG-99703 phase I/II study. A Report from the children’s Oncology Group. Pediatr Neurol Jul 53(1):31–46
Rutkowski S, Bode U, Deinlein F, Ottensmeier H, Warmuth-Metz M, Soerensen N et al (Mar 2005) Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. N Engl J Med 10(10):978–986
Rutkowski S, von Hoff K, Emser A, Zwiener I, Pietsch T, Figarella-Branger D et al (2010) Survival and prognostic factors of early childhood medulloblastoma: an international meta-analysis. J Clin Oncol Off J Am Soc Clin Oncol 20 Nov 28(33):4961–4968
Mynarek M, von Hoff K, Pietsch T, Ottensmeier H, Warmuth-Metz M, Bison B et al (2020) Nonmetastatic medulloblastoma of early childhood: results from the prospective clinical trial HIT-2000 and an extended validation cohort. J Clin Oncol Off J Am Soc Clin Oncol 20 Jun 38(18):2028–2040
Ottensmeier H, Schlegel PG, Eyrich M, Wolff JE, Juhnke BO, von Hoff K et al (2020) Treatment of children under 4 years of age with medulloblastoma and ependymoma in the HIT2000/HIT-REZ 2005 trials: neuropsychological outcome 5 years after treatment. PLoS ONE 15(1):e0227693
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol Aug 149(2):351–356
Limond JA, Bull KS, Calaminus G, Kennedy CR, Spoudeas HA, Chevignard MP (2015) Quality of survival assessment in european childhood brain tumour trials, for children aged 5 years and over. Eur J Paediatr Neurol Mar 19(2):202–210
Limond J, Thomas S, Bull KS, Calaminus G, Lemiere J, Traunwieser T et al (2020) Quality of survival assessment in european childhood brain tumour trials, for children below the age of 5 years. Eur J Paediatr Neurol Mar 25:59–67
Wechsler D (1991) Wechsler preschool and primary scales of intelligence, 3rd edn. The Psychological Corporation, San Antonio, TX
Wechsler D (2012) Wechsler preschool and primary scale of intelligence—fourth edition. Psychol Corp San Antonio TX
Wechsler D (2003) Wechsler Intelligence Scale for Children–Fourth Edition. Psychological Corporation, San Antonio, TX
Beery KE, Buktenica NA, Beery NA (2004) The Beery-Buktenica Developmental Test of Visual-Motor Integration: for children and adults (Beery VMI). Modern Curriculum Press
Korkman M, Kemp S, Kirk U (1998) NEPSY: A Developmental Neuropsychological Assessment; Manual [Internet]. PsychCorp; Available at: https://books.google.fr/books?id=Vv9AcgAACAAJ
Evans AS, Preston AS (2011) Test of Everyday Attention for Children. In: Kreutzer JS, DeLuca J, Caplan B, éditeurs. Encyclopedia of Clinical Neuropsychology [Internet]. New York, NY: Springer New York; p. 2493–2493. Available at: https://doi.org/10.1007/978-0-387-79948-3_1299
Cohen MJ (1997) CMS - Children Memory Scale [Internet]. Pearson Executive Office; Available at: https://books.google.fr/books?id=xhcnzQEACAAJ
Gioia GA, Isquith PK (2011) Behavior Rating Inventory for Executive Functions. In: Kreutzer JS, DeLuca J, Caplan B, éditeurs. Encyclopedia of Clinical Neuropsychology [Internet]. New York, NY: Springer New York; p. 372–6. Available at: https://doi.org/10.1007/978-0-387-79948-3_1881
Varni JW, Seid M, Rode CA (1999) The PedsQL: measurement model for the pediatric quality of life inventory. Med Care Feb 37(2):126–139
Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P (2002) The PedsQL in pediatric cancer: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales, multidimensional fatigue scale, and Cancer Module. Cancer 1 Apr 94(7):2090–2106
Reddick WE, Glass JO, Helton KJ, Langston JW, Xiong X, Wu S et al (2005) Prevalence of leukoencephalopathy in children treated for acute lymphoblastic leukemia with high-dose methotrexate. AJNR Am J Neuroradiol May 26(5):1263–1269
Dhall G, O’Neil SH, Ji L, Haley K, Whitaker AM, Nelson MD et al (2020) Excellent outcome of young children with nodular desmoplastic medulloblastoma treated on “Head Start” III: a multi-institutional, prospective clinical trial. Neuro-Oncol 18 Apr 22(12):1862–1872
Bhojwani D, Sabin ND, Pei D, Yang JJ, Khan RB, Panetta JC et al (2014) Methotrexate-induced neurotoxicity and leukoencephalopathy in childhood acute lymphoblastic leukemia. J Clin Oncol Off J Am Soc Clin Oncol 20 Mar 32(9):949–959
Cheung YT, Sabin ND, Reddick WE, Bhojwani D, Liu W, Brinkman TM et al (2016) Leukoencephalopathy and long-term neurobehavioural, neurocognitive, and brain imaging outcomes in survivors of childhood acute lymphoblastic leukaemia treated with chemotherapy: a longitudinal analysis. Lancet Haematol Oct 3(10):e456–e466
Fay-McClymont TB, Ploetz DM, Mabbott D, Walsh K, Smith A, Chi SN et al (2017) Long-term neuropsychological follow-up of young children with medulloblastoma treated with sequential high-dose chemotherapy and irradiation sparing approach. J Neurooncol May 133(1):119–128
Oyefiade A, Paltin I, De Luca CR, Hardy KK, Grosshans DR, Chintagumpala M, Mabbott DJ, Kahalley LS (2021) Cognitive Risk in Survivors of Pediatric Brain Tumors. J Clin Oncol. Jun 1;39(16):1718–1726. doi: https://doi.org/10.1200/JCO.20.02338. Epub 2021 Apr 22. PMID: 33886348; PMCID: PMC8260914
Puget S, Boddaert N, Viguier D, Kieffer V, Bulteau C, Garnett M et al (2009) Injuries to inferior vermis and dentate nuclei predict poor neurological and neuropsychological outcome in children with malignant posterior fossa tumors. Cancer 15 Mar 115(6):1338–1347
Riva D, Giorgi C, Nichelli F, Bulgheroni S, Massimino M, Cefalo G et al (2002) Intrathecal methotrexate affects cognitive function in children with medulloblastoma. Neurol 9 Jul 59(1):48–53
Doger de Spéville E, Kieffer V, Dufour C, Grill J, Noulhiane M, Hertz-Pannier L et al (2021) Neuropsychological consequences of childhood medulloblastoma and possible interventions: a review. Neurochirurgie Feb 67(1):90–98
Author information
Authors and Affiliations
Contributions
C Dufour, L Riffaud, C Puiseux, E De Carli, D Bodet, C Icher, F Doz, C Faure-Conter, A Pagnier, C Pluchart; S Thouvenin-Doulet and J Lejeune provided all patient data relevant to the writing of the manuscript. MS Merlin collected clinical, pathological and therapeutic data about included patients and wrote the main manuscript text and prepared Figures and Tables. E Schmitt performed a centralized review of all follow-up MRIs. MS Merlin and M Mezloy-Destracque performed an analysis of all neuropsychological assessment. P-L Ngyuen Thi carried out the statistical analysis. P Chastagner coordinated and supervised the entire research project.The main author declares that there is no conflict of interest. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The main author declares that there is no conflict of interest. All authors reviewed the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merlin, MS., Schmitt, E., Mezloy-Destracque, M. et al. Neurocognitive and radiological follow-up of children under 5 years of age treated for medulloblastoma according to the HIT-SKK protocol. J Neurooncol 163, 195–205 (2023). https://doi.org/10.1007/s11060-023-04328-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04328-0