Abstract
Purpose
This study aims to investigate the spatial distribution difference of brain metastases (BM) between small-cell lung cancer (SCLC) and non-small-cell lung cancer (NSCLC) and to identify the metastatic risk in brain regions.
Methods
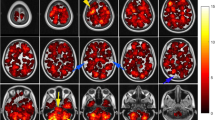
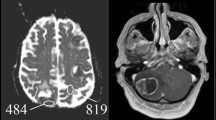
T1-enhanced MR images of 2997 BM from 728 eligible patients with SCLC and NSCLC were retrospectively reviewed by three independent medical institutions in China. All images were spatially normalised according to the Montreal Neurological Institute space, following BM delineation confirmed by three senior radiologists. The brain regions in the normalised images were identified based on the merged Anatomical Automatic Labeling atlas, and all BM locations were mapped onto these brain regions. Two-tailed proportional hypothesis testing was used to compare the BM observed rate with the expected rate based on the region’s volume, and metastatic risk regions were finally identified.
Results
In SCLC and NSCLC, BM was mainly present in the deep white matter (22.51% and 17.96%, respectively), cerebellar hemisphere (9.84% and 7.46%, respectively) and middle frontal gyrus (6.72% and 7.97%, respectively). The cerebellar hemisphere was a high-risk brain region in the SCLC. The precentral gyrus, middle frontal gyrus, paracentral lobule and cerebellar hemisphere were high-risk BM in the NSCLC. The inferior frontal gyrus and the temporal pole were a low-risk brain region in the SCLC and NSCLC, respectively.
Conclusion
The spatial BM distribution between SCLC and NSCLC is similar. Several critical brain regions had relatively low BM frequency in both SCLC and NSCLC, where a low-dose radiation distribution can be delivered due to adequate preoperative evaluations.



Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Hwang TL, Close TP, Grego JM et al (1996) Predilection of brain metastasis in gray and white matter junction and vascular border zones. Cancer 77(8):1551–1555
Lin X, DeAngelis LM (2015) Treatment of brain metastases. J Clin Oncol 33(30):3475–3484
Quattrocchi CC, Errante Y, Gaudino C et al (2012) Spatial brain distribution of intra-axial metastatic lesions in breast and lung cancer patients. J Neurooncol 110(1):79–87
Kyeong S, Cha YJ, Ahn SG et al (2017) Subtypes of breast cancer show different spatial distributions of brain metastases. PLoS ONE 12(11):e0188542
Schroeder T, Bittrich P, Kuhne JF et al (2020) Mapping distribution of brain metastases: does the primary tumor matter? J Neurooncol 147(1):229–235
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA 71(3):209–249
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14(1):48–54
Chi A, Komaki R (2010) Treatment of brain metastasis from lung cancer. Cancers 2(4):2100–2137
Ernani V, Stinchcombe TE (2019) Management of brain metastases in non–small-cell lung cancer. J Oncol Pract 15(11):563–570
Brown PD, Ahluwalia MS, Khan OH et al (2018) Whole-brain radiotherapy for brain metastases: evolution or revolution? J Clin Oncol 36(5):483–491
Brown PD, Ballman KV, Cerhan JH et al (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC· 3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1049–1060
Yanagihara TK, Mcfaline-Figueroa JR, Giacalone NJ et al (2019) A low percentage of metastases in deep brain and temporal lobe structures. Neuro Oncol 21(5):640–647
Kundapur V, Ellchuk T, Ahmed S et al (2015) Risk of hippocampal metastases in small cell lung cancer patients at presentation and after cranial irradiation: a safety profile study for hippocampal sparing during prophylactic or therapeutic cranial irradiation. Int J Radiat Oncol Biol Phys 91(4):781–786
Kwon H, Kim JW, Park M et al (2020) Brain metastases from lung adenocarcinoma may preferentially involve the distal middle cerebral artery territory and cerebellum. Front Oncol 10:1664
Mazziotta JC, Toga AW, Evans A et al (2001) A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM). Philos Trans R Soc Lond Ser B 356(1412):1293–1322
Jenkinson M, Beckmann CF, Behrens TE et al (2012) Fsl. Neuroimage 62(2):782–790
Tzourio-Mazoyer N, Landeau B, Papathanassiou D et al (2002) Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage 15(1):273–289
Yanagihara TK, Lee A, Wang TJC (2017) Quantitative analysis of the spatial distribution of metastatic brain lesions. Tomography 3(1):16–22
Péchoux CL, Sun A, Slotman BJ et al (2016) Prophylactic cranial irradiation for patients with lung cancer. Lancet Oncol 17(7):e277–e293
Gondi V, Pugh SL, Tome WA et al (2014) Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol 32(34):3810–3816
Wolfson AH, Bae K, Komaki R et al (2011) Primary analysis of a phase II randomized trial Radiation Therapy Oncology Group (RTOG) 0212: impact of different total doses and schedules of prophylactic cranial irradiation on chronic neurotoxicity and quality of life for patients with limited-disease small-cell lung cancer. Int J Radiat Oncol Biol Phys 81(1):77–84
Takano K, Kinoshita M, Takagaki M et al (2016) Different spatial distributions of brain metastases from lung cancer by histological subtype and mutation status of epidermal growth factor receptor. Neuro Oncol 18(5):716–724
Fidler IJ, Yano S, Zhang R et al (2002) The seed and soil hypothesis: vascularisation and brain metastases. Lancet Oncol 3(1):53–57
Knisely J, Yu JB (2010) Hippocampal-sparing whole-brain radiotherapy: a “how-to” technique using helical tomotherapy and linear accelerator-based intensity-modulated radiotherapy: in regard to Gondi V, et al (Int J Radiat Oncol Biol Phys 2010;78(4):1244–1252). Int J Radiat Oncol Biol Phys 2011;79(3):957–958
Han Y-M, Cai G, Chai WM et al (2017) Radiological distribution of brain metastases and its implication for the hippocampus avoidance in whole brain radiotherapy approach. Br J Radiol 90(1079):20170099
Rivera MP, Mehta AC, Wahidi MM (2013) Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143(5):e142S-e165S
Yamamoto M, Serizawa T, Shuto T et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15(4):387–395
Funding
This work was supported by the Key Research and Development Program of Shandong Province (Grant Number: 2021SFGC0104), Key Research and Development Program of Jiangsu Province (Grant Number: BE2021663), China Postdoctoral Science Foundation (Grant Number: 2022M712332), Science and Technology Project of Suzhou (Grant Number: SJC2021014), Natural Science Foundation of Shandong Province (Grant Numbers: ZR2022QF071, ZR2022QF099), National Natural Science Foundation of China (Grant Numbers: 81872475, 81372413), Shandong Key Research and Development Plan (Grant Numbers: 2017CXGC1209, 2017GSF18164), Outstanding Youth Natural Science Foundation of Shandong Province (Grant Number: JQ201423), Clinical Medicine Science and Technology Innovation Plan of Jinan (Grant Number: 201704095), and National Key Research and Development Program of China (Grant Number: 2016YFC0904700).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Study design, data acquisition: YW, BL, MN, GW, SY, XG. Patient sample collection: YW, BL, MN, JS, YB, WL. Data analysis: WS, YW, WX, XG. Drafted manuscript: WS, YW, XG. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Not applicable.
Ethical approval
This study was approved by the ethics committee of each participating hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, W., Wang, Y., Xia, W. et al. Brain metastases from small cell lung cancer and non-small cell lung cancer: comparison of spatial distribution and identification of metastatic risk regions. J Neurooncol 161, 97–105 (2023). https://doi.org/10.1007/s11060-022-04211-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04211-4