Abstract
Purpose
The incidence of intracranial metastatic disease (IMD) in patients with gastrointestinal (GI) cancers is rising. Expression of the erythroblastic oncogene B-2 (ERBB2) is associated with an in increased risk of IMD in patients with breast cancer. The implications of ERBB2 expression for IMD risk in patients with GI cancers is less clear. The objective of this systematic review was to determine the incidence of IMD and OS in patients with ERBB2+ gastrointestinal cancers.
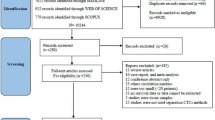
Methods
A literature search of MEDLINE, EMBASE, CENTRAL, and grey literature sources was conducted from date of database inception to July 2021. Included studies reported outcomes on patients with IMD secondary to ERBB2 GI cancers.
Results
Fourteen cohort studies met inclusion criteria, of which thirteen were retrospective. Eleven studies reported on gastric, esophageal, or gastroesophageal junction cancers. Three studies directly compared incidence of IMD based on ERBB2 status and among these, ERBB2+ patients had a higher incidence of IMD. One study indicated that ERBB2+ patients had significantly longer OS from the times of primary cancer (P = .015) and IMD diagnosis (P = .01), compared with patients with ERBB2− disease.
Conclusions
In this systematic review, patients with ERBB2+ GI cancer were more likely to develop IMD. Future study is required on the prognostic and predictive value of ERBB2 status in patients with GI cancers.
Similar content being viewed by others
Data availability
The data, analytic methods, and study materials will be made available to other researchers on request.
Abbreviations
- ERBB2:
-
Erythroblastic oncogene B-2
- GI:
-
Gastrointestinal
- IMD:
-
Intracranial metastatic disease
- OS:
-
Overall survival
References
Arnold M et al (2020) Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159(1):335-349.e15. https://doi.org/10.1053/j.gastro.2020.02.068
Schechter AL et al (1984) The neu oncogene: an erb-B-related gene encoding a 185,000-Mr tumour antigen. Nature 312(5994):513–516. https://doi.org/10.1038/312513A0
Go PH, Klaassen Z, Meadows MC, Chamberlain RS (2011) Gastrointestinal cancer and brain metastasis: a rare and ominous sign. Cancer. https://doi.org/10.1002/cncr.25940
Da Silva AN, Nagayama K, Schlesinger DJ, Sheehan JP (2009) Gamma Knife surgery for brain metastases from gastrointestinal cancer: clinical article. J Neurosurg 111(3):423–430. https://doi.org/10.3171/2008.9.JNS08281
Habbous S et al (2020) Incidence and real-world burden of brain metastases from solid tumors and hematologic malignancies in Ontario: a population-based study. Neuro-oncol Adv. https://doi.org/10.1093/NOAJNL/VDAA178
Chamberlain RS, Nyberg C, Shrestha S (2015) “Gastrointestinal cancer and brain metastasis outcomes and management”, in brain metastases from primary tumors: epidemiology. Biol Ther. https://doi.org/10.1016/B978-0-12-801419-6.00015-X
Palmieri D et al (2007) Her-2 overexpression increases the metastatic outgrowth of breast cancer cells in the brain. Cancer Res 67(9):4190–4198. https://doi.org/10.1158/0008-5472.CAN-06-3316
Pestalozzi BC et al (2006) Identifying breast cancer patients at risk for central nervous system (CNS) metastases in trials of the International breast cancer study group (IBCSG). Ann Oncol Off J Eur Soc Med Oncol 17(6):935–944. https://doi.org/10.1093/ANNONC/MDL064
Pasquier D et al (2020) Treatment and outcomes in patients with central nervous system metastases from breast cancer in the real-life ESME MBC cohort. Eur J Cancer 125:22–30. https://doi.org/10.1016/J.EJCA.2019.11.001
Howlader N et al (2014) US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. https://doi.org/10.1093/JNCI/DJU055
Seung SJ, Traore AN, Pourmirza B, Fathers KE, Coombes M, Jerzak KJ (2020) A population-based analysis of breast cancer incidence and survival by subtype in ontario women. Curr Oncol 27(2):e191–e198. https://doi.org/10.3747/CO.27.5769
Tsukada Y, Fouad A, Pickren JW, Lane WW (1983) central nervous system metastasis from breast carcinoma autopsy study. Cancer. https://doi.org/10.1002/1097-0142
Lin NU, Bellon JR, Winer EP (2004) CNS metastases in breast cancer. J Clin Oncol 22(17):3608–3617. https://doi.org/10.1200/JCO.2004.01.175
Darlix A et al (2018) Hormone receptors status: a strong determinant of the kinetics of brain metastases occurrence compared with HER2 status in breast cancer. J Neurooncol 138(2):369–382. https://doi.org/10.1007/S11060-018-2805-9/TABLES/3
Gori S et al (2007) Central nervous system metastases in HER-2 positive metastatic breast cancer patients treated with trastuzumab: incidence, survival, and risk factors. Oncologist 12(7):766–773. https://doi.org/10.1634/THEONCOLOGIST.12-7-766
Lin NU et al (2020) Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol 38(23):2610. https://doi.org/10.1200/JCO.20.00775
Brufsky AM et al (2011) Central nervous system metastases in patients with HER2-positive metastatic breast cancer: incidence, treatment, and survival in patients from registHER. Clin Cancer Res 17(14):4834–4843. https://doi.org/10.1158/1078-0432.CCR-10-2962
Bang YJ et al (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. https://doi.org/10.1016/S0140-6736(10)61121-X
Fusco N, Bosari S (2016) HER2 aberrations and heterogeneity in cancers of the digestive system: Implications for pathologists and gastroenterologists. World J Gastroenterol 22(35):7926–7937. https://doi.org/10.3748/wjg.v22.i35.7926
Mitsui Y et al (2015) Trastuzumab in combination with docetaxel/cisplatin/S-1 (DCS) for patients with HER2-positive metastatic gastric cancer: feasibility and preliminary efficacy. Cancer Chemother Pharmacol. https://doi.org/10.1007/s00280-015-2807-7
Siena S et al (2018) Targeting the human epidermal growth factor receptor 2 (HER2) oncogene in colorectal cancer. Ann Oncol 29(5):1108–1119. https://doi.org/10.1093/annonc/mdy100
Gowryshankar A, Nagaraja V, Eslick GD (2014) HER2 status in Barrett’s esophagus & esophageal cancer: a meta analysis. J Gastrointest Oncol 5(1):25–35. https://doi.org/10.3978/j.issn.2078-6891.2013.039
Lengyel CG et al (2020) Role of her-2 in gastrointestinal tumours beyond gastric cancer: a tool for precision medicine. Gastrointest Disord 3(1):1–22. https://doi.org/10.3390/gidisord3010001
Ottawa Hospital Research Institute (2021) Newcastle Ottawa Scale: Coding Manual for Case-Control Studies
University of Oxford (2020) The Centre for Evidence-Based Medicine
Efstathiou J, Finkelstein SE (2018) The proceedings of the radiation oncology summit: ACRO 2018. J Radiat Oncol. https://doi.org/10.1007/s13566-018-0348-5
Aprile G et al (2013) HER-2 Expression in brain metastases from colorectal cancer and corresponding primary tumors: a case cohort series. Int J Mol Sci 14(2):2370–2387. https://doi.org/10.3390/ijms14022370
Blay C et al (2015) Incidence of brain metastases in HER2+ gastric or gastroesophageal junction adenocarcinoma. Acta Oncol. https://doi.org/10.3109/0284186X.2015.1011757
Cavanna L et al (2018) Gastric cancer with brain metastasis and the role of human epidermal growth factor 2 status. Oncol Lett 15(4):5787–5791. https://doi.org/10.3892/ol.2018.8054
Feilchenfeldt J et al (2015) Brain metastases in gastro-oesophageal adenocarcinoma: insights into the role of the human epidermal growth factor receptor 2 (HER2). Br J Cancer 113(5):716. https://doi.org/10.1038/BJC.2015.279
Limon D et al (2018) Brain metastasis in gastroesophageal adenocarcinoma and HER2 status. J Neurooncol. https://doi.org/10.1007/s11060-018-2798-4
Ma LX et al (2018) “Relationship between human epidermal growth factor receptor 2 (HER2) status and central nervous system metastases in gastroesophageal cancer. J Clin Oncol 36(suppl 4):145–145. https://doi.org/10.1200/JCO.2018.36.4_SUPPL.145
Mitra D et al (2019) Enrichment of HER2 amplification in brain metastases from primary gastrointestinal malignancies. Oncologist. https://doi.org/10.1634/theoncologist.2018-0152
Preusser M et al (2013) Brain metastases of gastro-oesophageal cancer: evaluation of molecules with relevance for targeted therapies. Anticancer Res 33(3):1065–1071
Safran H et al (2007) Phase I/II study of trastuzumab, paclitaxel, cisplatin and radiation for locally advanced, HER2 overexpressing, esophageal adenocarcinoma. Int J Radiat Oncol Biol Phys 67(2):405–409. https://doi.org/10.1016/J.IJROBP.2006.08.076
Sperduto PW et al (2019) Estimating survival in patients with gastrointestinal cancers and brain metastases: an update of the graded prognostic assessment for gastrointestinal cancers (GI-GPA). Clin Transl Radiat Oncol. https://doi.org/10.1016/j.ctro.2019.06.007
Tan RYC et al (2018) HER2 positive rates are enriched amongst colorectal cancer brain metastases: a study amongst 1920 consecutive patients. Ann Oncol Off J Eur Soc Med Oncol 29(7):1598–1599. https://doi.org/10.1093/annonc/mdy156
Yoon HH et al (2016) Central nervous system relapse in patients with untreated HER2-positive esophageal or gastroesophageal junction adenocarcinoma. Int J Cancer. https://doi.org/10.1002/ijc.30200
Tosi F et al (2020) Long-term clinical outcome of trastuzumab and lapatinib for her2-positive metastatic colorectal cancer. Clin Colorectal Cancer. https://doi.org/10.1016/j.clcc.2020.06.009
Sperduto PW et al (2019) Survival and prognostic factors in patients with gastrointestinal cancers and brain metastases: have we made progress? Transl Res 208:63–72. https://doi.org/10.1016/j.trsl.2019.02.011
A. G. et al (2013) HER-2 expression in brain metastases from colorectal cancer and corresponding primary tumors: a case cohort series. Int J Mol Sci 14(2):2370–2387
Tosi F et al (2020) Long-term clinical outcome of trastuzumab and lapatinib for her2-positive metastatic colorectal cancer. Clin Colorectal Cancer 19(4):256-262.e2. https://doi.org/10.1016/j.clcc.2020.06.009
Zimmer AS, Van Swearingen AED, Anders CK (2020) “HER2-positive breast cancer brain metastasis: a new and exciting landscape.” Cancer Reports. Wiley Ltd, Hoboken, p e1274
Wang S et al (2017) Brain metastases from hepatocellular carcinoma: Recent advances and future avenues. Oncotarget 8(15):25814–25829. https://doi.org/10.18632/oncotarget.15730
Wu SG, Zhang WW, Sun JY, Li FY, Lin Q, He ZY (2018) Patterns of distant metastasis between histological types in esophageal cancer. Front Oncol. https://doi.org/10.3389/fonc.2018.00302
Cavanna L et al (2018) Gastric cancer with brain metastasis and the role of human epidermal growth factor 2 status. Oncol Lett. https://doi.org/10.3892/ol.2018.8054
Lemke J et al (2014) Brain Metastases in gastrointestinal cancers: Is there a role for surgery? Int J Mol Sci. https://doi.org/10.3390/ijms150916816
Sperduto PW et al (2019) Survival and prognostic factors in patients with gastrointestinal cancers and brain metastases: have we made progress? Transl Res. https://doi.org/10.1016/j.trsl.2019.02.011
Je Y, S. J, A. JA, W. DM, and G. ZL, (1999) Gastric cancer and metastasis to the brain. Ann Surg Oncol 6(8):771–776. https://doi.org/10.1007/S10434-999-0771-3
Jørgensen JT, Hersom M (2012) HER2 as a prognostic marker in gastric cancer—a systematic analysis of data from the literature. J Cancer 3(1):137–144. https://doi.org/10.7150/jca.4090
Erickson AW, Habbous S, Wright F, Lofters AK, Jerzak KJ, Das S (2021) Assessing the association of targeted therapy and intracranial metastatic disease. JAMA Oncol 7(8):1220–1224. https://doi.org/10.1001/JAMAONCOL.2021.1600
Erickson AW et al (2020) HER2-targeted therapy prolongs survival in patients with HER2-positive breast cancer and intracranial metastatic disease: a systematic review and meta-analysis. Neuro-oncology Adv. https://doi.org/10.1093/NOAJNL/VDAA136
Liu Q, Tong X, Wang J (2019) Management of brain metastases: history and the present. Chin Neurosurg J 5(1):1–8. https://doi.org/10.1186/S41016-018-0149-0/METRICS
Fox BD, Cheung VJ, Patel AJ, Suki D, Rao G (2011) Epidemiology of metastatic brain tumors. Neurosurg Clin N Am 22(1):1–6. https://doi.org/10.1016/J.NEC.2010.08.007
Siena S et al (2021) Trastuzumab deruxtecan (DS-8201) in patients with HER2-expressing metastatic colorectal cancer (DESTINY-CRC01): a multicentre, open-label, phase 2 trial. Lancet Oncol 22(6):779–789. https://doi.org/10.1016/S1470-2045(21)00086-3
Karan C et al (2022) Human epidermal growth factor receptor 2-targeting approaches for colorectal cancer: clinical implications of novel treatments and future therapeutic avenues. JCO Oncol Pract. https://doi.org/10.1200/OP.21.00904
Strickler JH et al (2021) “MOUNTAINEER-02: Phase II/III study of tucatinib, trastuzumab, ramucirumab, and paclitaxel in previously treated HER2+ gastric or gastroesophageal junction adenocarcinoma—trial in Progress.” J Clin oncol. https://doi.org/10.1200/JCO.2021.39.3_SUPPL.TPS252
Funding
This study was supported by philanthropic funds from Gratitude 10.
Author information
Authors and Affiliations
Contributions
MS, KG, AWE and SD contributed to the study conception and design. Material preparation and data collection were performed by MS and KG. Data analysis and interpretation were completed by MS, KG, AWE and SD. The first draft of the manuscript was written by MSh and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sherman, M., Gaebe, K., Li, A.Y. et al. Erythroblastic oncogene B-2 status and intracranial metastatic disease in patients with gastrointestinal cancer: a systematic review. J Neurooncol 160, 735–742 (2022). https://doi.org/10.1007/s11060-022-04195-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04195-1