Abstract
Purpose
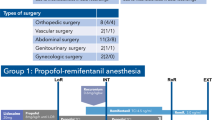
In awake surgery, the patient is sedated, but is also required to be sufficiently alert and collaborative during extensive neurocognitive testing. In the present preliminary report of a retrospective single-center study, a continuous series of 168 patients who underwent awake surgery for brain tumor located near eloquent areas, was investigated to observe the effect of dexmedetomidine (n = 58) compared with propofol (n = 110) on vigilance and collaboration required to perform extensive intra-operatory Real Time Neuropsychological Testing (RTNT).
Methods
We assigned a score to each patient, by using a scale that combines vigilance and collaboration in a 5 levels score (the higher score denoting higher level).
Results
The median interquartile range was significantly lower (range 3–5) for the dexmedetomidine group compared to the propofol one (range 4–5, p = .044). Patients with intra-operative seizures (p = .014) and/or electrocorticographic slow/epileptiform activity (p = .042), and patients in the propofol group who showed increased heart rate (p = .032) were those who obtained the lower scores (lower vigilance and collaboration level).
Conclusion
The study shows that the effect of dexmedetomidine or propofol -based conscious sedation on ability to perform Real Time Neuropsychological Testing during awake surgery for supratentorial tumor resection is different. Although both permit high mean levels of vigilance and collaboration, the patient who received dexmedetomidine was more likely to show lower vigilance and collaboration during RTNT.

Similar content being viewed by others
Data availability
The datasets analyzed for this study will be made available from the authors upon request.
Abbreviations
- Cet:
-
Concentration at effect site
- DES:
-
Direct electrical stimulation
- DEX:
-
Dexmedetomidine
- ECoG:
-
Electrocorticography
- EEG:
-
Electroencephalogram
- IOS:
-
Intra-operative seizure
- HFF:
-
High frequency filter
- LFF:
-
Low frequency filter
- MRI:
-
Magnetic resonance imaging
- P:
-
Propofol
- R:
-
Remifentanil
- RTNT:
-
Real time neuropsychological testing
- TCI:
-
Target controlled infusion
- V/C:
-
Vigilance and collaboration
References
Sanai N, Berger MS (2008) Glioma extent of resection and its impact on patient outcome. Neurosurgery 62:753–766. https://doi.org/10.1227/01.neu.0000318159.21731.cf
Duffau H, Capelle L, Denvil D et al (2003) Usefulness of intraoperative electrical subcortical mapping during surgery for low-grade gliomas located within eloquent brain regions: functional results in a consecutive series of 103 patients. J Neurosurg 98:764–778. https://doi.org/10.3171/jns.2003.98.4.0764
Duffau H, Lopes M, Arthuis F et al (2005) Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: a comparative study between two series without (1985–96) and with (1996–2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry 76:845–851. https://doi.org/10.1136/jnnp.2004.048520
Ojemann G, Ojemann J, Lettich E et al (1989) Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. J Neurosurg 71:316–326. https://doi.org/10.3171/JNS/2008/108/2/0411
Ojemann GA (1993) Functional mapping of cortical language areas in adults. Intraoperative Approaches Adv Neurol 63:155–163
Ius T, Isola M, Budai R et al (2012) Low-grade glioma surgery in eloquent areas: volumetric analysis of extent of resection and its impact on overall survival. A single-institution experience in 190 patients: clinical article. J Neurosurg 117:1039–1052. https://doi.org/10.3171/2012.8.JNS12393
Keles GE, Lundin DA, Lamborn KR et al (2004) Intraoperative subcortical stimulation mapping for hemispherical perirolandic gliomas located within or adjacent to the descending motor pathways: evaluation of morbidity and assessment of functional outcome in 294 patients. J Neurosurg 100:369–375. https://doi.org/10.3171/jns.2004.100.3.0369
Sanai N, Berger MS (2011) Extent of resection influences outcomes for patients with gliomas. Rev Neurol (Paris) 167:648–654. https://doi.org/10.1016/j.neurol.2011.07.004
Sanai N, Polley MY, Berger MS (2010) Insular glioma resection: assessment of patient morbidity, survival, and tumor progression. J Neurosurg 112:1–9. https://doi.org/10.3171/2009.6.JNS0952
Berger MS, Ojemann GA (1992) Intraoperative brain mapping techniques in neuro-oncology. Stereotact Funct Neurosurg 58:153–161. https://doi.org/10.1159/000098989
Berger MS (1994) Lesions in functional (“eloquent”) cortex and subcortical white matter. Clin Neurosurg 41:44–463
Berger MS (1996) Minimalism through intraoperative functional mapping. Clin Neurosurg 43:324–337
Duffau H, Capelle L, Sichez JP et al (2000) Surgery of the central nervous system: value of preoperative functional brain mapping by direct electric stimulation. Presse Med 29:421–422
Skrap M, Marin D, Ius T et al (2016) Brain mapping: a novel intraoperative neuropsychological approach. J Neurosurg 5:1–11. https://doi.org/10.3171/2015.10.JNS15740
Tomasino B, Rumiati RI (2020) Methods in neuropsychology. Reference module in neuroscience and biobehavioral psychology. Elsevier, Amsterdam
Meng L, McDonagh DL, Berger MS et al (2017) Anesthesia for awake craniotomy: a how-to guide for the occasional practitioner. Anesthésie pour craniotomie éveillé: guide pratique pour le praticien occasionnel. Can J Anaesth 64:517–529. https://doi.org/10.1007/s12630-017-0840-1
Kallapur BG, Bhosale R (2012) Use of dexmedetomidine infusion in anaesthesia for awake craniotomy. Indian J Anaesth 56:413–415. https://doi.org/10.4103/0019-5049.100854
Suero Molina E, Schipmann S, Mueller I et al (2018) Conscious sedation with dexmedetomidine compared with asleep-awake-asleep craniotomies in glioma surgery: an analysis of 180 patients. J Neurosurg 129:1223–1230. https://doi.org/10.3171/2017.7.JNS171312
Özlü O (2018) Anaesthesiologist’s approach to awake craniotomy. Turk J Anaesthesiol Reanim 46:250–256. https://doi.org/10.5152/TJAR.2018.56255
Sokhal N, Rath GP, Chaturvedi A et al (2015) Anaesthesia for awake craniotomy: a retrospective study of 54 cases. Indian J Anaesth 59:300–305. https://doi.org/10.4103/0019-5049.156878
Piccioni F, Fanzio M (2008) Management of anesthesia in awake craniotomy. Minerva Anestesiol 74:393–408
Garavaglia MM, Das S, Cusimano MD et al (2014) Anesthetic approach to high-risk patients and prolonged awake craniotomy using dexmedetomidine and scalp block. J Neurosurg Anesthesiol 26:226–233. https://doi.org/10.1097/ANA.0b013e3182a58aba
Kim SH, Choi SH (2020) Anesthetic considerations for awake craniotomy. Anesth Pain Med (Seoul) 31(15):269–274. https://doi.org/10.17085/apm.20050
Shen S, Zheng J, Zhang J et al (2013) Comparison of dexmedetomidine and propofol for conscious sedation in awake craniotomy: a prospective, double-blind, randomized, and controlled clinical trial. Ann Pharmacother 47:1391–1399. https://doi.org/10.1177/1060028013504082
Chung YH, Park S, Kim WH et al (2012) Anesthetic management of awake craniotomy with laryngeal mask airway and dexmedetomidine in risky patients. Korean J Anesthesiol 63:573–575. https://doi.org/10.4097/kjae.2012.63.6.573
Ard JL Jr, Bekker AY, Doyle WK (2005) Dexmedetomidine in awake craniotomy: a technical note. Surg Neurol 63:114–116. https://doi.org/10.1016/j.surneu.2004.02.029
Goettel N, Bharadwaj S, Venkatraghavan L et al (2016) Dexmedetomidine vs propofol-remifentanil conscious sedation for awake craniotomy: a prospective randomized controlled trial. Br J Anaesth 116:811–821. https://doi.org/10.1093/bja/aew024
Frost EA, Booij LH (2007) Anesthesia in the patient for awake craniotomy. Curr Opin Anaesthesiol 20:331–335. https://doi.org/10.1097/ACO.0b013e328136c56f
Herrick IA, Craen RA, Gelb AW et al (1997) Propofol sedation during awake craniotomy for seizures: electrocorticographic and epileptogenic effects. Anesth Analg 84:1280–1284. https://doi.org/10.1097/00000539-199706000-00020
Bekker AY, Kaufman B, Samir H et al (2001) The use of dexmedetomidine infusion for awake craniotomy. Anesth Analg 92:1251–1253. https://doi.org/10.1097/00000539-200105000-00031
Tomasino B, Guarracino I, Ius T et al (2021) Real-time neuropsychological testing protocol for left temporal brain tumor surgery: a technical note and case report. Front Hum Neurosci. https://doi.org/10.3389/fnhum.2021.760569
Guarracino I, Ius T, Pauletto G et al (2020) Junior-Real Time neuropsychological testing (j-RTNT) for a young patient undergoing awake craniotomy. Brain Cogn 140:105535. https://doi.org/10.1016/j.bandc.2020.105535
Tomasino B, Guarracino I, Ius T et al (2022) Real-time neuropsychological testing of sensorimotor cognition during awake surgery in precentral and postsomatosensory areas. World Neurosurg. https://doi.org/10.1016/j.wneu.2022.05.018
Tomasino B, Ius T, Skrap M (2021) Brain mapping: real-time neuropsychological testing experience during low-grade tumor resection. In: Debinski W (ed) Gliomas. Exon Publications, Brisbane
Itoi C, Hiromitsu K, Saito S et al (2015) Predicting sleepiness during an awake craniotomy. Clin Neurol Neurosurg 139:307–310. https://doi.org/10.1016/j.clineuro.2015.10.033
Jo Chris (2008) Anesthesia. In: Bagheri SC, Jo C (eds) Clinical review of oral and maxillofacial surgery. Mosby, Clay City, pp 45–63
Ius T, Mazzucchi E, Tomasino B et al (2021) Multimodal integrated approaches in low grade glioma surgery. Sci Rep 11:9964. https://doi.org/10.1038/s41598-021-87924-2
Skrap M, Tomasino MM, B, et al (2012) Surgery of insular nonenhancing gliomas: volumetric analysis of tumoral resection clinical outcome, and survival in a consecutive series of 66 cases. Neurosurgery 70:1081–1094. https://doi.org/10.1227/NEU.0b013e31823f5be5
Blume WT, Jones DC, Pathak P (2004) Properties of after-discharges from cortical electrical stimulation in focal epilepsies. Clin Neurophysiol 115:982–989. https://doi.org/10.1016/j.clinph.2003.11.023
Chatrian GE, Bergamini L, Dondey M et al (1974) A glossary of terms most commonly used by clinical electroencephalographers. Electroencephalogr Clin Neurophysiol 37:538–548. https://doi.org/10.1016/0013-4694(74)90099-6
Fisher R, Scharfman HE, DeCurtis M (2014) How can we identify ictal and interictal abnormal activity? Adv Exp Med Biol 813:3–23. https://doi.org/10.1007/978-94-017-8914-1_1
Chong DJ, Hirsch LJ (2005) Which EEG patterns warrant treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J Clin Neurophysiol 22:79–91. https://doi.org/10.1097/01.wnp.0000158699.78529.af
Lettieri T, Ius L, Verriello L et al (2021) Risk factors for intraoperative seizures in glioma surgery: electrocorticography matters. J Clin Neurophysiol. https://doi.org/10.1097/WNP.0000000000000854
Hansen E, Seemann M, Zech N et al (2013) Awake craniotomies without any sedation: the awake-awake-awake technique. Acta Neurochir (Wien) 155:1417–1424. https://doi.org/10.1007/s00701-013-1801-2
Manninen PH, Balki M, Lukitto K et al (2006) Patient satisfaction with awake craniotomy for tumor surgery: a comparison of remifentanil and fentanyl in conjunction with propofol. Anesth Analg 102:237–242. https://doi.org/10.1213/01.ANE.0000181287.86811.5C
Tasbihgou SR, Barends CRM, Absalom AR (2021) (2021) The role of dexmedetomidine in neurosurgery. Best Pract Res Clin Anaesthesiol 35(2):221–229. https://doi.org/10.1016/j.bpa.2020.10.002
Akeju O, Kim SE, Vazquez R et al (2016) Spatiotemporal dynamics of dexmedetomidine-induced electroencephalogram oscillations. PLoS ONE 11(10):e0163431. https://doi.org/10.1371/journal.pone.0163431
Mason KP, O’Mahony E, Zurakowski D, Libenson MH (2009) Effects of dexmedetomidine sedation on the EEG in children. Paediatr Anaesth 19(12):1175–1183. https://doi.org/10.1111/j.1460-9592.2009.03160.x
Chaitanya G, Arivazhagan A, Sinha S et al (2015) Dexmedetomidine anesthesia enhances spike generation during intra-operative electrocorticography: a promising adjunct for epilepsy surgery. Epilepsy Res 109:65–71. https://doi.org/10.1016/j.eplepsyres.2014.10.006
Elbakry AE, Ibrahim E (2017) Propofol-dexmedetomidine versus propofol-remifentanil conscious sedation for awake craniotomy during epilepsy surgery. Minerva Anestesiol 83(12):1248–1254. https://doi.org/10.23736/S0375-9393.17.11873-0
Acknowledgements
This work was supported by the Ricerca Corrente (Italian Ministry of Health) to B.T.
Funding
This study was funded by Ministry of Health, Ricerca Corrente.
Author information
Authors and Affiliations
Contributions
GP, TI, MS, CD and BT designed the study, GP, SP, IG, TI, DF, AN, SM, CL, acquired the data; MI, MDM and BT analyzed the data; BT, GP, IG, TI, CD and MS wrote the paper; all authors edited the paper; all authors revised the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tomasino, B., Guarracino, I., Pauletto, G. et al. Performing real time neuropsychological testing during awake craniotomy: are dexmedetomidine or propofol the same? A preliminary report. J Neurooncol 160, 707–716 (2022). https://doi.org/10.1007/s11060-022-04191-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04191-5