Abstract
Background
Intraoperative magnetic resonance imaging (iMRI) is a useful adjunct for resection of primary malignant brain tumors (MBTs). The aim of our study is to investigate the impact of iMRI on health care utilization in patients who underwent craniotomy for resection of MBTs.
Materials and methods
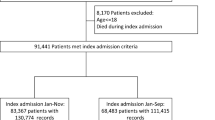
MarketScan database were queried using the ICD-9/10 and CPT 4th edition, from 2008 to 2020. We included patients ≥ 18 years of age who underwent a craniotomy with at-least one year follow-up. Outcomes were length of stay (LOS), discharge disposition, hospital/emergency room (ER) re-admissions, outpatient services, medication refills and corresponding payments.
Results
Of 6,640 patients who underwent craniotomy for MBTs, 465 patients (7%) had iMRI used during the procedure with 0.7% per year increase in iMRI use during the study period. Patients without iMRI use had higher complications at index hospitalization compared to those with iMRI use (19% vs. 14%, p = 0.04). There was no difference in the ER admission rates among the patients who underwent surgery with and without iMRI use at 6-months and 1-year after the index procedure. In terms of post-discharge payments, no significant differences were noted among the patients without and with iMRI use at 6-months ($81,107 vs. $ 81,458, p = 0.26) and 1-year ($132,657 vs. $ 118,113, p = 0.12).
Conclusion
iMRI use during craniotomy for MBT gradually increased during the study period. iMRI did not result in higher payments at index hospitalization, 6-months, and 1-year after the index procedure.


Similar content being viewed by others
References
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12:997–1003. https://doi.org/10.1016/s1470-2045(11)70196-6
Nimsky C, Ganslandt O, Cerny S, Hastreiter P, Greiner G, Fahlbusch R (2000) Quantification of, visualization of, and compensation for brain shift using intraoperative magnetic resonance imaging. Neurosurgery 47:1070–1079; discussion 1079–1080 https://doi.org/10.1097/00006123-200011000-00008
Shahar T, Rozovski U, Marko NF, Tummala S, Ziu M, Weinberg JS, Rao G, Kumar VA, Sawaya R, Prabhu SS (2014) Preoperative imaging to predict intraoperative changes in tumor-to-corticospinal tract distance: an analysis of 45 cases using high-field intraoperative magnetic resonance imaging. Neurosurgery 75:23–30. https://doi.org/10.1227/neu.0000000000000338
Akbari SHA, Sylvester PT, Kulwin C, Shah MV, Somasundaram A, Kamath AA, Beaumont TL, Rich KM, Chicoine MR (2019) Initial Experience Using Intraoperative Magnetic Resonance Imaging During a Trans-Sulcal Tubular Retractor Approach for the Resection of Deep-Seated Brain Tumors: A Case Series. Oper Neurosurg (Hagerstown) 16:292–301. https://doi.org/10.1093/ons/opy108
Patel PD, Ashraf O, Danish SF (2022) Magnetic Resonance-Guided Laser Interstitial Thermal Therapy for Brainstem Pathologies. World Neurosurg 161:e80–e89. https://doi.org/10.1016/j.wneu.2022.01.040
Borghei-Razavi H, Koech H, Sharma M, Krivosheya D, Lee BS, Barnett GH, Mohammadi AM (2018) Laser Interstitial Thermal Therapy for Posterior Fossa Lesions: An Initial Experience. World Neurosurg 117:e146–e153. https://doi.org/10.1016/j.wneu.2018.05.217
Hall WA, Liu H, Martin AJ, Truwit CL (2001) Minimally invasive procedures. Interventional MR image-guided neurobiopsy. Neuroimaging Clin N Am 11:705–713
Black PM, Moriarty T, Alexander E 3, Stieg P, Woodard EJ, Gleason PL, Martin CH, Kikinis R, Schwartz RB, Jolesz FA (1997) Development and implementation of intraoperative magnetic resonance imaging and its neurosurgical applications. Neurosurgery 41:831–842 discussion 842 – 835. https://doi.org/10.1097/00006123-199710000-00013
Hall WA, Truwit CL (2008) Intraoperative MR-guided neurosurgery. J Magn Reson Imaging 27:368–375. https://doi.org/10.1002/jmri.21273
Black PM, Alexander E 3, Martin C, Moriarty T, Nabavi A, Wong TZ, Schwartz RB, Jolesz F (1999) Craniotomy for tumor treatment in an intraoperative magnetic resonance imaging unit. Neurosurgery 45:423–431 discussion 431 – 423. https://doi.org/10.1097/00006123-199909000-00001
Chu RM, Tummala RP, Kucharczyk J, Truwit CL, Maxwell RE (2001) Minimally invasive procedures. Interventional MR image-guided functional neurosurgery. Neuroimaging Clin N Am 11:715–725
Fountain DM, Bryant A, Barone DG, Waqar M, Hart MG, Bulbeck H, Kernohan A, Watts C, Jenkinson MD (2021) Intraoperative imaging technology to maximise extent of resection for glioma: a network meta-analysis. Cochrane Database Syst Rev 1:Cd013630. https://doi.org/10.1002/14651858.CD013630.pub2
Lo YT, Lee H, Shui C, Lamba N, Korde R, Devi S, Chawla S, Nam Y, Patel R, Doucette J, Bunevicius A, Mekary RA (2021) Intraoperative Magnetic Resonance Imaging for Low-Grade and High-Grade Gliomas: What Is the Evidence? A Meta-Analysis. World Neurosurg 149:232–243e233. https://doi.org/10.1016/j.wneu.2021.01.089
Shah AS, Sylvester PT, Yahanda AT, Vellimana AK, Dunn GP, Evans J, Rich KM, Dowling JL, Leuthardt EC, Dacey RG, Kim AH, Grubb RL, Zipfel GJ, Oswood M, Jensen RL, Sutherland GR, Cahill DP, Abram SR, Honeycutt J, Shah M, Tao Y, Chicoine MR (2021) Intraoperative MRI for newly diagnosed supratentorial glioblastoma: a multicenter-registry comparative study to conventional surgery. J Neurosurg 135:505–514. https://doi.org/10.3171/2020.6.JNS19287
Deora H, Ferini G, Garg K, Narayanan MDK, Umana GE (2022) Evaluating the Impact of Intraoperative MRI in Neuro-Oncology by Scientometric Analysis. Life (Basel) 12. https://doi.org/10.3390/life12020175
Nimsky C, Ganslandt O, Von Keller B, Romstöck J, Fahlbusch R (2004) Intraoperative high-field-strength MR imaging: implementation and experience in 200 patients. Radiology 233:67–78. https://doi.org/10.1148/radiol.2331031352
Feigl GC, Heckl S, Kullmann M, Filip Z, Decker K, Klein J, Ernemann U, Tatagiba M, Velnar T, Ritz R (2019) Review of first clinical experiences with a 1.5 Tesla ceiling-mounted moveable intraoperative MRI system in Europe. Bosn J Basic Med Sci 19:24–30. https://doi.org/10.17305/bjbms.2018.3777
Kubben PL, ter Meulen KJ, Schijns OE, Laak-Poort MP, van Overbeeke JJ, van Santbrink H (2011) Intraoperative MRI-guided resection of glioblastoma multiforme: a systematic review. Lancet Oncol 12:1062–1070. https://doi.org/10.1016/s1470-2045(11)70130-9
Li P, Qian R, Niu C, Fu X (2017) Impact of intraoperative MRI-guided resection on resection and survival in patient with gliomas: a meta-analysis. Curr Med Res Opin 33:621–630. https://doi.org/10.1080/03007995.2016.1275935
Yahanda AT, Patel B, Shah AS, Cahill DP, Sutherland G, Honeycutt J, Jensen RL, Rich KM, Dowling JL, Limbrick DD, Dacey RG, Kim AH, Leuthardt EC, Dunn GP, Zipfel GJ, Leonard JR, Smyth MD, Shah MV, Abram SR, Evans J, Chicoine MR (2020) Impact of Intraoperative Magnetic Resonance Imaging and Other Factors on Surgical Outcomes for Newly Diagnosed Grade II Astrocytomas and Oligodendrogliomas: A Multicenter Study. Neurosurgery 88:63–73. https://doi.org/10.1093/neuros/nyaa320
Scherer M, Ahmeti H, Roder C, Gessler F, Jungk C, Pala A, Mayer B, Senft C, Tatagiba M, Synowitz M, Wirtz CR, Unterberg AW, Coburger J (2020) Surgery for Diffuse WHO Grade II Gliomas: Volumetric Analysis of a Multicenter Retrospective Cohort From the German Study Group for Intraoperative Magnetic Resonance Imaging. Neurosurgery 86:E64–e74. https://doi.org/10.1093/neuros/nyz397
Sylvester PT, Evans JA, Zipfel GJ, Chole RA, Uppaluri R, Haughey BH, Getz AE, Silverstein J, Rich KM, Kim AH, Dacey RG, Chicoine MR (2015) Combined high-field intraoperative magnetic resonance imaging and endoscopy increase extent of resection and progression-free survival for pituitary adenomas. Pituitary 18:72–85. https://doi.org/10.1007/s11102-014-0560-2
Juthani RG, Reiner AS, Patel AR, Cowan A, Roguski M, Panageas KS, Geer EB, Karimi S, Cohen MA, Tabar V (2020) Radiographic and clinical outcomes using intraoperative magnetic resonance imaging for transsphenoidal resection of pituitary adenomas. J Neurosurg 134:1824–1835. https://doi.org/10.3171/2020.4.Jns20178
Hlaváč M, Knoll A, Mayer B, Braun M, Karpel-Massler G, Etzrodt-Walter G, Coburger J, Wirtz CR, Paľa A (2020) Ten years’ experience with intraoperative MRI-assisted transsphenoidal pituitary surgery. Neurosurg Focus 48:E14. https://doi.org/10.3171/2020.3.Focus2072
Zhang Z, Yang K, Xia Y, Meng X, Yu X (2019) High-Field Intraoperative Magnetic Resonance Imaging Increases Extent of Resection and Progression-Free Survival for Nonfunctioning Pituitary Adenomas. World Neurosurg 127:e925–e931. https://doi.org/10.1016/j.wneu.2019.04.001
Gong X, Yao C-J, Yuan S-W, Zhuang D-X, Qiu T-M, Lu J-F, Zhang J, Song Y-Y, Zhu W, Mao Y, Wu J-S, Zhou L-F (2015) 3.0T iMRI-guided resection of eloquent high-grade gliomas: preliminary results of a randomised controlled trial. The Lancet 386:S11. https://doi.org/10.1016/S0140-6736(15)00589-9
Eljamel MS, Mahboob SO (2016) The effectiveness and cost-effectiveness of intraoperative imaging in high-grade glioma resection; a comparative review of intraoperative ALA, fluorescein, ultrasound and MRI. Photodiagnosis Photodyn Ther 16:35–43. https://doi.org/10.1016/j.pdpdt.2016.07.012
Coburger J, Scheuerle A, Kapapa T, Engelke J, Thal DR, Wirtz CR, König R (2015) Sensitivity and specificity of linear array intraoperative ultrasound in glioblastoma surgery: a comparative study with high field intraoperative MRI and conventional sector array ultrasound. Neurosurg Rev 38:499–509 discussion 509. https://doi.org/10.1007/s10143-015-0627-1
Kowalik K, Truwit C, Hall W, Kucharczyk J (2000) Initial assessment of costs and benefits of MRI-guided brain tumor resection. Eur Radiol 10(Suppl 3):S366–367. https://doi.org/10.1007/s003300000740
Makary M, Chiocca EA, Erminy N, Antor M, Bergese SD, Abdel-Rasoul M, Fernandez S, Dzwonczyk R (2011) Clinical and economic outcomes of low-field intraoperative MRI-guided tumor resection neurosurgery. J Magn Reson Imaging 34:1022–1030. https://doi.org/10.1002/jmri.22739
Schulder M, Carmel PW (2003) Intraoperative magnetic resonance imaging: impact on brain tumor surgery. Cancer Control 10:115–124. https://doi.org/10.1177/107327480301000203
Garcia-Garcia S, García-Lorenzo B, Ramos PR, Gonzalez-Sanchez JJ, Culebras D, Restovic G, Alcover E, Pons I, Torales J, Reyes L, Sampietro-Colom L, Enseñat J (2020) Cost-Effectiveness of Low-Field Intraoperative Magnetic Resonance in Glioma Surgery. Front Oncol 10. https://doi.org/10.3389/fonc.2020.586679
Abraham P, Sarkar R, Brandel MG, Wali AR, Rennert RC, Lopez Ramos C, Padwal J, Steinberg JA, Santiago-Dieppa DR, Cheung V, Pannell JS, Murphy JD, Khalessi AA (2019) Cost-effectiveness of Intraoperative MRI for Treatment of High-Grade Gliomas. Radiology 291:689–697. https://doi.org/10.1148/radiol.2019182095
Hansen L (2018) IBM MarketScan Research Databases for life sciences researchers. IBM Watson Health
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity Measures for Use with Administrative Data. Med Care 36:8–27
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Parikh AA, Robinson J, Zaydfudim VM, Penson D, Whiteside MA (2014) The effect of health insurance status on the treatment and outcomes of patients with colorectal cancer. J Surg Oncol 110:227–232. https://doi.org/10.1002/jso.23627
Albayrak B, Samdani AF, Black PM (2004) Intra-operative magnetic resonance imaging in neurosurgery. Acta Neurochir (Wien) 146:543–556 discussion 557. https://doi.org/10.1007/s00701-004-0229-0
Dietz N, Sharma M, Alhourani A, Ugiliweneza B, Wang D, Nuno M, Drazin D, Boakye M (2019) Outcomes of decompression and fusion for treatment of spinal infection. Neurosurg Focus 46:E7. https://doi.org/10.3171/2018.10.FOCUS18460
Sharma M, Dietz N, Alhourani A, Ugiliweneza B, Wang D, Drazin D, Boakye M (2019) Insights into complication rates, reoperation rates, and healthcare utilization associated with use of recombinant human bone morphogenetic protein-2 in patients with spine infections. Neurosurg Focus 46:E8. https://doi.org/10.3171/2018.10.FOCUS18448
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures:
The authors have no conflicts of interest or financial disclosures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharma, M., Wang, D., Palmisciano, P. et al. Is intraoperative MRI use in malignant brain tumor surgery a health care burden? A matched analysis of MarketScan Database. J Neurooncol 160, 331–339 (2022). https://doi.org/10.1007/s11060-022-04142-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04142-0