Abstract
Purpose
Identifying relationships between craniopharyngiomas (CPs) and contiguous structures, and tumor origin are crucial for treatments. This study attempted to explore the relationships and tumor origin.
Methods
CPs that underwent endoscopic surgeries were enrolled. The interfacial specimens of CPs attaching the hypothalamus, pituitary stalk (PS), pituitary grand (PG), optic chiasma (OC) and brain tissue (BT) were pathologically examined. Boundaries between CPs and these structures were observed during operations. Expression of β-catenin and stem cell markers were analyzed to explore the tumor origin. Outcomes of patients were assessed.
Results
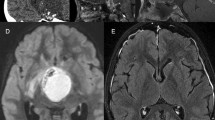
A total of 34 CPs were categorized into two groups based on the locations of finger-like protrusions (FP). Group A comprised 18 CPs with FP only present in the specimens attaching to hypothalamus. The surface of these CPs was fused with hypothalamus under endoscopic videos. However, the specimens attaching to the PS, PG, OC, and BT showed no FP. Clear boundaries was observed between these CPs and these structures. Group B comprised 16 CPs with FP only present in the specimens attaching to PS. The tumor surface was fused with PS. Specimens attaching to the hypothalamus, PG, OC and BT showed no FP. Clear boundary was observed among these CPs with these structures. These results implied CPs only invaded a certain part of hypothalamic-pituitary axis. β-catenin and stem cells markers mainly distributed in the FP tissues of both groups. Patients in group B achieved better outcomes than group A.
Conclusions
CPs only invade the hypothalamic-pituitary axis with FP and the FP would be the tumor origin.





Similar content being viewed by others
Data availability
The datasets and the corresponding videos of endoscopic surgeries generated of this study are available from the corresponding author on reasonable request.
References
Lewin R, Ruffolo E, Saraceno C (1984) Craniopharyngioma arising in the pharyngeal hypophysis. South Med J 77:1519–1523. https://doi.org/10.1097/00007611-198412000-00011
Müller HL, Merchant TE, Warmuth-Metz M, Martinez-Barbera JP, Puget S (2019) Craniopharyngioma. Nat Rev Dis Primers 5:75. https://doi.org/10.1038/s41572-019-0125-9
Fuller GN, Scheithauer BW (2007) The 2007 revised World Health Organization (WHO) classification of tumours of the central nervous system: newly codified entities. Brain Pathol 17:304–307. https://doi.org/10.1111/j.1750-3639.2007.00084.x
Puget S, Garnett M, Wray A, Grill J, Habrand JL, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A, Sainte-Rose C (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106:3–12. https://doi.org/10.3171/ped.2007.106.1.3
Martinez-Barbera JP, Andoniadou CL (2020) Biological behaviour of craniopharyngiomas. Neuroendocrinology 110:797–804. https://doi.org/10.1159/000506904
Pascual JM, Prieto R, Carrasco R, Barrios L (2013) Displacement of mammillary bodies by craniopharyngiomas involving the third ventricle: surgical-MRI correlation and use in topographical diagnosis. J Neurosurg 119:381–405. https://doi.org/10.3171/2013.1.Jns111722
Prieto R, Pascual JM, Rosdolsky M, Castro-Dufourny I, Carrasco R, Strauss S, Barrios L (2016) Craniopharyngioma adherence: a comprehensive topographical categorization and outcome-related risk stratification model based on the methodical examination of 500 tumors. Neurosurg Focus 41:E13. https://doi.org/10.3171/2016.9.Focus16304
Prieto R, Pascual JM (2014) Accurate craniopharyngioma topography for patient outcome improvement. World Neurosurg 82:e555-559. https://doi.org/10.1016/j.wneu.2014.06.026
Cavallo LM, Solari D, Esposito F, Cappabianca P (2013) The endoscopic endonasal approach for the management of craniopharyngiomas involving the third ventricle. Neurosurg Rev 36:27–37. https://doi.org/10.1007/s10143-012-0403-4
Martinez-Barbera JP, Buslei R (2015) Adamantinomatous craniopharyngioma: pathology, molecular genetics and mouse models. J Pediatr Endocrinol Metab 28:7–17. https://doi.org/10.1515/jpem-2014-0442
Kawamata T, Kubo O, Hori T (2005) Histological findings at the boundary of craniopharyngiomas. Brain Tumor Pathol 22:75–78. https://doi.org/10.1007/s10014-005-0191-4
Hölsken A, Buchfelder M, Fahlbusch R, Blümcke I, Buslei R (2010) Tumour cell migration in adamantinomatous craniopharyngiomas is promoted by activated Wnt-signalling. Acta Neuropathol 119:631–639. https://doi.org/10.1007/s00401-010-0642-9
Müller HL (2010) Childhood craniopharyngioma–current concepts in diagnosis, therapy and follow-up. Nat Rev Endocrinol 6:609–618. https://doi.org/10.1038/nrendo.2010.168
Li S, Yang L, Tong Z, Wu B, Tang B, Xie S, Li M, Zhou L, Ouyang C, Wu X, Yang Y, Wang C, Hong T (2021) The eagle sign: a new preoperative MRI-based tool for predicting topographic correlation between craniopharyngioma and hypothalamus. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-021-03791-4
Kenning TJ, Beahm DD, Farrell CJ, Schaberg MR, Rosen MR, Evans JJ (2012) Endoscopic endonasal craniopharyngioma resection. J Neurosurg 32(Suppl):E5
Yang L, Xie SH, Fang C, Zeng EM, Tang B, Hong T (2019) Preservation of hypothalamic function with endoscopic endonasal resection of hypothalamus-invaded craniopharyngiomas. World Neurosurg 132:e841–e851. https://doi.org/10.1016/j.wneu.2019.07.225
Fischer AH, Jacobson KA, Rose J, Zeller R (2008) Hematoxylin and eosin staining of tissue and cell sections. CSH Protoc. https://doi.org/10.1101/pdb.prot4986
Must A, Anderson SE (2006) Body mass index in children and adolescents: considerations for population-based applications. Int J Obes (Lond) 30:590–594. https://doi.org/10.1038/sj.ijo.0803300
Yang L, Xie S, Tang B, Wu X, Tong Z, Fang C, Ding H, Bao Y, Zheng S, Hong T (2020) Hypothalamic injury patterns after resection of craniopharyngiomas and correlation to tumor origin: a study based on endoscopic observation. Cancer Med 9:8950–8961. https://doi.org/10.1002/cam4.3589
Chen KL, Xu Y, Chu AQ, Ding D, Liang XN, Nasreddine ZS, Dong Q, Hong Z, Zhao QH, Guo QH (2016) Validation of the Chinese version of montreal cognitive assessment basic for screening mild cognitive impairment. J Am Geriatr Soc 64:e285–e290. https://doi.org/10.1111/jgs.14530
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Royle J, Lincoln NB (2008) The everyday memory questionnaire-revised: development of a 13-item scale. Disabil Rehabil 30:114–121. https://doi.org/10.1080/09638280701223876
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62. https://doi.org/10.1136/jnnp.23.1.56
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50–55. https://doi.org/10.1111/j.2044-8341.1959.tb00467.x
Gil Z, Abergel A, Spektor S, Shabtai E, Khafif A, Fliss DM (2004) Development of a cancer-specific anterior skull base quality-of-life questionnaire. J Neurosurg 100:813–819. https://doi.org/10.3171/jns.2004.100.5.0813
Qi S, Liu Y, Wang C, Fan J, Pan J, Zhang X, Lu Y (2020) Membrane structures between craniopharyngioma and the third ventricle floor based on the QST classification and its significance: a pathological study. J Neuropathol Exp Neurol 79:966–974. https://doi.org/10.1093/jnen/nlaa087
Apps JR, Stache C, Gonzalez-Meljem JM, Gutteridge A, Chalker J, Jacques TS, Forshew T, Holsken A, Martinez-Barbera JP (2020) CTNNB1 mutations are clonal in adamantinomatous craniopharyngioma. Neuropathol Appl Neurobiol 46:510–514. https://doi.org/10.1111/nan.12613
Sekine S, Shibata T, Kokubu A, Morishita Y, Noguchi M, Nakanishi Y, Sakamoto M, Hirohashi S (2002) Craniopharyngiomas of adamantinomatous type harbor beta-catenin gene mutations. Am J Pathol 161:1997–2001. https://doi.org/10.1016/s0002-9440(10)64477-x
Whelan R, Prince E, Gilani A, Hankinson T (2020) The inflammatory milieu of adamantinomatous craniopharyngioma and its implications for treatment. J Clin Med. https://doi.org/10.3390/jcm9020519
Haston S, Pozzi S, Carreno G, Manshaei S, Panousopoulos L, Gonzalez-Meljem JM, Apps JR, Virasami A, Thavaraj S, Gutteridge A, Forshew T, Marais R, Brandner S, Jacques TS, Andoniadou CL, Martinez-Barbera JP (2017) MAPK pathway control of stem cell proliferation and differentiation in the embryonic pituitary provides insights into the pathogenesis of papillary craniopharyngioma. Development 144:2141–2152. https://doi.org/10.1242/dev.150490
Hölsken A, Stache C, Schlaffer SM, Flitsch J, Fahlbusch R, Buchfelder M, Buslei R (2014) Adamantinomatous craniopharyngiomas express tumor stem cell markers in cells with activated Wnt signaling: further evidence for the existence of a tumor stem cell niche? Pituitary 17:546–556. https://doi.org/10.1007/s11102-013-0543-8
Wang CH, Qi ST, Fan J, Pan J, Peng JX, Nie J, Bao Y, Liu YW, Zhang X, Liu Y (2019) Identification of tumor stem-like cells in admanatimomatous craniopharyngioma and determination of these cells’ pathological significance. J Neurosurg. https://doi.org/10.3171/2019.5.Jns19565
Samii M, Tatagiba M (1997) Surgical management of craniopharyngiomas: a review. Neurol Med Chir (Tokyo) 37:141–149. https://doi.org/10.2176/nmc.37.141
Flitsch J, Müller HL, Burkhardt T (2011) Surgical strategies in childhood craniopharyngioma. Front Endocrinol (Lausanne) 2:96. https://doi.org/10.3389/fendo.2011.00096
Pascual JM, González-Llanos F, Barrios L, Roda JM (2004) Intraventricular craniopharyngiomas: topographical classification and surgical approach selection based on an extensive overview. Acta Neurochir (Wien) 146:785–802. https://doi.org/10.1007/s00701-004-0295-3
Kassam AB, Gardner PA, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM (2008) Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg 108:715–728. https://doi.org/10.3171/JNS/2008/108/4/0715
Pan J, Qi S, Liu Y, Lu Y, Peng J, Zhang X, Xu Y, Huang GL, Fan J (2016) Growth patterns of craniopharyngiomas: clinical analysis of 226 patients. J Neurosurg Pediatr 17:418–433. https://doi.org/10.3171/2015.7.PEDS14449
Prieto R, Pascual JM, Rosdolsky M, Barrios L (2018) Preoperative assessment of craniopharyngioma adherence: magnetic resonance imaging findings correlated with the severity of tumor attachment to the hypothalamus. World Neurosurg 110:e404–e426. https://doi.org/10.1016/j.wneu.2017.11.012
Lu YT, Qi ST, Xu JM, Pan J, Shi J (2015) A membranous structure separating the adenohypophysis and neurohypophysis: an anatomical study and its clinical application for craniopharyngioma. J Neurosurg Pediatr 15:630–637. https://doi.org/10.3171/2014.10.Peds143
Gaston-Massuet C, Andoniadou CL, Signore M, Jayakody SA, Charolidi N, Kyeyune R, Vernay B, Jacques TS, Taketo MM, Le Tissier P, Dattani MT, Martinez-Barbera JP (2011) Increased Wingless (Wnt) signaling in pituitary progenitor/stem cells gives rise to pituitary tumors in mice and humans. Proc Natl Acad Sci USA 108:11482–11487. https://doi.org/10.1073/pnas.1101553108
Marcucci F, Ghezzi P, Rumio C (2017) The role of autophagy in the cross-talk between epithelial-mesenchymal transitioned tumor cells and cancer stem-like cells. Mol Cancer 16:3. https://doi.org/10.1186/s12943-016-0573-8
Plaks V, Kong N, Werb Z (2015) The cancer stem cell niche: how essential is the niche in regulating stemness of tumor cells? Cell Stem Cell 16:225–238. https://doi.org/10.1016/j.stem.2015.02.015
Bajaj J, Diaz E, Reya T (2020) Stem cells in cancer initiation and progression. J Cell Biol https://doi.org/10.1083/jcb.201911053
Acknowledgements
The authors would like to acknowledge all the staff at Department of Pathology, the Ninth Hospital of Nanchang, including Ping Zhang, Wu Wang, Tianmin Zhou, QingMei Zhong, Yang Gui, Wenli Liu and Di Yao, for their assistance of histopathologic analysis.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Nos. 82060246 and 81460381), Ganpo555 engineering excellence of Jiangxi science and Technology Department (2013) and the Key research and invention plan of Jiangxi Science and Technology Department (20192BBG70026).
Author information
Authors and Affiliations
Contributions
Conception design and supervision: TH; Data curation: SL, BW and CY; Formal analysis: JW and ZH; Analysis and interpretation of data: BT and SX; Investigation and Specimens collection: ML, YY and CP; Histopathologic examination and evaluation: YX and SL; Drafting the article: SL; The schematic diagram drawing: BW; Critical revising the article and Methodology: LY, CW and SL; Statistical analysis: XW and SZ. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no competing and financial interests.
Ethical approval
This study was approved by the ethics committee of the First Affiliated Hospital of Nanchang University (2021-8-028).
Consent to participate
Written informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, S., Wu, B., Xiao, Y. et al. Exploring the pathological relationships between adamantinomatous craniopharyngioma and contiguous structures with tumor origin. J Neurooncol 159, 485–497 (2022). https://doi.org/10.1007/s11060-022-04084-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04084-7