Abstract
Background
Lactate dehydrogenase (LDH) is a biomarker for cancer. However, the relationship between serum LDH levels and the survival of patients with brain metastasis has been fully revealed. We aimed to evaluate the serum LDH levels and assess its prognostic value in patients with BM.
Methods
The serum LDH levels were collected from 2507 patients with BM. Patients were categorized into four groups according to the quartile of serum LDH levels. The association between serum LDH levels and overall survival (OS) was evaluated using Cox regression models and Kaplan–Meier curves. Three predictive models were used to evaluate patients.
Results
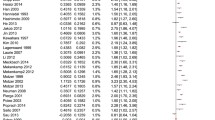
The Kaplan–Meier curve for survival by the serum LDH group demonstrates clear separation between four groups (P < 0.001). The participants in the lower group had longer OS than those in the higher group. After adjusting in multivariate Cox regression models remained significant for patients in the Q4 compared with patients in the Q1 (Q4:Q1 OR 1.58, 95% CI 1.38–1.80). Furthermore, the GPA-LDH model generates a pooled area under the curve of 0.630 (95% CI 0.600, 0.660).
Conclusions
Serum LDH levels and OS in patients with brain metastasis is an inverse association. Moreover, Serum LDH levels can improve the prognosis of the GPA model.



Similar content being viewed by others
Data availability
Yes.
References
Heron M, Anderson RN (2016) Changes in the leading cause of death: recent patterns in heart disease and cancer mortality. NCHS Data Brief pp 1–8
Boire A, Brastianos PK, Garzia L, Valiente M (2020) Brain metastasis. Nat Rev Cancer 20:4–11. https://doi.org/10.1038/s41568-019-0220-y
Sperduto PW, Mesko S, Li J, Cagney D, Aizer A, Lin NU, Nesbit E, Kruser TJ, Chan J, Braunstein S, Lee J, Kirkpatrick JP, Breen W, Brown PD, Shi D, Shih HA, Soliman H, Sahgal A, Shanley R, Sperduto WA, Lou E, Everett A, Boggs DH, Masucci L, Roberge D, Remick J, Plichta K, Buatti JM, Jain S, Gaspar LE, Wu CC, Wang TJC, Bryant J, Chuong M, An Y, Chiang V, Nakano T, Aoyama H, Mehta MP (2020) Survival in patients with brain metastases: summary report on the updated diagnosis-specific graded prognostic assessment and definition of the eligibility quotient. J Clin Oncol 38:3773–3784. https://doi.org/10.1200/jco.20.01255
Fecci PE, Champion CD, Hoj J, McKernan CM, Goodwin CR, Kirkpatrick JP, Anders CK, Pendergast AM, Sampson JH (2019) The evolving modern management of brain metastasis. Clin Cancer Res 25:6570–6580. https://doi.org/10.1158/1078-0432.Ccr-18-1624
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674. https://doi.org/10.1016/j.cell.2011.02.013
Vander Heiden MG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 324:1029–1033. https://doi.org/10.1126/science.1160809
Ward PS, Thompson CB (2012) Metabolic reprogramming: a cancer hallmark even warburg did not anticipate. Cancer Cell 21:297–308. https://doi.org/10.1016/j.ccr.2012.02.014
Thorne JL, Campbell MJ (2015) Nuclear receptors and the Warburg effect in cancer. Int J Cancer 137:1519–1527. https://doi.org/10.1002/ijc.29012
Hirschhaeuser F, Sattler UG, Mueller-Klieser W (2011) Lactate: a metabolic key player in cancer. Cancer Res 71:6921–6925. https://doi.org/10.1158/0008-5472.Can-11-1457
Xie H, Hanai J, Ren JG, Kats L, Burgess K, Bhargava P, Signoretti S, Billiard J, Duffy KJ, Grant A, Wang X, Lorkiewicz PK, Schatzman S, Bousamra M 2nd, Lane AN, Higashi RM, Fan TW, Pandolfi PP, Sukhatme VP, Seth P (2014) Targeting lactate dehydrogenase—a inhibits tumorigenesis and tumor progression in mouse models of lung cancer and impacts tumor-initiating cells. Cell Metab 19:795–809. https://doi.org/10.1016/j.cmet.2014.03.003
Yu Y, Deck JA, Hunsaker LA, Deck LM, Royer RE, Goldberg E, Vander Jagt DL (2001) Selective active site inhibitors of human lactate dehydrogenases A4, B4, and C4. Biochem Pharmacol 62:81–89. https://doi.org/10.1016/s0006-2952(01)00636-0
Drent M, Cobben NA, Henderson RF, Wouters EF, van Dieijen-Visser M (1996) Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation. Eur Respir J 9:1736–1742. https://doi.org/10.1183/09031936.96.09081736
Chen ZH, Qiu MZ, Wu XY, Wu QN, Lu JH, Zeng ZL, Wang Y, Wei XL, Wang F, Xu RH (2018) Elevated baseline serum lactate dehydrogenase indicates a poor prognosis in primary duodenum adenocarcinoma patients. J Cancer 9:512–520. https://doi.org/10.7150/jca.22305
Lee DS, Park KR, Kim SJ, Chung MJ, Lee YH, Chang JH, Kang JH, Hong SH, Kim MS, Kim YS (2016) Serum lactate dehydrogenase levels at presentation in stage IV non-small cell lung cancer: predictive value of metastases and relation to survival outcomes. Tumour Biol 37:619–625. https://doi.org/10.1007/s13277-015-3776-5
Wulaningsih W, Holmberg L, Garmo H, Malmstrom H, Lambe M, Hammar N, Walldius G, Jungner I, Ng T, Van Hemelrijck M (2015) Serum lactate dehydrogenase and survival following cancer diagnosis. Br J Cancer 113:1389–1396. https://doi.org/10.1038/bjc.2015.361
Pérez-Tomás R, Pérez-Guillén I (2020) Lactate in the tumor microenvironment: an essential molecule in cancer progression and treatment. Cancers (Basel). https://doi.org/10.3390/cancers12113244
Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514. https://doi.org/10.1016/j.ijrobp.2007.06.074
Sperduto PW, Yang TJ, Beal K, Pan H, Brown PD, Bangdiwala A, Shanley R, Yeh N, Gaspar LE, Braunstein S, Sneed P, Boyle J, Kirkpatrick JP, Mak KS, Shih HA, Engelman A, Roberge D, Arvold ND, Alexander B, Awad MM, Contessa J, Chiang V, Hardie J, Ma D, Lou E, Sperduto W, Mehta MP (2017) Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (lung-molGPA). JAMA Oncol 3:827–831. https://doi.org/10.1001/jamaoncol.2016.3834
Alba AC, Agoritsas T, Walsh M, Hanna S, Iorio A, Devereaux PJ, McGinn T, Guyatt G (2017) Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA 318:1377–1384. https://doi.org/10.1001/jama.2017.12126
Kerr KF, Brown MD, Zhu K, Janes H (2016) Assessing the clinical impact of risk prediction models with decision curves: guidance for correct interpretation and appropriate use. J Clin Oncol 34:2534–2540. https://doi.org/10.1200/jco.2015.65.5654
Pencina MJ, Dagostino RB, Dagostino RB, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172
Heagerty PJ, Zheng Y (2005) Survival model predictive accuracy and ROC curves. Biometrics 61:92–105. https://doi.org/10.1111/j.0006-341X.2005.030814.x
Denko NC (2008) Hypoxia, HIF1 and glucose metabolism in the solid tumour. Nat Rev Cancer 8:705–713. https://doi.org/10.1038/nrc2468
Palmer BF, Clegg DJ (2014) Oxygen sensing and metabolic homeostasis. Mol Cell Endocrinol 397:51–58. https://doi.org/10.1016/j.mce.2014.08.001
Armstrong AJ, George DJ, Halabi S (2012) Serum lactate dehydrogenase predicts for overall survival benefit in patients with metastatic renal cell carcinoma treated with inhibition of mammalian target of rapamycin. J Clin Oncol 30:3402–3407. https://doi.org/10.1200/jco.2011.40.9631
Motzer RJ, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J (1999) Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol 17:2530–2540. https://doi.org/10.1200/jco.1999.17.8.2530
Balch CM, Soong SJ, Atkins MB, Buzaid AC, Cascinelli N, Coit DG, Fleming ID, Gershenwald JE, Houghton A, Kirkwood JM, McMasters KM, Mihm MF, Morton DL, Reintgen DS, Ross MI, Sober A, Thompson JA, Thompson JF (2004) An evidence-based staging system for cutaneous melanoma. CA Cancer J Clin 54:131–149
Acknowledgements
None.
Funding
The work was supported by National Natural Science Foundation of China (Grant Nos. 82172842, and 81803104 and 81672386), the Sichuan Province Science and Technology Support Program (Grant Nos. 2021YFSY008, 2020YFS0276), West China Nursing Discipline Development Special Fund Project (Grant No. HXHL21008), the Technology Innovation Project of Chengdu Science and Technology Bureau (Grant No. 2019-YF05-00459-SN), Postdoctoral research and Development Fund and Translational medicine fund of West China Hospital (Grant Nos. 2020HXBH119 and CGZH19002, National Key R&D Program of China (2018YFA0108604), the 1·3·5 project for disciplines of excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (21HXFH046), the innovation team project of Affiliated Hospital of Clinical Medicine College of Chengdu University (CDFYCX202203), the project of Sichuan Science and Technology Bureau (22ZDYF0798), and Clinical Incubation Program of West China Hospital, SCU(2018HXFU008). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
FF and XCP conceived the study and designed the protocol. YYP, YH, and JYY collected data and cleaned data. YYP, YZ and ZRL analyzed and interpret data. YYP and YZ wrote the first draft of the paper. FF, XCP, YYP, YZ, ZRL, YH, JYY, RJZ, and JJW critically revised successive drafts of the paper and approved the final version. FF and XCP are the guarantors of the review.
Corresponding authors
Ethics declarations
Competing interests
The author declare that they have no competing interest.
Ethical approval
The study was approved by Ethics Committee on Biomedical Research West China Hospital of Sichuan University. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Yes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pei, YY., Zhang, Y., Liu, ZR. et al. Lactate dehydrogenase as promising marker for prognosis of brain metastasis. J Neurooncol 159, 359–368 (2022). https://doi.org/10.1007/s11060-022-04070-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04070-z