Abstract
Introduction
In this study, we investigate factors associated with radionecrosis (RN) in HER2 + (human epidermal growth factor receptor 2) patients with brain metastases (BrM) treated with stereotactic radiosurgery (SRS).
Methods
Patients with HER2 + breast cancer BrM treated with SRS (2010–2020) were identified from an institutional database. The incidence of RN was determined per treated BrM according to serial imaging and/or histology. Factors associated with RN such as age, RT dose, BrM volume, and initiation of Trastuzumab Emtansine (T-DM1) were investigated with univariate and multivariable analyses (MVA).
Results
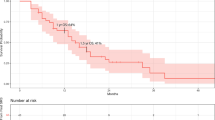
67 HER2 + patients with 223 BrM were identified. 21 patients (31.3%) were treated with T-DM1 post-SRS, including 14 patients (20.9%) who received T-DM1 within 12 months of SRS. The median follow-up was 15.6 (interquartile range (IQR) 5.4–35.3) months. The overall probability of RN post-SRS was 21.6% (95% confidence interval (CI) 2.7–10.7), and the 1 and 2 year risk was 6.7% (95% CI 2.7–10.7) and 15.2% (95% CI 9.2–21.3). MVA identified T-DM1 treatment post-SRS (hazard ratio (HR) 2.5, 95% CI 1.2–5.3, p = 0.02) and equivalent dose in 2 Gy fractions (EQD2) > 90 Gy2 (HR 2.4, 95% CI 1.1–5.1, p = 0.02) as predictors of RN. Patients treated with T-DM1 and SRS had a 29.9% (95% CI 15.3–44.6%) probability of RN, with a 25.2% (95% CI 12.8–37.6%) risk at 1- and 2 years post-T-DM1. The majority of RN were symptomatic (71%), with a median time to RN of 4.8 months.
Conclusion
T-DM1 exposure post-SRS was associated with a higher risk of RN among patients with HER2 + BrM.


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Gao YK, Kuksis M, Id Said B et al (2021) Treatment patterns and outcomes of women with symptomatic and asymptomatic breast cancer brain metastases: a single-center retrospective study. Oncologist 26(11):e1951–e1961
Barnholtz-Sloan JS, Sloan AE, Davis FG et al (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the metropolitan detroit cancer surveillance system. J Clin Oncol 22(14):2865–2872
Kuksis M, Gao YK, Tran W et al (2021) The incidence of brain metastases among patients with metastatic breast cancer: a systematic review and meta-analysis. Neuro Oncol 23(6):894–904
Sperduto PW, Mesko S, Li J et al (2020) Beyond an updated graded prognostic assessment (breast GPA): a prognostic index and trends in treatment and survival in breast cancer brain metastases from 1985 to today. Int J Radiat Oncol Biol Phys 107(2):334–343
Shewade A, Hsieh AFC, Mani A et al (2018) Real-world (RW) characteristics, treatment (tx) patterns, and overall survival (OS) in US patients (pts) with metastatic breast cancer (mBC) and CNS metastases (CNS mets). J Clin Oncol 36:1037–1037
Patchell RA, Tibbs PA, Walsh JW et al (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500
Suh JH, Kotecha R, Chao ST et al (2020) Current approaches to the management of brain metastases. Nat Rev Clin Oncol 17(5):279–299
Soliman H, Das S, Larson DA et al (2016) Stereotactic radiosurgery (SRS) in the modern management of patients with brain metastases. Oncotarget 7(11):12318
Myrehaug S, Soliman H, Ruschin M et al (2017) Clinical outcomes for frameless image-guided stereotactic radiation therapy to intact brain metastases in five daily hypofractionated treatments. Int J Radiat Oncol Biol Phys 99(2):E96–E97
Chang EL, Wefel JS, Hess K et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044
Lin NU, Borges V, Anders C et al (2020) Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. Am Soc Clin Oncol. 38:2610–2619
Bartsch R, Berghoff AS, Vogl U et al (2015) Activity of T-DM1 in Her2-positive breast cancer brain metastases. Clin Exp Metas 32(7):729–737
Lambert JM, Chari RV (2014) Ado-trastuzumab Emtansine (T-DM1): an antibody–drug conjugate (ADC) for HER2-positive breast cancer. J Med Chem 57:6949
Verma S, Miles D, Gianni L et al (2012) Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med 367(19):1783–1791
Krop IE, Lin NU, Blackwell K et al (2015) Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann Oncol 26(1):113–119
Montemurro F, Delaloge S, Barrios CH et al (2020) Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial☆. Ann Oncol 31(10):1350–1358
Shen CJ, Kummerlowe MN, Redmond KJ et al (2016) Stereotactic radiosurgery: treatment of brain metastasis without interruption of systemic therapy. Int J Radiat Oncol Biol Phys 95(2):735–742
Faruqi S, Ruschin M, Soliman H et al (2020) Adverse radiation effect after hypofractionated stereotactic radiosurgery in 5 daily fractions for surgical cavities and intact brain metastases. Int J Radiat Oncol Biol Phys. 106(4):772–779
Minniti G, Clarke E, Lanzetta G et al (2011) Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6(1):1–9
Sneed PK, Mendez J, Vemer-van den Hoek JG et al (2015) Adverse radiation effect after stereotactic radiosurgery for brain metastases: incidence, time course, and risk factors. J Neurosurgy. 123(2):373–386
Stumpf PK, Cittelly DM, Robin TP et al (2019) Combination of trastuzumab emtansine and stereotactic radiosurgery results in high rates of clinically significant radionecrosis and dysregulation of aquaporin-4. Clin Cancer Res 25(13):3946–3953
Geraud A, Xu HP, Beuzeboc P et al (2017) Preliminary experience of the concurrent use of radiosurgery and T-DM1 for brain metastases in HER2-positive metastatic breast cancer. J Neurooncol 131(1):69–72
Vilela MD, Longstreth WT Jr, Pedrosa HA et al (2018) Progressively enlarging cerebellar hematoma concurrent with T-DM1 treatment. World neurosurg 111:109–114
Mitsuya K, Watanabe J, Nakasu Y et al (2016) Expansive hematoma in delayed cerebral radiation necrosis in patients treated with T-DM1: a report of two cases. BMC Cancer 16(1):1–5
Santacroce A, Kamp MA, Budach W et al (2013) Radiobiology of radiosurgery for the central nervous system. BioMed Res Int. 2013:1–9
Mehrabian H, Desmond KL, Soliman H et al (2017) Differentiation between radiation necrosis and tumor progression using chemical exchange saturation transfer. Clin Cancer Res 23(14):3667–3675
Detsky JS, Keith J, Conklin J et al (2017) Differentiating radiation necrosis from tumor progression in brain metastases treated with stereotactic radiotherapy: utility of intravoxel incoherent motion perfusion MRI and correlation with histopathology. J Neurooncol 134(2):433–441
Askoxylakis V, Ferraro GB, Kodack DP et al (2016) Preclinical efficacy of ado-trastuzumab emtansine in the brain microenvironment. J Natl Cancer Institute. 108(2):djv313
Nordal RA, Wong CS (2005) Molecular targets in radiation-induced blood-brain barrier disruption. Int J Radiat Oncol Biol Phys. 62(1):279–287
Carlson JA, Nooruddin Z, Rusthoven C et al (2014) Trastuzumab emtansine and stereotactic radiosurgery: an unexpected increase in clinically significant brain edema. Neuro Oncol 16(7):1006–1009
Mills MN, Walker C, Thawani C et al (2021) Trastuzumab Emtansine (T-DM1) and stereotactic radiation in the management of HER2+ breast cancer brain metastases. BMC Cancer 21(1):1–8
Saura C, Oliveira M, Feng YH et al (2020) Neratinib plus capecitabine versus lapatinib plus capecitabine in HER2-positive metastatic breast cancer previously treated with≥ 2 HER2-directed regimens: phase III NALA trial. J Clin Oncol 38(27):3138
Murthy R, Borges VF, Conlin A et al (2018) Tucatinib with capecitabine and trastuzumab in advanced HER2-positive metastatic breast cancer with and without brain metastases: a non-randomised, open-label, phase 1b study. Lancet Oncol 19(7):880–888
Narayan P, Osgood CL, Singh H et al (2021) FDA approval summary: fam-trastuzumab deruxtecan-nxki for the treatment of unresectable or metastatic HER2-positive breast cancer. Clin Cancer Res 27(16):4478–4485
Meng Y, Reilly RM, Pezo RC et al (2021) MR-guided focused ultrasound enhances delivery of trastuzumab to Her2-positive brain metastases. Sci Trans Med. 13(615):eabj4011
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by BIS, HC, KJ and HS. The first draft of the manuscript was written by BIS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
BI (none), HC (none), KJJ (advisor: Amgen, AzstraZeneca, Apo Biologix, Eli Lily, Esai, Genomic Health, Knight Therapeutics,Merck. Myriad Genetics Inc, Noveratis, Purdue Pharma, Pfizer, Roche, Seagen; grant: Aztra Zeneca, Eli Lilly, Seagen), EW (none), SM (none), CLT (advisor: Sanofi, Elekta MR-linac consortium), JD (none), ZH (none), AJ (advisor: Gamma Knife Icon, honoraria: Astra Zeneca, BrainLAB, Elekta AB; grant: Elekta, BrainLAB, Varian), HS (none)
Ethical approval
This study received REB approval prior to study initiation.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Id Said, B., Chen, H., Jerzak, K.J. et al. Trastuzumab emtansine increases the risk of stereotactic radiosurgery-induced radionecrosis in HER2 + breast cancer. J Neurooncol 159, 177–183 (2022). https://doi.org/10.1007/s11060-022-04055-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04055-y