Abstract
Purpose
Glioblastoma (GBM) is a devastating neuro-oncologic disease with invariably poor prognosis. Despite this, research shows patients have unrealistic perceptions of their prognosis, which may relate in part to communication patterns between patients, caregivers and oncologists. The purpose of this study was to examine communication processes and goals among patients, caregivers, and oncologists to elucidate drivers of prognostic understanding (PU) in the context of recurrent GBM.
Methods
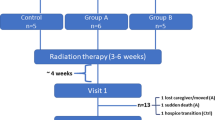
This was a prospective, multi-center study enrolling adult patients with GBM, caregivers, and oncologists, who independently reported the content of a specific discussion involving the disclosure of GBM recurrence. Communication processes and goals were characterized for each participant, and concordance between all dyads and patient-caregiver-oncologist triads were calculated.
Results
Seventeen patient, caregiver, and oncologist triads were analyzed. At the individual level, three (17.6%) patients and 8 (47.1%) caregivers reported having discussed prognosis during the clinical encounter, as compared to ten oncologists (58.8%). Seven patients (41.2%) and 5 caregivers (29.4%), versus thirteen oncologists (76.5%) reported ever discussing prognosis or life expectancy at previous appointments. Generally, patient-caregiver concordance (i.e., both answered the same) regarding communication goals and processes was low. Triads showed limited concordant responses in discussing curability (n = 5), prognosis (n = 4), end-of-life treatment goals (n = 4), and ever discussing prognosis (n = 3).
Conclusion
Patients, caregivers and oncologists had discordant views regarding communication processes and prognostic goals, even when recalling a single discussion. This study highlights the importance of clear and frequent communication about prognosis, and the need for further research on communication and PU in the neuro-oncology setting.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Urbańska K et al (2014) Glioblastoma multiforme—an overview. Contemp Oncol (Pozn) 18(5):307–312
Stupp R et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Gilbert MR et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370(8):699–708
Gilbert MR et al (2013) Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol 31(32):4085–4091
Masterson MP et al (2018) Don’t shoot the messenger: experiences of delivering prognostic information in the context of advanced cancer. Am J Hosp Palliat Care 35(12):1526–1531
Committee on Approaching Death: Addressing Key End of Life, I. and M. Institute of, in Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. 2015, National Academies Press (US) Copyright 2015 by the National Academy of Sciences. All Rights Reserved: Washington (DC)
Innes S, Payne S (2009) Advanced cancer patients’ prognostic information preferences: a review. Palliat Med 23(1):29–39
Malhotra K et al (2019) Prognostic accuracy of patients, caregivers, and oncologists in advanced cancer. Cancer 125(15):2684–2692
Tang ST et al (2018) Accurate prognostic awareness facilitates, whereas better quality of life and more anxiety symptoms hinder end-of-life care discussions: a longitudinal survey study in terminally ill cancer patients’ last six months of life. J Pain Symptom Manag 55(4):1068–1076
Epstein AS et al (2016) Discussions of life expectancy and changes in illness understanding in patients with advanced cancer. J Clin Oncol 34(20):2398–2403
Cohen SM et al (2018) Being present: oncologists’ role in promoting advanced cancer patients’ illness understanding. Cancer Med 7(4):1511–1518
Enzinger AC et al (2015) Outcomes of prognostic disclosure: associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol 33(32):3809–3816
Mack JW et al (2010) End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 28(7):1203–1208
Fenton JJ et al (2018) Impact of prognostic discussions on the patient-physician relationship: prospective Cohort study. J Clin Oncol 36(3):225–230
Shen MJ, Trevino KM, Prigerson HG (2018) The interactive effect of advanced cancer patient and caregiver prognostic understanding on patients’ completion of Do Not Resuscitate orders. Psychooncology 27(7):1765–1771
Trevino KM et al (2019) Association between advanced cancer patient-caregiver agreement regarding prognosis and hospice enrollment. Cancer 125(18):3259–3265
Diamond EL et al (2017) Prognostic awareness, prognostic communication, and cognitive function in patients with malignant glioma. Neuro Oncol 19(11):1532–1541
Forst DA et al (2020) Perceptions of prognosis and goal of treatment in patients with malignant gliomas and their caregivers. Neurooncol Pract 7(5):490–497
Prigerson HGPI. Black-white difference in advance cancer communication, acceptance, and care (Project No. 3R01CA106370 [Grant]. 2010–2015.
Wen FH et al (2019) Evolution and predictors of patient-caregiver concordance on states of life-sustaining treatment preferences over terminally ill cancer patients’ last six months of life. J Palliat Med 22(1):25–33
Loh KP et al (2021) Caregiver-oncologist prognostic concordance, caregiver mastery, and caregiver psychological health and quality of life. Oncologist 26(4):310–317
Derry HM et al (2019) Associations between anxiety, poor prognosis, and accurate understanding of scan results among advanced cancer patients. J Palliat Med 22(8):961–965
Loh KP et al (2019) Beliefs about advanced cancer curability in older patients, their caregivers, and oncologists. Oncologist 24(6):e292–e302
Applebaum AJ et al (2018) Prognostic awareness and communication preferences among caregivers of patients with malignant glioma. Psychooncology 27(3):817–823
Sharma A et al (2021) How much time do we have? Longitudinal perception of prognosis in newly-diagnosed high grade glioma patients and caregivers compared to clinicians. J Neurooncol 152(2):313–323
Epstein AS et al (2021) Development of the oncolo-GIST (“Giving Information Strategically & Transparently”) intervention manual for oncologist skills training in advanced cancer prognostic information communication. J Pain Symptom Manag 62(1):10–19
Funding
NIH P30 CA008748, NIH T32 CA009461 (L.E.W), American Society of Clinical Oncology Career Development Award (E.L.D).
Author information
Authors and Affiliations
Contributions
ED, HP, KP, AA, and AR designed the study. ED, AT, and TW collected data. JB, AS, LW, KP, AA, and AR analyzed the data. ED, LW, HP, KP, AR, and AA interpreted the data. LW, LP, AA, HP, KP, AR, and ED wrote the manuscript. All authors revised and approved of the final manuscript.
Corresponding author
Ethics declarations
Competing interest
Dr. Diamond discloses unpaid editorial support from Pfizer, Inc, and paid advisory board membership for Day One Biopharmaceuticals and Springworks Therapeutics, both outside the submitted work. Dr. Applebaum receives support from Bluenote Therapeutics. Dr. Walbert discloses paid advisory board membership for AstraZeneca and work for NovoCure.
Ethical approval
This study was approved by the ethics at each institution (IRB Number 15-034 at Memorial Sloan Kettering Cancer Center; IRB number 17-0540 at University of Vermont, IRB number 11458 at Henry Ford Health System).
Informed consent
Informed consent was obtained from all individual participants (patients, caregivers, and physicians) included in the study. Consent for publication was obtained via informed consent and all data presented have been de-identified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Walsh, L.E., Polacek, L.C., Panageas, K. et al. Coping with glioblastoma: prognostic communication and prognostic understanding among patients with recurrent glioblastoma, caregivers, and oncologists. J Neurooncol 158, 69–79 (2022). https://doi.org/10.1007/s11060-022-04010-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04010-x