Abstract
Introduction
Up to 34% of patients with medulloblastoma develop posterior fossa syndrome (PFS) following brain tumor resection and have increased risk of long-term neurocognitive impairments. Lack of agreement in conceptualization and diagnosis of PFS calls for improvements in diagnostic methods. The current study aimed to describe psychometric properties of a new posterior fossa syndrome questionnaire (PFSQ).
Methods
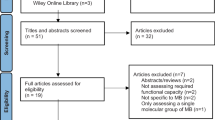
The PFSQ was informed by prior research and developed by a multidisciplinary team with subject matter expertise. Participants (N = 164; 63.4% Male; 78.7% White; Mage at diagnosis = 10.38 years, SD = 5.09, range 3–31 years) included patients with newly diagnosed medulloblastoma enrolled in the SJMB12 clinical trial. Forty-four patients (26.8%) were classified as having PFS based on attending physician’s post-surgical yes/no report. A PFSQ was completed by a neurologist within 2 weeks of coming to St. Jude Children’s Research Hospital for adjuvant treatment, irrespective of suspicion for PFS.
Results
PFSQ items ataxia (100.00%), dysmetria (95.45%), and speech/language changes (79.55%) were most sensitive. However, ataxia (26.50%) and dysmetria (46.61%) demonstrated low specificity. Speech/language changes (81.36%), mutism (95.76%), orofacial apraxia (98.29%) and irritability (96.61%) had high specificity. A principal component analysis found four components: (1) speech/language changes, (2) apraxias (including mutism), (3) motor/oromotor, and (4) emotional lability.
Conclusions
The PFSQ is a dimensional diagnostic approach that can be used to improve diagnostic consistency across clinical and research groups to help accelerate understanding of PFS etiology, identify surgical correlates of risk, predict long-term impairments, and develop targeted interventions. Additional measure validation, including correlation with symptom resolution, is required.


Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Khan RB, Patay Z, Kilmo P et al (2020) Clinical features, neurologic recovery, and risk prediction of post-operative posterior fossa syndrome: a prospective study. Neuro Oncol 22:28. https://doi.org/10.1093/neuonc/noab030
Gudrunardottir T, Morgan AT, Lux AL et al (2016) Consensus paper on post-operative pediatric cerebellar mutism syndrome: The Iceland Delphi results. Childs Nerv Syst 32(7):1195–1203. https://doi.org/10.1007/s00381-016-3093-3
De Smet HJ, Baillieux H, Wackenier P et al (2009) Long-term cognitive deficits following posterior fossa tumor resection: a neuropsychological and functional neuroimaging follow-up study. Neuropsychology 23(6):694–704. https://doi.org/10.1037/a0016106
Korah MP, Esiashvili N, Mazewski CM et al (2010) Incidence, risks, and sequelae of posterior fossa syndrome in pediatric medulloblastoma. Int J Radiat Oncol Biol Phys 77(1):106–112. https://doi.org/10.1016/j.ijrobp.2009.04.058
Gudrunardottir T, Sehested A, Juhler M, Schmiegelow K (2011) Cerebellar mutism: review of the literature. Childs Nerv Syst 27(3):355–363. https://doi.org/10.1007/s00381-010-1328-2
Patay Z (2015) Postoperative posterior fossa syndrome: Unraveling the etiology and underlying pathophysiology by using magnetic resonance imaging. Childs Nerv Syst 31(10):1853–1858. https://doi.org/10.1007/s00381-015-2796-1
Robertson PL, Muraszko KM, Holmes EJ et al (2006) Incidence and severity of postoperative cerebellar mutism syndrome in children with medulloblastoma: a prospective study by the Children’s Oncology Group. J Neurosurg 105(6 Suppl):444–451. https://doi.org/10.3171/ped.2006.105.6.444
Schreiber JE, Palmer SL, Conklin HM et al (2017) Posterior fossa syndrome and long-term neuropsychological outcomes among children treated for medulloblastoma on a multi-institutional, prospective study. Neuro Oncol 19(12):1673–1682. https://doi.org/10.1093/neuonc/nox135
Wolfe-Christensen C, Mullins L, Scott J, McNall-Knapp R (2007) Persistent psychosocial problems in children who develop posterior fossa syndrome after medulloblastoma resection. Pediatr Blood Cancer 49(5):723–726. https://doi.org/10.1002/pbc.21084
Wickenhauser ME, Khan RB, Raches D et al (2020) Characterizing posterior fossa syndrome: a survey of experts. Pediatr Neurol 104:19–22. https://doi.org/10.1016/j.pediatrneurol.2019.11.007
Hoche F, Guell X, Vangel MG, Sherman JC, Schmahmann JD (2018) The cerebellar cognitive affective/Schmahmann syndrome scale. Brain 141(1):248–370. https://doi.org/10.1093/brain/awx317
Schmahmann JD (2020) Pediatric post-operative cerebellar mutism syndrome, cerebellar cognitive affective syndrome, and posterior fossa syndrome: historical review and proposed resolution to guide future study. Childs Nerv Syst 36(6):1205–1214
Catsman-Berrevoets C, Patay Z (2018) Cerebellar mutism syndrome. Hand Clin Neurol 155:273–288. https://doi.org/10.1007/s00381-019-04253-6
Heitzer AM, Ashford JM, Harel BT et al (2019) Computerized assessment of cognitive impairment among children undergoing radiation therapy for medulloblastoma. J Neurooncol 141(2):403–411. https://doi.org/10.1007/s11060-018-03046-2
Pituch KA, Stevens JP (2016) Applied multivariate statistics for the social sciences: analyses with SAS and IBM’s SPSS, 6th edn. Routledge, London
Acknowledgements
The authors thank the patients and families who participated in the SJMB12 clinical trial. We also thank our multidisciplinary team members for their valuable contributions to this work.
Funding
This work was supported, in part, by the National Cancer Institute (St. Jude Cancer Center Support [CORE] Grant [P30-CA21765]) and the American Lebanese Syrian Associated Charities (ALSAC).
Author information
Authors and Affiliations
Contributions
RBK, DR, and HMC originally conceived the idea for the study and acquired study data with the help of GWR, AG, and KL. MEW, JMA, KMWR, and HMC were involved in all aspects of the study including design of the work, data analysis, interpretation, and final manuscript preparation. All authors contributed to writing and editing, and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of St. Jude Children’s Research Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wickenhauser, M.E., Khan, R.B., Raches, D. et al. The posterior fossa syndrome questionnaire: using science to inform practice. J Neurooncol 157, 465–473 (2022). https://doi.org/10.1007/s11060-022-03990-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-03990-0