Abstract
Patients with human epidermal growth factor receptor 2 (HER2)-positive breast cancer are at a particularly high risk of breast cancer brain metastasis (BCBM) and leptomeningeal disease (LMD). Improvements in systemic therapy have translated to improved survival for patients with HER2-positive BCBM and LMD. However, the optimal management of these cases is rapidly evolving and requires a multidisciplinary approach. Herein, a team of radiation oncologists, medical oncologists, neuro-oncologists, and breast surgeon created a review of the evolving management of HER2-positive BCBM and LMD. We assess the epidemiology, diagnosis, and evolving treatment options for patients with HER2-positive BCBM and LMD, as well as the ongoing prospective clinical trials enrolling these patients. The management of HER2-positive BCBM and LMD represents an increasingly common challenge that involves the coordination of local and systemic therapy. Advances in systemic therapy have resulted in an improved prognosis, and promising targeted therapies currently under prospective investigation have the potential to further benefit these patients.

Similar content being viewed by others
References
Ross JS, Slodkowska EA, Symmans WF, Pusztai L, Ravdin PM, Hortobagyi GN (2009) The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist 14(4):320–368. https://doi.org/10.1634/theoncologist.2008-0230
Azim HA, Abdel-Malek R, Kassem L (2018) Predicting brain metastasis in breast cancer patients: stage versus biology. Clin Breast Cancer 18(2):e187–e195. https://doi.org/10.1016/j.clbc.2017.08.004
Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A, Heeson S, Clark E, Ross G, Benyunes MC, Cortes J (2015) Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med 372(8):724–734. https://doi.org/10.1056/NEJMoa1413513
Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, Pegram M, Oh DY, Dieras V, Guardino E, Fang L, Lu MW, Olsen S, Blackwell K (2012) Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med 367(19):1783–1791. https://doi.org/10.1056/NEJMoa1209124
Krop IE, Kim SB, Martin AG, LoRusso PM, Ferrero JM, Badovinac-Crnjevic T, Hoersch S, Smitt M, Wildiers H (2017) Trastuzumab emtansine versus treatment of physician’s choice in patients with previously treated HER2-positive metastatic breast cancer (TH3RESA): final overall survival results from a randomised open-label phase 3 trial. Lancet Oncol 18(6):743–754. https://doi.org/10.1016/S1470-2045(17)30313-3
Mehta AI, Brufsky AM, Sampson JH (2013) Therapeutic approaches for HER2-positive brain metastases: circumventing the blood-brain barrier. Cancer Treat Rev 39(3):261–269. https://doi.org/10.1016/j.ctrv.2012.05.006
Stemmler HJ, Schmitt M, Willems A, Bernhard H, Harbeck N, Heinemann V (2007) Ratio of trastuzumab levels in serum and cerebrospinal fluid is altered in HER2-positive breast cancer patients with brain metastases and impairment of blood-brain barrier. Anticancer Drugs 18(1):23–28. https://doi.org/10.1097/01.cad.0000236313.50833.ee
Kabraji S, Ni J, Lin NU, Xie S, Winer EP, Zhao JJ (2018) Drug resistance in HER2-positive breast cancer brain metastases: blame the barrier or the brain? Clin Cancer Res 24(8):1795–1804. https://doi.org/10.1158/1078-0432.CCR-17-3351
Kuksis M, Gao Y, Tran W, Hoey C, Kiss A, Komorowski AS, Dhaliwal AJ, Sahgal A, Das S, Chan KK, Jerzak KJ (2021) The incidence of brain metastases among patients with metastatic breast cancer: a systematic review and meta-analysis. Neuro Oncol 23(6):894–904. https://doi.org/10.1093/neuonc/noaa285
Kim YJ, Kim JS, Kim IA (2018) Molecular subtype predicts incidence and prognosis of brain metastasis from breast cancer in SEER database. J Cancer Res Clin Oncol 144(9):1803–1816. https://doi.org/10.1007/s00432-018-2697-2
National Comprehensive Cancer Network Guidelines: Breast Cancer (2021) https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
Franzoi MA, Hortobagyi GN (2019) Leptomeningeal carcinomatosis in patients with breast cancer. Crit Rev Oncol Hematol 135:85–94. https://doi.org/10.1016/j.critrevonc.2019.01.020
Griguolo G, Pouderoux S, Dieci MV, Jacot W, Bourgier C, Miglietta F, Firmin N, Conte P, Viala M, Guarneri V, Darlix A (2018) Clinicopathological and treatment-associated prognostic factors in patients with breast cancer leptomeningeal metastases in relation to tumor biology. Oncologist 23(11):1289–1299. https://doi.org/10.1634/theoncologist.2018-0200
Figura NB, Rizk VT, Armaghani AJ, Arrington JA, Etame AB, Han HS, Czerniecki BJ, Forsyth PA, Ahmed KA (2019) Breast leptomeningeal disease: a review of current practices and updates on management. Breast Cancer Res Treat 177(2):277–294. https://doi.org/10.1007/s10549-019-05317-6
Mills MN, Figura NB, Arrington JA, Yu HM, Etame AB, Vogelbaum MA, Soliman H, Czerniecki BJ, Forsyth PA, Han HS, Ahmed KA (2020) Management of brain metastases in breast cancer: a review of current practices and emerging treatments. Breast Cancer Res Treat 180(2):279–300. https://doi.org/10.1007/s10549-020-05552-2
Ramakrishna N, Temin S, Chandarlapaty S, Crews JR, Davidson NE, Esteva FJ, Giordano SH, Kirshner JJ, Krop IE, Levinson J, Modi S, Patt DA, Perlmutter J, Winer EP, Lin NU (2018) Recommendations on disease management for patients with advanced human epidermal growth factor receptor 2-positive breast cancer and brain metastases: ASCO clinical practice guideline update. J Clin Oncol 36(27):2804–2807. https://doi.org/10.1200/JCO.2018.79.2713
Bargmann CI, Hung MC, Weinberg RA (1986) The neu oncogene encodes an epidermal growth factor receptor-related protein. Nature 319(6050):226–230. https://doi.org/10.1038/319226a0
Sirkisoon SR, Carpenter RL, Rimkus T, Miller L, Metheny-Barlow L, Lo HW (2016) EGFR and HER2 signaling in breast cancer brain metastasis. Front Biosci 8:245–263. https://doi.org/10.2741/E765
Harari D, Yarden Y (2000) Molecular mechanisms underlying ErbB2/HER2 action in breast cancer. Oncogene 19(53):6102–6114. https://doi.org/10.1038/sj.onc.1203973
Hosonaga M, Saya H, Arima Y (2020) Molecular and cellular mechanisms underlying brain metastasis of breast cancer. Cancer Metastasis Rev 39(3):711–720. https://doi.org/10.1007/s10555-020-09881-y
Vareslija D, Priedigkeit N, Fagan A, Purcell S, Cosgrove N, O’Halloran PJ, Ward E, Cocchiglia S, Hartmaier R, Castro CA, Zhu L, Tseng GC, Lucas PC, Puhalla SL, Brufsky AM, Hamilton RL, Mathew A, Leone JP, Basudan A, Hudson L, Dwyer R, Das S, O’Connor DP, Buckley PG, Farrell M, Hill ADK, Oesterreich S, Lee AV, Young LS (2019) Transcriptome characterization of matched primary breast and brain metastatic tumors to detect novel actionable targets. J Natl Cancer Inst 111(4):388–398. https://doi.org/10.1093/jnci/djy110
Lunell NO, Pschera H, Zador G, Carlstrom K (1991) Evaluation of the possible interaction of the antifungal triazole SCH 39304 with oral contraceptives in normal healthy women. Gynecol Obstet Invest 32(2):91–97. https://doi.org/10.1159/000293003
Priedigkeit N, Hartmaier RJ, Chen Y, Vareslija D, Basudan A, Watters RJ, Thomas R, Leone JP, Lucas PC, Bhargava R, Hamilton RL, Chmielecki J, Puhalla SL, Davidson NE, Oesterreich S, Brufsky AM, Young L, Lee AV (2017) Intrinsic subtype switching and acquired ERBB2/HER2 amplifications and mutations in breast cancer brain metastases. JAMA Oncol 3(5):666–671. https://doi.org/10.1001/jamaoncol.2016.5630
Momeny M, Saunus JM, Marturana F, McCart Reed AE, Black D, Sala G, Iacobelli S, Holland JD, Yu D, Da Silva L, Simpson PT, Khanna KK, Chenevix-Trench G, Lakhani SR (2015) Heregulin-HER3-HER2 signaling promotes matrix metalloproteinase-dependent blood-brain-barrier transendothelial migration of human breast cancer cell lines. Oncotarget 6(6):3932–3946. https://doi.org/10.18632/oncotarget.2846
Zhang S, Huang WC, Zhang L, Zhang C, Lowery FJ, Ding Z, Guo H, Wang H, Huang S, Sahin AA, Aldape KD, Steeg PS, Yu D (2013) SRC family kinases as novel therapeutic targets to treat breast cancer brain metastases. Cancer Res 73(18):5764–5774. https://doi.org/10.1158/0008-5472.CAN-12-1803
Hackshaw MD, Danysh HE, Henderson M, Wang E, Tu N, Islam Z, Ladner A, Ritchey ME, Salas M (2021) Prognostic factors of brain metastasis and survival among HER2-positive metastatic breast cancer patients: a systematic literature review. BMC Cancer 21(1):967. https://doi.org/10.1186/s12885-021-08708-5
Hung MH, Liu CY, Shiau CY, Hsu CY, Tsai YF, Wang YL, Tai LC, King KL, Chao TC, Chiu JH, Su CH, Lo SS, Tzeng CH, Shyr YM, Tseng LM (2014) Effect of age and biological subtype on the risk and timing of brain metastasis in breast cancer patients. PLoS ONE 9(2):e89389. https://doi.org/10.1371/journal.pone.0089389
Graesslin O, Abdulkarim BS, Coutant C, Huguet F, Gabos Z, Hsu L, Marpeau O, Uzan S, Pusztai L, Strom EA, Hortobagyi GN, Rouzier R, Ibrahim NK (2010) Nomogram to predict subsequent brain metastasis in patients with metastatic breast cancer. J Clin Oncol 28(12):2032–2037. https://doi.org/10.1200/JCO.2009.24.6314
Jung JM, Kim S, Joo J, Shin KH, Gwak HS, Lee SH (2012) Incidence and risk factors for leptomeningeal carcinomatosis in breast cancer patients with parenchymal brain metastases. J Korean Neurosurg Soc 52(3):193–199. https://doi.org/10.3340/jkns.2012.52.3.193
Johnson MD, Avkshtol V, Baschnagel AM, Meyer K, Ye H, Grills IS, Chen PY, Maitz A, Olson RE, Pieper DR, Krauss DJ (2016) Surgical resection of brain metastases and the risk of leptomeningeal recurrence in patients treated with stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 94(3):537–543. https://doi.org/10.1016/j.ijrobp.2015.11.022
Yust-Katz S, Garciarena P, Liu D, Yuan Y, Ibrahim N, Yerushalmi R, Penas-Prado M, Groves MD (2013) Breast cancer and leptomeningeal disease (LMD): hormone receptor status influences time to development of LMD and survival from LMD diagnosis. J Neurooncol 114(2):229–235. https://doi.org/10.1007/s11060-013-1175-6
Trifiletti DM, Romano KD, Xu Z, Reardon KA, Sheehan J (2015) Leptomeningeal disease following stereotactic radiosurgery for brain metastases from breast cancer. J Neurooncol 124(3):421–427. https://doi.org/10.1007/s11060-015-1854-6
Suki D, Hatiboglu MA, Patel AJ, Weinberg JS, Groves MD, Mahajan A, Sawaya R (2009) Comparative risk of leptomeningeal dissemination of cancer after surgery or stereotactic radiosurgery for a single supratentorial solid tumor metastasis. Neurosurgery 64(4):664–674. https://doi.org/10.1227/01.NEU.0000341535.53720.3E
Prabhu RS, Turner BE, Asher AL, Marcrom SR, Fiveash JB, Foreman PM, Press RH, Patel KR, Curran WJ, Breen WG, Brown PD, Jethwa KR, Grills IS, Arden JD, Foster LM, Manning MA, Stern JD, Soltys SG, Burri SH (2019) A multi-institutional analysis of presentation and outcomes for leptomeningeal disease recurrence after surgical resection and radiosurgery for brain metastases. Neuro Oncol. https://doi.org/10.1093/neuonc/noz049
Shi S, Sandhu N, Jin MC, Wang E, Jaoude JA, Schofield K, Zhang C, Liu E, Gibbs IC, Hancock SL, Chang SD, Li G, Hayden-Gephart M, Adler JR, Soltys SG, Pollom EL (2020) Stereotactic radiosurgery for resected brain metastases: single-institutional experience of over 500 cavities. Int J Radiat Oncol Biol Phys 106(4):764–771. https://doi.org/10.1016/j.ijrobp.2019.11.022
Atalar B, Modlin LA, Choi CY, Adler JR, Gibbs IC, Chang SD, Harsh GRT, Li G, Nagpal S, Hanlon A, Soltys SG (2013) Risk of leptomeningeal disease in patients treated with stereotactic radiosurgery targeting the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys 87(4):713–718. https://doi.org/10.1016/j.ijrobp.2013.07.034
Routman DM, Yan E, Vora S, Peterson J, Mahajan A, Chaichana KL, Laack N, Brown PD, Parney IF, Burns TC, Trifiletti DM (2018) Preoperative stereotactic radiosurgery for brain metastases. Front Neurol 9:959. https://doi.org/10.3389/fneur.2018.00959
Sperduto PW, Mesko S, Li J, Cagney D, Aizer A, Lin NU, Nesbit E, Kruser TJ, Chan J, Braunstein S, Lee J, Kirkpatrick JP, Breen W, Brown PD, Shi D, Shih HA, Soliman H, Sahgal A, Shanley R, Sperduto W, Lou E, Everett A, Boggs DH, Masucci L, Roberge D, Remick J, Plichta K, Buatti JM, Jain S, Gaspar LE, Wu CC, Wang TJC, Bryant J, Chuong M, Yu J, Chiang V, Nakano T, Aoyama H, Mehta MP (2020) Beyond an updated graded prognostic assessment (breast GPA): A prognostic index and trends in treatment and survival in breast cancer brain metastases from 1985 to today. Int J Radiat Oncol Biol Phys 107(2):334–343. https://doi.org/10.1016/j.ijrobp.2020.01.051
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R (1997) Recursive partitioning analysis (RPA) of prognostic factors in three radiation therapy oncology group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37(4):745–751. https://doi.org/10.1016/s0360-3016(96)00619-0
Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70(2):510–514. https://doi.org/10.1016/j.ijrobp.2007.06.074
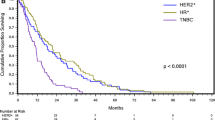
Mills MN, Thawani C, Figura NB, Oliver DE, Soyano AE, Etame A, Robinson TJ, Liu JK, Vogelbaum MA, Forsyth PA, Czerniecki BJ, Soliman HH, Han HS, Yu HM, Ahmed KA (2021) Breast cancer subtype predicts clinical outcomes after stereotactic radiation for brain metastases. J Neurooncol 152(3):591–601. https://doi.org/10.1007/s11060-021-03735-5
Carausu M, Carton M, Darlix A, Pasquier D, Leheurteur M, Debled M, Mouret-Reynier MA, Goncalves A, Dalenc F, Verret B, Campone M, Augereau P, Ferrero JM, Levy C, Fumet JD, Lefeuvre-Plesse C, Petit T, Uwer L, Jouannaud C, Larrouquere L, Chevrot M, Courtinard C, Cabel L (2021) Breast cancer patients treated with intrathecal therapy for leptomeningeal metastases in a large real-life database. ESMO Open 6(3):100150. https://doi.org/10.1016/j.esmoop.2021.100150
Morikawa A, Jordan L, Rozner R, Patil S, Boire A, Pentsova E, Seidman AD (2017) Characteristics and outcomes of patients with breast cancer with leptomeningeal metastasis. Clin Breast Cancer 17(1):23–28. https://doi.org/10.1016/j.clbc.2016.07.002
Abouharb S, Ensor J, Loghin ME, Katz R, Moulder SL, Esteva FJ, Smith B, Valero V, Hortobagyi GN, Melhem-Bertrandt A (2014) Leptomeningeal disease and breast cancer: the importance of tumor subtype. Breast Cancer Res Treat 146(3):477–486. https://doi.org/10.1007/s10549-014-3054-z
Gauthier H, Guilhaume MN, Bidard FC, Pierga JY, Girre V, Cottu PH, Laurence V, Livartowski A, Mignot L, Dieras V (2010) Survival of breast cancer patients with meningeal carcinomatosis. Ann Oncol 21(11):2183–2187. https://doi.org/10.1093/annonc/mdq232
National Comprehensive Cancer Network Guidelines. Non-Small Cell Lung Cancer. (version 7.2021)
National Comprehensive Cancer Network Guidelines. Melanoma. (version 2.2021)
Mills MN, Potluri TK, Kawahara Y, Fahey M, Figura NB, Soyano AE, Washington IR, Diaz R, Oliver DE, Yu HM, Etame AB, Vogelbaum MA, Czerniecki BJ, Arrington JA, Sahebjam S, Forsyth PA, Soliman HH, Han HS, Ahmed KA (2021) The presentation of brain metastases in melanoma, non-small cell lung cancer, and breast cancer and potential implications for screening brain MRIs. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-021-06420-3
Cagney DN, Martin AM, Catalano PJ, Brown PD, Alexander BM, Lin NU, Aizer AA (2018) Implications of screening for brain metastases in patients with breast cancer and non-small cell lung cancer. JAMA Oncol 4(7):1001–1003. https://doi.org/10.1001/jamaoncol.2018.0813
Le Rhun E, Weller M, Brandsma D, Van den Bent M, de Azambuja E, Henriksson R, Boulanger T, Peters S, Watts C, Wick W, Wesseling P, Ruda R, Preusser M, Board EE (2017) EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann Oncol 28(4):84–99. https://doi.org/10.1093/annonc/mdx221
Angus L, Martens JWM, van den Bent MJ, Sillevis Smitt PAE, Sleijfer S, Jager A (2019) Novel methods to diagnose leptomeningeal metastases in breast cancer. Neuro Oncol 21(4):428–439. https://doi.org/10.1093/neuonc/noy186
Le Rhun E, Devos P, Weller J, Seystahl K, Mo F, Compter A, Berghoff AS, Jongen JLM, Wolpert F, Ruda R, Brandsma D, van den Bent M, Preusser M, Herrlinger U, Weller M (2021) Prognostic validation and clinical implications of the EANO ESMO classification of leptomeningeal metastasis from solid tumors. Neuro Oncol 23(7):1100–1112. https://doi.org/10.1093/neuonc/noaa298
Herrlinger U, Wiendl H, Renninger M, Forschler H, Dichgans J, Weller M (2004) Vascular endothelial growth factor (VEGF) in leptomeningeal metastasis: diagnostic and prognostic value. Br J Cancer 91(2):219–224. https://doi.org/10.1038/sj.bjc.6601953
Le Rhun E, Kramar A, Salingue S, Girot M, Rodrigues I, Mailliez A, Zairi F, Bakhache E, Robin YM, Taillibert S, Dubois F, Bonneterre J, Chamberlain MC (2014) CSF CA 15–3 in breast cancer-related leptomeningeal metastases. J Neurooncol 117(1):117–124. https://doi.org/10.1007/s11060-014-1361-1
Corsini E, Bernardi G, Gaviani P, Silvani A, de Grazia U, Ciusani E, Croci D, Salmaggi A (2009) Intrathecal synthesis of tumor markers is a highly sensitive test in the diagnosis of leptomeningeal metastasis from solid cancers. Clin Chem Lab Med 47(7):874–879. https://doi.org/10.1515/CCLM.2009.183
van Bussel MTJ, Pluim D, Bol M, Beijnen JH, Schellens JHM, Brandsma D (2018) EpCAM-based assays for epithelial tumor cell detection in cerebrospinal fluid. J Neurooncol 137(1):1–10. https://doi.org/10.1007/s11060-017-2691-6
Milojkovic Kerklaan B, Pluim D, Bol M, Hofland I, Westerga J, van Tinteren H, Beijnen JH, Boogerd W, Schellens JH, Brandsma D (2016) EpCAM-based flow cytometry in cerebrospinal fluid greatly improves diagnostic accuracy of leptomeningeal metastases from epithelial tumors. Neuro Oncol 18(6):855–862. https://doi.org/10.1093/neuonc/nov273
Pessoa LS, Heringer M, Ferrer VP (2020) ctDNA as a cancer biomarker: A broad overview. Crit Rev Oncol Hematol 155:103109. https://doi.org/10.1016/j.critrevonc.2020.103109
De Mattos-Arruda L, Mayor R, Ng CKY, Weigelt B, Martinez-Ricarte F, Torrejon D, Oliveira M, Arias A, Raventos C, Tang J, Guerini-Rocco E, Martinez-Saez E, Lois S, Marin O, de la Cruz X, Piscuoglio S, Towers R, Vivancos A, Peg V, RamonyCajal S, Carles J, Rodon J, Gonzalez-Cao M, Tabernero J, Felip E, Sahuquillo J, Berger MF, Cortes J, Reis-Filho JS, Seoane J (2015) Cerebrospinal fluid-derived circulating tumour DNA better represents the genomic alterations of brain tumours than plasma. Nat Commun 6:8839. https://doi.org/10.1038/ncomms9839
Boire A, Brandsma D, Brastianos PK, Le Rhun E, Ahluwalia M, Junck L, Glantz M, Groves MD, Lee EQ, Lin N, Raizer J, Ruda R, Weller M, Van den Bent MJ, Vogelbaum MA, Chang S, Wen PY, Soffietti R (2019) Liquid biopsy in central nervous system metastases: a RANO review and proposals for clinical applications. Neuro Oncol 21(5):571–584. https://doi.org/10.1093/neuonc/noz012
Lin NU, Lee EQ, Aoyama H, Barani IJ, Barboriak DP, Baumert BG, Bendszus M, Brown PD, Camidge DR, Chang SM, Dancey J, de Vries EG, Gaspar LE, Harris GJ, Hodi FS, Kalkanis SN, Linskey ME, Macdonald DR, Margolin K, Mehta MP, Schiff D, Soffietti R, Suh JH, van den Bent MJ, Vogelbaum MA, Wen PY (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16(6):e270-278. https://doi.org/10.1016/S1470-2045(15)70057-4
Galldiks N, Kocher M, Ceccon G, Werner JM, Brunn A, Deckert M, Pope WB, Soffietti R, Le Rhun E, Weller M, Tonn JC, Fink GR, Langen KJ (2020) Imaging challenges of immunotherapy and targeted therapy in patients with brain metastases: response, progression, and pseudoprogression. Neuro Oncol 22(1):17–30. https://doi.org/10.1093/neuonc/noz147
Okada H, Weller M, Huang R, Finocchiaro G, Gilbert MR, Wick W, Ellingson BM, Hashimoto N, Pollack IF, Brandes AA, Franceschi E, Herold-Mende C, Nayak L, Panigrahy A, Pope WB, Prins R, Sampson JH, Wen PY, Reardon DA (2015) Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol 16(15):e534–e542. https://doi.org/10.1016/S1470-2045(15)00088-1
Chamberlain M, Soffietti R, Raizer J, Ruda R, Brandsma D, Boogerd W, Taillibert S, Groves MD, Le Rhun E, Junck L, van den Bent M, Wen PY, Jaeckle KA (2014) Leptomeningeal metastasis: a Response Assessment in Neuro-Oncology critical review of endpoints and response criteria of published randomized clinical trials. Neuro Oncol 16(9):1176–1185. https://doi.org/10.1093/neuonc/nou089
Chamberlain M, Junck L, Brandsma D, Soffietti R, Ruda R, Raizer J, Boogerd W, Taillibert S, Groves MD, Le Rhun E, Walker J, van den Bent M, Wen PY, Jaeckle KA (2017) Leptomeningeal metastases: a RANO proposal for response criteria. Neuro Oncol 19(4):484–492. https://doi.org/10.1093/neuonc/now183
Le Rhun E, Devos P, Boulanger T, Smits M, Brandsma D, Ruda R, Furtner J, Hempel JM, Postma TJ, Roth P, Snijders TJ, Winkler F, Winklhofer S, Castellano A, Hattingen E, Capellades J, Gorlia T, Van den Bent M, Wen PY, Bendszus M, Weller M (2019) The RANO Leptomeningeal Metastasis Group proposal to assess response to treatment: lack of feasibility and clinical utility and a revised proposal. Neuro Oncol 21(5):648–658. https://doi.org/10.1093/neuonc/noz024
Pellerino A, Interno V, Mo F, Franchino F, Soffietti R, Ruda R (2020) Management of brain and leptomeningeal metastases from breast cancer. Int J Mol Sci 21:22. https://doi.org/10.3390/ijms21228534
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500. https://doi.org/10.1056/NEJM199002223220802
Vecht CJ, Haaxma-Reiche H, Noordijk EM, Padberg GW, Voormolen JH, Hoekstra FH, Tans JT, Lambooij N, Metsaars JA, Wattendorff AR et al (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 33(6):583–590. https://doi.org/10.1002/ana.410330605
Le Rhun E, Guckenberger M, Smits M, Dummer R, Bachelot T, Sahm F, Galldiks N, de Azambuja E, Berghoff AS, Metellus P, Peters S, Hong YK, Winkler F, Schadendorf D, van den Bent M, Seoane J, Stahel R, Minniti G, Wesseling P, Weller M, Preusser M, Board EE (2021) EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann Oncol 32(11):1332–1347. https://doi.org/10.1016/j.annonc.2021.07.016
Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, Kryscio RJ, Markesbery WR, Foon KA, Young B (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280(17):1485–1489. https://doi.org/10.1001/jama.280.17.1485
Brown PD, Pugh S, Laack NN, Wefel JS, Khuntia D, Meyers C, Choucair A, Fox S, Suh JH, Roberge D, Kavadi V, Bentzen SM, Mehta MP, Watkins-Bruner D, G Radiation Therapy Oncology (2013) Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol 15(10):1429–1437. https://doi.org/10.1093/neuonc/not114
Yang WC, Chen YF, Yang CC, Wu PF, Chan HM, Chen JL, Chen GY, Cheng JC, Kuo SH, Hsu FM (2021) Hippocampal avoidance whole-brain radiotherapy without memantine in preserving neurocognitive function for brain metastases: a phase II blinded randomized trial. Neuro Oncol 23(3):478–486. https://doi.org/10.1093/neuonc/noaa193
Brown PD, Gondi V, Pugh S, Tome WA, Wefel JS, Armstrong TS, Bovi JA, Robinson C, Konski A, Khuntia D, Grosshans D, Benzinger TLS, Bruner D, Gilbert MR, Roberge D, Kundapur V, Devisetty K, Shah S, Usuki K, Anderson BM, Stea B, Yoon H, Li J, Laack NN, Kruser TJ, Chmura SJ, Shi W, Deshmukh S, Mehta MP, Kachnic LA (2020) Hippocampal avoidance during whole-brain radiotherapy plus memantine for patients with brain metastases: phase III trial NRG oncology CC001. J Clin Oncol 38(10):1019–1029. https://doi.org/10.1200/JCO.19.02767
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363(9422):1665–1672. https://doi.org/10.1016/S0140-6736(04)16250-8
Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK, Carrero XW, Barker FG 2nd, Deming R, Burri SH, Menard C, Chung C, Stieber VW, Pollock BE, Galanis E, Buckner JC, Asher AL (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316(4):401–409. https://doi.org/10.1001/jama.2016.9839
Brown PD, Ballman KV, Cerhan JH, Anderson SK, Carrero XW, Whitton AC, Greenspoon J, Parney IF, Laack NNI, Ashman JB, Bahary JP, Hadjipanayis CG, Urbanic JJ, Barker FG 2nd, Farace E, Khuntia D, Giannini C, Buckner JC, Galanis E, Roberge D (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1049–1060. https://doi.org/10.1016/S1470-2045(17)30441-2
Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, Kawagishi J, Yamanaka K, Sato Y, Jokura H, Yomo S, Nagano O, Kenai H, Moriki A, Suzuki S, Kida Y, Iwai Y, Hayashi M, Onishi H, Gondo M, Sato M, Akimitsu T, Kubo K, Kikuchi Y, Shibasaki T, Goto T, Takanashi M, Mori Y, Takakura K, Saeki N, Kunieda E, Aoyama H, Momoshima S, Tsuchiya K (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15(4):387–395. https://doi.org/10.1016/S1470-2045(14)70061-0
Hughes RT, Masters AH, McTyre ER, Farris MK, Chung C, Page BR, Kleinberg LR, Hepel J, Contessa JN, Chiang V, Ruiz J, Watabe K, Su J, Fiveash JB, Braunstein S, Chao S, Attia A, Ayala-Peacock DN, Chan MD (2019) Initial SRS for patients with 5 to 15 brain metastases: results of a multi-institutional experience. Int J Radiat Oncol Biol Phys 104(5):1091–1098. https://doi.org/10.1016/j.ijrobp.2019.03.052
Kohutek ZA, Yamada Y, Chan TA, Brennan CW, Tabar V, Gutin PH, Yang TJ, Rosenblum MK, Ballangrud A, Young RJ, Zhang Z, Beal K (2015) Long-term risk of radionecrosis and imaging changes after stereotactic radiosurgery for brain metastases. J Neurooncol 125(1):149–156. https://doi.org/10.1007/s11060-015-1881-3
Lockman PR, Mittapalli RK, Taskar KS, Rudraraju V, Gril B, Bohn KA, Adkins CE, Roberts A, Thorsheim HR, Gaasch JA, Huang S, Palmieri D, Steeg PS, Smith QR (2010) Heterogeneous blood-tumor barrier permeability determines drug efficacy in experimental brain metastases of breast cancer. Clin Cancer Res 16(23):5664–5678. https://doi.org/10.1158/1078-0432.CCR-10-1564
Babak MV, Zalutsky MR, Balyasnikova IV (2020) Heterogeneity and vascular permeability of breast cancer brain metastases. Cancer Lett 489:174–181. https://doi.org/10.1016/j.canlet.2020.06.012
Teng F, Tsien CI, Lawrence TS, Cao Y (2017) Blood-tumor barrier opening changes in brain metastases from pre to one-month post radiation therapy. Radiother Oncol 125(1):89–93. https://doi.org/10.1016/j.radonc.2017.08.006
Swain SM, Baselga J, Miles D, Im YH, Quah C, Lee LF, Cortes J (2014) Incidence of central nervous system metastases in patients with HER2-positive metastatic breast cancer treated with pertuzumab, trastuzumab, and docetaxel: results from the randomized phase III study CLEOPATRA. Ann Oncol 25(6):1116–1121. https://doi.org/10.1093/annonc/mdu133
Lin NU, Pegram M, Sahebjam S, Ibrahim N, Fung A, Cheng A, Nicholas A, Kirschbrown W, Kumthekar P (2021) Pertuzumab plus high-dose trastuzumab in patients with progressive brain metastases and HER2-positive metastatic breast cancer: primary analysis of a phase II study. J Clin Oncol 39(24):2667–2675. https://doi.org/10.1200/JCO.20.02822
Olson EM, Abdel-Rasoul M, Maly J, Wu CS, Lin NU, Shapiro CL (2013) Incidence and risk of central nervous system metastases as site of first recurrence in patients with HER2-positive breast cancer treated with adjuvant trastuzumab. Ann Oncol 24(6):1526–1533. https://doi.org/10.1093/annonc/mdt036
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, Wolmark N, Rastogi P, Schneeweiss A, Redondo A, Fischer HH, Jacot W, Conlin AK, Arce-Salinas C, Wapnir IL, Jackisch C, DiGiovanna MP, Fasching PA, Crown JP, Wulfing P, Shao Z, Rota Caremoli E, Wu H, Lam LH, Tesarowski D, Smitt M, Douthwaite H, Singel SM, Geyer CE Jr, Investigators K (2019) Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med 380(7):617–628. https://doi.org/10.1056/NEJMoa1814017
Krop IE, Lin NU, Blackwell K, Guardino E, Huober J, Lu M, Miles D, Samant M, Welslau M, Dieras V (2015) Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann Oncol 26(1):113–119. https://doi.org/10.1093/annonc/mdu486
Montemurro F, Delaloge S, Barrios CH, Wuerstlein R, Anton A, Brain E, Hatschek T, Kelly CM, Pena-Murillo C, Yilmaz M, Donica M, Ellis P (2020) Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial(). Ann Oncol 31(10):1350–1358. https://doi.org/10.1016/j.annonc.2020.06.020
Di Leo A, Gomez HL, Aziz Z, Zvirbule Z, Bines J, Arbushites MC, Guerrera SF, Koehler M, Oliva C, Stein SH, Williams LS, Dering J, Finn RS, Press MF (2008) Phase III, double-blind, randomized study comparing lapatinib plus paclitaxel with placebo plus paclitaxel as first-line treatment for metastatic breast cancer. J Clin Oncol 26(34):5544–5552. https://doi.org/10.1200/JCO.2008.16.2578
Geyer CE, Forster J, Lindquist D, Chan S, Romieu CG, Pienkowski T, Jagiello-Gruszfeld A, Crown J, Chan A, Kaufman B, Skarlos D, Campone M, Davidson N, Berger M, Oliva C, Rubin SD, Stein S, Cameron D (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355(26):2733–2743. https://doi.org/10.1056/NEJMoa064320
Blackwell KL, Burstein HJ, Storniolo AM, Rugo HS, Sledge G, Aktan G, Ellis C, Florance A, Vukelja S, Bischoff J, Baselga J, O’Shaughnessy J (2012) Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 Study. J Clin Oncol 30(21):2585–2592. https://doi.org/10.1200/JCO.2011.35.6725
Iwata H, Narabayashi M, Ito Y, Saji S, Fujiwara Y, Usami S, Katsura K, Sasaki Y (2013) A phase II study of lapatinib for brain metastases in patients with HER2-overexpressing breast cancer following trastuzumab based systemic therapy and cranial radiotherapy: subset analysis of Japanese patients. Int J Clin Oncol 18(4):621–628. https://doi.org/10.1007/s10147-012-0444-2
Taskar KS, Rudraraju V, Mittapalli RK, Samala R, Thorsheim HR, Lockman J, Gril B, Hua E, Palmieri D, Polli JW, Castellino S, Rubin SD, Lockman PR, Steeg PS, Smith QR (2012) Lapatinib distribution in HER2 overexpressing experimental brain metastases of breast cancer. Pharm Res 29(3):770–781. https://doi.org/10.1007/s11095-011-0601-8
Bachelot T, Romieu G, Campone M, Dieras V, Cropet C, Dalenc F, Jimenez M, Le Rhun E, Pierga JY, Goncalves A, Leheurteur M, Domont J, Gutierrez M, Cure H, Ferrero JM, Labbe-Devilliers C (2013) Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol 14(1):64–71. https://doi.org/10.1016/S1470-2045(12)70432-1
Lin NU, Freedman RA, Ramakrishna N, Younger J, Storniolo AM, Bellon JR, Come SE, Gelman RS, Harris GJ, Henderson MA, Macdonald SM, Mahadevan A, Eisenberg E, Ligibel JA, Mayer EL, Moy B, Eichler AF, Winer EP (2013) A phase I study of lapatinib with whole brain radiotherapy in patients with Human Epidermal Growth Factor Receptor 2 (HER2)-positive breast cancer brain metastases. Breast Cancer Res Treat 142(2):405–414. https://doi.org/10.1007/s10549-013-2754-0
Awada A, Colomer R, Inoue K, Bondarenko I, Badwe RA, Demetriou G, Lee SC, Mehta AO, Kim SB, Bachelot T, Goswami C, Deo S, Bose R, Wong A, Xu F, Yao B, Bryce R, Carey LA (2016) Neratinib plus paclitaxel vs trastuzumab plus paclitaxel in previously untreated metastatic ERBB2-positive breast cancer: the NEfERT-T randomized clinical trial. JAMA Oncol 2(12):1557–1564. https://doi.org/10.1001/jamaoncol.2016.0237
Chan A, Moy B, Mansi J, Ejlertsen B, Holmes FA, Chia S, Iwata H, Gnant M, Loibl S, Barrios CH, Somali I, Smichkoska S, Martinez N, Alonso MG, Link JS, Mayer IA, Cold S, Murillo SM, Senecal F, Inoue K, Ruiz-Borrego M, Hui R, Denduluri N, Patt D, Rugo HS, Johnston SRD, Bryce R, Zhang B, Xu F, Wong A, Martin M (2021) Final efficacy results of neratinib in HER2-positive hormone receptor-positive early-stage breast cancer from the phase III ExteNET Trial. Clin Breast Cancer 21(1):80–91. https://doi.org/10.1016/j.clbc.2020.09.014
Saura C, Oliveira M, Feng YH, Dai MS, Chen SW, Hurvitz SA, Kim SB, Moy B, Delaloge S, Gradishar W, Masuda N, Palacova M, Trudeau ME, Mattson J, Yap YS, Hou MF, De Laurentiis M, Yeh YM, Chang HT, Yau T, Wildiers H, Haley B, Fagnani D, Lu YS, Crown J, Lin J, Takahashi M, Takano T, Yamaguchi M, Fujii T, Yao B, Bebchuk J, Keyvanjah K, Bryce R, Brufsky A, Investigators N (2020) Neratinib plus capecitabine versus lapatinib plus capecitabine in HER2-positive metastatic breast cancer previously treated with >/= 2 HER2-directed regimens: phase III NALA trial. J Clin Oncol 38(27):3138–3149. https://doi.org/10.1200/JCO.20.00147
Hurvitz SA, Saura C, Oliveira M, Trudeau ME, Moy B, Delaloge S, Gradishar W, Kim SB, Haley B, Ryvo L, Dai MS, Milovanov V, Alarcon J, Kalmadi S, Cronemberger E, Souza C, Landeiro L, Bose R, Bebchuk J, Kabbinavar F, Bryce R, Keyvanjah K, Brufsky AM (2021) Efficacy of neratinib plus capecitabine in the subgroup of patients with central nervous system involvement from the NALA trial. Oncologist 26(8):e1327–e1338. https://doi.org/10.1002/onco.13830
Freedman RA, Gelman RS, Anders CK, Melisko ME, Parsons HA, Cropp AM, Silvestri K, Cotter CM, Componeschi KP, Marte JM, Connolly RM, Moy B, Van Poznak CH, Blackwell KL, Puhalla SL, Jankowitz RC, Smith KL, Ibrahim N, Moynihan TJ, O’Sullivan CC, Nangia J, Niravath P, Tung N, Pohlmann PR, Burns R, Rimawi MF, Krop IE, Wolff AC, Winer EP, Lin NU (2019) TBCRC 022: a phase II trial of neratinib and capecitabine for patients with human epidermal growth factor receptor 2-positive breast cancer and brain metastases. J Clin Oncol 37(13):1081–1089. https://doi.org/10.1200/JCO.18.01511
Schuler M, Wu YL, Hirsh V, O’Byrne K, Yamamoto N, Mok T, Popat S, Sequist LV, Massey D, Zazulina V, Yang JC (2016) First-line afatinib versus chemotherapy in patients with non-small cell lung cancer and common epidermal growth factor receptor gene mutations and brain metastases. J Thorac Oncol 11(3):380–390. https://doi.org/10.1016/j.jtho.2015.11.014
Reardon DA, Nabors LB, Mason WP, Perry JR, Shapiro W, Kavan P, Mathieu D, Phuphanich S, Cseh A, Fu Y, Cong J, Wind S, Eisenstat DD, Group BIT, the Canadian Brain Tumour C (2015) Phase I/randomized phase II study of afatinib, an irreversible ErbB family blocker, with or without protracted temozolomide in adults with recurrent glioblastoma. Neuro Oncol 17(3):430–439. https://doi.org/10.1093/neuonc/nou160
Cortes J, Dieras V, Ro J, Barriere J, Bachelot T, Hurvitz S, Le Rhun E, Espie M, Kim SB, Schneeweiss A, Sohn JH, Nabholtz JM, Kellokumpu-Lehtinen PL, Taguchi J, Piacentini F, Ciruelos E, Bono P, Ould-Kaci M, Roux F, Joensuu H (2015) Afatinib alone or afatinib plus vinorelbine versus investigator’s choice of treatment for HER2-positive breast cancer with progressive brain metastases after trastuzumab, lapatinib, or both (LUX-Breast 3): a randomised, open-label, multicentre, phase 2 trial. Lancet Oncol 16(16):1700–1710. https://doi.org/10.1016/S1470-2045(15)00373-3
Metzger Filho O, Leone JP, Li T, Tan-Wasielewski Z, Trippa L, Barry WT, Younger J, Lawler E, Walker L, Freedman RA, Tolaney SM, Krop I, Winer EP, Lin NU (2020) Phase I dose-escalation trial of tucatinib in combination with trastuzumab in patients with HER2-positive breast cancer brain metastases. Ann Oncol 31(9):1231–1239. https://doi.org/10.1016/j.annonc.2020.05.014
Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, Lin NU, Borges V, Abramson V, Anders C, Bedard PL, Oliveira M, Jakobsen E, Bachelot T, Shachar SS, Muller V, Braga S, Duhoux FP, Greil R, Cameron D, Carey LA, Curigliano G, Gelmon K, Hortobagyi G, Krop I, Loibl S, Pegram M, Slamon D, Palanca-Wessels MC, Walker L, Feng W, Winer EP (2020) Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med 382(7):597–609. https://doi.org/10.1056/NEJMoa1914609
Lin NU, Borges V, Anders C, Murthy RK, Paplomata E, Hamilton E, Hurvitz S, Loi S, Okines A, Abramson V, Bedard PL, Oliveira M, Mueller V, Zelnak A, DiGiovanna MP, Bachelot T, Chien AJ, O’Regan R, Wardley A, Conlin A, Cameron D, Carey L, Curigliano G, Gelmon K, Loibl S, Mayor J, McGoldrick S, An X, Winer EP (2020) Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol 38(23):2610–2619. https://doi.org/10.1200/jco.20.00775
Xu B, Yan M, Ma F, Hu X, Feng J, Ouyang Q, Tong Z, Li H, Zhang Q, Sun T, Wang X, Yin Y, Cheng Y, Li W, Gu Y, Chen Q, Liu J, Cheng J, Geng C, Qin S, Wang S, Lu J, Shen K, Liu Q, Wang X, Wang H, Luo T, Yang J, Wu Y, Yu Z, Zhu X, Chen C, Zou J, Investigators P (2021) Pyrotinib plus capecitabine versus lapatinib plus capecitabine for the treatment of HER2-positive metastatic breast cancer (PHOEBE): a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Oncol 22(3):351–360. https://doi.org/10.1016/S1470-2045(20)30702-6
Lin Y, Lin M, Zhang J, Wang B, Tao Z, Du Y, Zhang S, Cao J, Wang L, Hu X (2020) Real-world data of pyrotinib-based therapy in metastatic HER2-positive breast cancer: promising efficacy in lapatinib-treated patients and in brain metastasis. Cancer Res Treat 52(4):1059–1066. https://doi.org/10.4143/crt.2019.633
Anwar M, Chen Q, Ouyang D, Wang S, Xie N, Ouyang Q, Fan P, Qian L, Chen G, Zhou E, Guo L, Gu X, Ding B, Yang X, Liu L, Deng C, Xiao Z, Li J, Wang Y, Zeng S, Hu J, Zhou W, Qiu B, Wang Z, Weng J, Liu M, Li Y, Tang T, Wang J, Zhang H, Dai B, Tang W, Wu T, Xiao M, Li X, Liu H, Li L, Yi W (2021) Pyrotinib treatment in patients with HER2-positive metastatic breast cancer and brain metastasis: exploratory final analysis of real-world. Multicenter Data Clin Cancer Res 27(16):4634–4641. https://doi.org/10.1158/1078-0432.CCR-21-0474
Yan M, Ouyang Q, Sun T, Niu L, Yang J, Li L, Song Y, Hao C, Chen Z, Orlandi A, Ishii N, Takabe K, Franceschini G, Ricci F, Verschraegen C, Liu Z, Zhang M, Lv H, Liu L, Yang X, Xiao H, Gao Z, Li X, Dong F, Chen X, Qiao J, Zhang G (2022) Pyrotinib plus capecitabine for patients with human epidermal growth factor receptor 2-positive breast cancer and brain metastases (PERMEATE): a multicentre, single-arm, two-cohort, phase 2 trial. Lancet Oncol. https://doi.org/10.1016/S1470-2045(21)00716-6
Modi S, Saura C, Yamashita T, Park YH, Kim SB, Tamura K, Andre F, Iwata H, Ito Y, Tsurutani J, Sohn J, Denduluri N, Perrin C, Aogi K, Tokunaga E, Im SA, Lee KS, Hurvitz SA, Cortes J, Lee C, Chen S, Zhang L, Shahidi J, Yver A, Krop I, Investigators DE-B (2020) Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med 382(7):610–621. https://doi.org/10.1056/NEJMoa1914510
Jerusalem GHPY, Yamashita T, Hurvitz SA, Modi S, Andre F, Krop IE, Gonzalez X, Hall PS, You B, Saura C (2021) Trastuzumab deruxtecan (T-DXd) in patients with HER2+ metastatic breast cancer with brain metastases: a subgroup analysis of the DESTINY-Breast01 trial. J Clin Oncol 39(15 suppl):526. https://doi.org/10.1200/JCO.2021.39.15_suppl.526
Goldberg SB, Schalper KA, Gettinger SN, Mahajan A, Herbst RS, Chiang AC, Lilenbaum R, Wilson FH, Omay SB, Yu JB, Jilaveanu L, Tran T, Pavlik K, Rowen E, Gerrish H, Komlo A, Gupta R, Wyatt H, Ribeiro M, Kluger Y, Zhou G, Wei W, Chiang VL, Kluger HM (2020) Pembrolizumab for management of patients with NSCLC and brain metastases: long-term results and biomarker analysis from a non-randomised, open-label, phase 2 trial. Lancet Oncol 21(5):655–663. https://doi.org/10.1016/S1470-2045(20)30111-X
Tawbi HA, Forsyth PA, Hodi FS, Lao CD, Moschos SJ, Hamid O, Atkins MB, Lewis K, Thomas RP, Glaspy JA, Jang S, Algazi AP, Khushalani NI, Postow MA, Pavlick AC, Ernstoff MS, Reardon DA, Puzanov I, Kudchadkar RR, Tarhini AA, Sumbul A, Rizzo JI, Margolin KA (2021) Safety and efficacy of the combination of nivolumab plus ipilimumab in patients with melanoma and asymptomatic or symptomatic brain metastases (CheckMate 204). Neuro Oncol 23(11):1961–1973. https://doi.org/10.1093/neuonc/noab094
Loi S, Giobbie-Hurder A, Gombos A, Bachelot T, Hui R, Curigliano G, Campone M, Biganzoli L, Bonnefoi H, Jerusalem G, Bartsch R, Rabaglio-Poretti M, Kammler R, Maibach R, Smyth MJ, Di Leo A, Colleoni M, Viale G, Regan MM, Andre F, International Breast Cancer Study G, the Breast International G (2019) Pembrolizumab plus trastuzumab in trastuzumab-resistant, advanced, HER2-positive breast cancer (PANACEA): a single-arm, multicentre, phase 1b–2 trial. Lancet Oncol 20(3):371–382. https://doi.org/10.1016/S1470-2045(18)30812-X
Duchnowska R, Peksa R, Radecka B, Mandat T, Trojanowski T, Jarosz B, Czartoryska-Arlukowicz B, Olszewski WP, Och W, Kalinka-Warzocha E, Kozlowski W, Kowalczyk A, Loi S, Biernat W, Jassem J, C Polish Brain Metastasis (2016) Immune response in breast cancer brain metastases and their microenvironment: the role of the PD-1/PD-L axis. Breast Cancer Res 18(1):43. https://doi.org/10.1186/s13058-016-0702-8
Deng L, Liang H, Burnette B, Beckett M, Darga T, Weichselbaum RR, Fu YX (2014) Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest 124(2):687–695. https://doi.org/10.1172/JCI67313
Dewan MZ, Galloway AE, Kawashima N, Dewyngaert JK, Babb JS, Formenti SC, Demaria S (2009) Fractionated but not single-dose radiotherapy induces an immune-mediated abscopal effect when combined with anti-CTLA-4 antibody. Clin Cancer Res 15(17):5379–5388. https://doi.org/10.1158/1078-0432.CCR-09-0265
Ahmed KA, Kim Y, Arrington JA, Kim S, DeJesus M, Soyano AE, Armaghani AJ, Costa RLB, Khong HT, Loftus LS, Rosa M, Caudell JJ, Diaz R, Robinson TJ, Etame AB, Tran ND, Sahebjam S, Soliman HH, Czerniecki BJ, Forsyth PA, Yu HM, Han HS (2021) Nivolumab and stereotactic radiosurgery for patients with breast cancer brain metastases: a nonrandomized, open-label phase 1b study. Adv Radiat Oncol 6(6):100798. https://doi.org/10.1016/j.adro.2021.100798
Yang TJ, Wijetunga NA, Yamada J, Wolden S, Mehallow M, Goldman DA, Zhang Z, Young RJ, Kris MG, Yu HA, Seidman AD, Gavrilovic IT, Lin A, Santomasso B, Grommes C, Piotrowski AF, Schaff L, Stone JB, DeAngelis LM, Boire A, Pentsova E (2021) Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro Oncol 23(1):134–143. https://doi.org/10.1093/neuonc/noaa152
Soffietti R, Cornu P, Delattre JY, Grant R, Graus F, Grisold W, Heimans J, Hildebrand J, Hoskin P, Kalljo M, Krauseneck P, Marosi C, Siegal T, Vecht C (2006) EFNS guidelines on diagnosis and treatment of brain metastases: report of an EFNS task force. Eur J Neurol 13(7):674–681. https://doi.org/10.1111/j.1468-1331.2006.01506.x
Feyer P, Sautter-Bihl ML, Budach W, Dunst J, Haase W, Harms W, Sedlmayer F, Souchon R, Wenz F, Sauer R (2010) DEGRO practical guidelines for palliative radiotherapy of breast cancer patients: brain metastases and leptomeningeal carcinomatosis. Strahlenther Onkol 186(2):63–69. https://doi.org/10.1007/s00066-010-2100-y
Kim JY, Kim ST, Nam DH, Lee JI, Park K, Kong DS (2011) Leukoencephalopathy and disseminated necrotizing leukoencephalopathy following intrathecal methotrexate chemotherapy and radiation therapy for central nerve system lymphoma or leukemia. J Korean Neurosurg Soc 50(4):304–310. https://doi.org/10.3340/jkns.2011.50.4.304
Pan Z, Yang G, He H, Zhao G, Yuan T, Li Y, Shi W, Gao P, Dong L, Li Y (2016) Concurrent radiotherapy and intrathecal methotrexate for treating leptomeningeal metastasis from solid tumors with adverse prognostic factors: a prospective and single-arm study. Int J Cancer 139(8):1864–1872. https://doi.org/10.1002/ijc.30214
Ahmed KA, Kim Y, DeJesus M, Kumthekar P, Williams NO, Palmer JD, Giglio P, Boire AA, Arrington J, Sahebjam S, Rosa M, Soliman HH, Yu H-HM, Han HS, Forsyth PAJ (2021) Trial in progress: phase I/II study of radiation therapy followed by intrathecal trastuzumab/pertuzumab in the management of HER2+ breast leptomeningeal disease. J Clin Oncol. https://doi.org/10.1200/JCO.2021.39.15_suppl.TPS1099
Wolf A, Donahue B, Silverman JS, Chachoua A, Lee JK, Kondziolka D (2017) Stereotactic radiosurgery for focal leptomeningeal disease in patients with brain metastases. J Neurooncol 134(1):139–143. https://doi.org/10.1007/s11060-017-2497-6
Onishi H, Morisaki T, Nakafusa Y, Nakashima Y, Yokohata K, Katano M (2011) Objective response with lapatinib in patients with meningitis carcinomatosa derived from HER2/HER1-negative breast cancer. Int J Clin Oncol 16(6):718–721. https://doi.org/10.1007/s10147-011-0195-5
Pellerino A, Palmiero R, Bruno F, Mo F, Muscolino E, Franchino F, Rudà R, Soffietti R (2021) P1442 Neratinib for treatment of leptomeningeal metastases from HER2-positive breast cancer in extended access program: preliminary results. Neuro Oncol 23(2):46. https://doi.org/10.1093/neuonc/noab180.159
Stringer-Reasor EM, O’Brien BJ, Topletz-Erickson A, White JB, Lobbous M, Riley K, Childress J, LaMaster K, Melisko ME, Morikawa A, Groot JFD, Krop IE, Valero V, Rimawi MF, Wolff AC, Tripathy D, Lin NU, Murthy RK (2021) Pharmacokinetic (PK) analyses in CSF and plasma from TBCRC049, an ongoing trial to assess the safety and efficacy of the combination of tucatinib, trastuzumab and capecitabine for the treatment of leptomeningeal metastasis (LM) in HER2 positive breast cancer. J Clin Oncol 39(15 suppl):1044–1044. https://doi.org/10.1200/JCO.2021.39.15_suppl.1044
Ricciardi GRR, Russo A, Franchina T, Schifano S, Mastroeni G, Santacaterina A, Adamo V (2018) Efficacy of T-DM1 for leptomeningeal and brain metastases in a HER2 positive metastatic breast cancer patient: new directions for systemic therapy: a case report and literature review. BMC Cancer 18(1):97. https://doi.org/10.1186/s12885-018-3994-5
Kumthekar P, Tang SC, Brenner AJ, Kesari S, Piccioni DE, Anders C, Carrillo J, Chalasani P, Kabos P, Puhalla S, Tkaczuk K, Garcia AA, Ahluwalia MS, Wefel JS, Lakhani N, Ibrahim N (2020) ANG1005, a brain-penetrating peptide-drug conjugate, shows activity in patients with breast cancer with leptomeningeal carcinomatosis and recurrent brain metastases. Clin Cancer Res 26(12):2789–2799. https://doi.org/10.1158/1078-0432.CCR-19-3258
Burch PA, Grossman SA, Reinhard CS (1988) Spinal cord penetration of intrathecally administered cytarabine and methotrexate: a quantitative autoradiographic study. J Natl Cancer Inst 80(15):1211–1216
Grossman SA, Finkelstein DM, Ruckdeschel JC, Trump DL, Moynihan T, Ettinger DS (1993) Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. Eastern Cooperative Oncology Group. J Clin Oncol 11(3):561–569. https://doi.org/10.1200/JCO.1993.11.3.561
Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, Maria B, LaFollette S, Schumann GB, Cole BF, Howell SB (1999) A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res 5(11):3394–3402
Hitchins RN, Bell DR, Woods RL, Levi JA (1987) A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J Clin Oncol 5(10):1655–1662. https://doi.org/10.1200/JCO.1987.5.10.1655
Boogerd W, van den Bent MJ, Koehler PJ, Heimans JJ, van der Sande JJ, Aaronson NK, Hart AA, Benraadt J, Vecht ChJ (2004) The relevance of intraventricular chemotherapy for leptomeningeal metastasis in breast cancer: a randomised study. Eur J Cancer 40(18):2726–2733. https://doi.org/10.1016/j.ejca.2004.08.012
Trump DL, Grossman SA, Thompson G, Murray K, Wharam M (1982) Treatment of neoplastic meningitis with intraventricular thiotepa and methotrexate. Cancer Treat Rep 66(7):1549–1551
Bhojwani D, Sabin ND, Pei D, Yang JJ, Khan RB, Panetta JC, Krull KR, Inaba H, Rubnitz JE, Metzger ML, Howard SC, Ribeiro RC, Cheng C, Reddick WE, Jeha S, Sandlund JT, Evans WE, Pui CH, Relling MV (2014) Methotrexate-induced neurotoxicity and leukoencephalopathy in childhood acute lymphoblastic leukemia. J Clin Oncol 32(9):949–959. https://doi.org/10.1200/JCO.2013.53.0808
Teh HS, Fadilah SA, Leong CF (2007) Transverse myelopathy following intrathecal administration of chemotherapy. Singapore Med J 48(2):e46-49
Siegal T, Lossos A, Pfeffer MR (1994) Leptomeningeal metastases: analysis of 31 patients with sustained off-therapy response following combined-modality therapy. Neurology 44(8):1463–1469
Boogerd W, Hart AA, van der Sande JJ, Engelsman E (1991) Meningeal carcinomatosis in breast cancer: prognostic factors and influence of treatment. Cancer 67(6):1685–1695
Zagouri F, Sergentanis TN, Bartsch R, Berghoff AS, Chrysikos D, de Azambuja E, Dimopoulos MA, Preusser M (2013) Intrathecal administration of trastuzumab for the treatment of meningeal carcinomatosis in HER2-positive metastatic breast cancer: a systematic review and pooled analysis. Breast Cancer Res Treat 139(1):13–22. https://doi.org/10.1007/s10549-013-2525-y
Figura NB, Rizk VT, Mohammadi H, Evernden B, Mokhtari S, Yu HM, Robinson TJ, Etame AB, Tran ND, Liu J, Washington I, Diaz R, Czerniecki BJ, Soliman H, Han HS, Sahebjam S, Forsyth PA, Ahmed KA (2019) Clinical outcomes of breast leptomeningeal disease treated with intrathecal trastuzumab, intrathecal chemotherapy, or whole brain radiation therapy. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-019-05170-7
Kumthekar P, Gradishar W, Lin N, Pentsova E, Groves M, Jeyapalan S, Melisko M, Grimm S, Lassman A, Raizer J (2018) CMET-22 intrathecal (IT) traztuzumab (T) for the treatment of leptomeningeal metastases (lm) in patients (PTS) with human epidermal growth factor receptor 2-positive (Her2+) cancer: a multicenter phase 1/2 study. Neuro Oncol 20(Suppl 6):58. https://doi.org/10.1093/neuonc/noy148.234
Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, Khushalani NI, Lewis K, Lao CD, Postow MA, Atkins MB, Ernstoff MS, Reardon DA, Puzanov I, Kudchadkar RR, Thomas RP, Tarhini A, Pavlick AC, Jiang J, Avila A, Demelo S, Margolin K (2018) Combined nivolumab and ipilimumab in melanoma metastatic to the brain. N Engl J Med 379(8):722–730. https://doi.org/10.1056/NEJMoa1805453
Schmid P, Cortes J, Pusztai L, McArthur H, Kümmel S, Bergh J, Denkert C, Park YH, Hui R, Harbeck N, Takahashi M, Foukakis T, Fasching PA, Cardoso F, Untch M, Jia L, Karantza V, Zhao J, Aktan G, Dent R, O’Shaughnessy J (2020) Pembrolizumab for early triple-negative breast cancer. N Engl J Med 382(9):810–821. https://doi.org/10.1056/NEJMoa1910549
Brastianos PK, Strickland MR, Lee EQ, Wang N, Cohen JV, Chukwueke U, Forst DA, Eichler A, Overmoyer B, Lin NU, Chen WY, Bardia A, Juric D, Dagogo-Jack I, White MD, Dietrich J, Nayyar N, Kim AE, Alvarez-Breckenridge C, Mahar M, Mora JL, Nahed BV, Jones PS, Shih HA, Gerstner ER, Giobbie-Hurder A, Carter SL, Oh K, Cahill DP, Sullivan RJ (2021) Phase II study of ipilimumab and nivolumab in leptomeningeal carcinomatosis. Nat Commun 12(1):5954. https://doi.org/10.1038/s41467-021-25859-y
Weller M, Stupp R, Wick W (2012) Epilepsy meets cancer: when, why, and what to do about it? Lancet Oncol 13(9):e375-382. https://doi.org/10.1016/S1470-2045(12)70266-8
Omuro AM, Lallana EC, Bilsky MH, DeAngelis LM (2005) Ventriculoperitoneal shunt in patients with leptomeningeal metastasis. Neurology 64(9):1625–1627. https://doi.org/10.1212/01.WNL.0000160396.69050.DC
Lin NU, Prowell T, Tan AR, Kozak M, Rosen O, Amiri-Kordestani L, White J, Sul J, Perkins L, Beal K, Gaynor R, Kim ES (2017) Modernizing clinical trial eligibility criteria: recommendations of the American society of clinical oncology-friends of cancer research brain metastases working group. J Clin Oncol 35(33):3760–3773. https://doi.org/10.1200/jco.2017.74.0761
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
KA, WK, and MM designed the study and prepared the manuscript. MM, WK, AS, YP, PF, BC, HS, HH, and KA assisted with data analysis, data interpretation, manuscript editing, and review.
Corresponding author
Ethics declarations
Conflict of interest
Peter A. Forsyth has received research funding from Pfizer and Celgene and is on the advisory boards of Novocure, BTG, Inovio, AbbVie, Ziopharm, Tocagen, and Pfizer. Hatem Soliman serves as a consultant for Astrazeneca, Celgene, Novartis, PUMA, and Eisai. Brian J Czerniecki has intellectual property on a HER2 dendritic cell vaccine. Hyo S. Han declares that she has received a speaker’s honorarium from Lilly Pharmaceuticals, research funding from Abbvie, Arvinas, GSK, Marker therapeutic, Novartis, Bristol-Myers Squibb, Pfizer, SeattleGenetics, Prescient, Horizon, Zymeworks and Karyopharm. Kamran A. Ahmed has received research funding from Bristol-Myers Squibb, Eli Lilly, and Genentech.
Ethical approval
This study was approved by the University of South Florida Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mills, M.N., King, W., Soyano, A. et al. Evolving management of HER2+ breast cancer brain metastases and leptomeningeal disease. J Neurooncol 157, 249–269 (2022). https://doi.org/10.1007/s11060-022-03977-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-03977-x