Abstract
Purpose/introduction
Craniopharyngiomas are locally-aggressive tumors arising along the hypothalamic-pituitary axis. Treatment is nuanced as a result of their proximity and adherence to vital neurovascular structures and responsiveness to surgery, radiation and, in some cases, chemotherapy.
Methods
We reviewed the literature discussing the current state of knowledge regarding craniopharyngioma biology and therapy.
Results
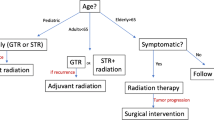
Recent advances in endoscopic endonasal surgery (EEA) have made surgery a safer and more effective option. While cure may be achieved with gross total resection (GTR), when felt to be too risky, a subtotal resection followed by radiation is often a more prudent strategy, particularly in children with hypothalamic invasion. Data on long-term outcome are mostly derived from older studies in which a craniotomy, rather than EEA, was performed. Long-term EEA outcome studies are lacking. Enhanced knowledge of the biological basis of papillary CPs has led to novel medical treatments for BRAFv600E variants that appear to be effective.
Conclusion
Endoscopic technology has improved surgical results for craniopharyngiomas and expanded the indications for the transsphenoidal approach. The goal of CP surgery goal is maximal safe resection to achieve cure, but subtotal resection and radiation may be equally effective. Early diagnosis of specific variants will facilitate enrollment in promising medical trials.



Similar content being viewed by others
Data availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- EOR:
-
Extent of resection
- CP:
-
Craniopharyngioma
- aCP:
-
Adamantinomatous craniopharyngioma
- pCP:
-
Papillary craniopharyngioma
- MRI:
-
Magnetic resonance imaging
- HPA:
-
Hypothalamic pituitary axis
- GTR:
-
Gross total resection
- STR:
-
Subtotal resection
- EEA:
-
Endonasal endoscopic approach
- TCA:
-
Transcranial approach
References
Pascual JM, Rosdolsky M, Prieto R, Strauβ S, Winter E, Ulrich W (2015) Jakob Erdheim (1874–1937): father of hypophyseal-duct tumors (craniopharyngiomas). Virchows Arch 467:459–469. https://doi.org/10.1007/s00428-015-1798-4
Prieto R, Rosdolsky M, Hofecker V, Barrios L, Pascual JM (2020) Craniopharyngioma treatment: an updated summary of important clinicopathological concepts. Expert Rev Endocrinol Metab 15:261–282. https://doi.org/10.1080/17446651.2020.1770081
Dandurand C, Sepehry AA, Asadi Lari MH, Akagami R, Gooderham P (2018) Adult craniopharyngioma: case series, systematic review, and meta-analysis. Neurosurgery 83:631–641. https://doi.org/10.1093/neuros/nyx570
Godil SS, Tosi U, Gerges MM, Garton A, Dobri GA, Kacker A, Tabaee A, Anand VK, Schwartz TH (2021) Long-term tumor control after endoscopic endonasal resection of craniopharyngiomas: comparison of gross-total resection versus subtotal resection with radiation therapy. Neurosurg Focus. https://doi.org/10.3171/2021.5.JNS202011
Sterkenburg AS, Hoffmann A, Gebhardt U, Warmuth-Metz M, Daubenbüchel AM, Müller HL (2015) Survival, hypothalamic obesity, and neuropsychological/psychosocial status after childhood-onset craniopharyngioma: newly reported long-term outcomes. Neuro Oncol 17:1029–1038. https://doi.org/10.1093/neuonc/nov044
Prieto R, Pascual JM, Rosdolsky M, Castro-Dufourny I, Carrasco R, Strauss S, Barrios L (2016) Craniopharyngioma adherence: a comprehensive topographical categorization and outcome-related risk stratification model based on the methodical examination of 500 tumors. Neurosurg Focus 41:E13. https://doi.org/10.3171/2016.9.Focus16304
Cavallo LM, Frank G, Cappabianca P, Solari D, Mazzatenta D, Villa A, Zoli M, D’Enza AI, Esposito F, Pasquini E (2014) The endoscopic endonasal approach for the management of craniopharyngiomas: a series of 103 patients. J Neurosurg 121:100–113. https://doi.org/10.3171/2014.3.Jns131521
Laws ER Jr (1980) Transsphenoidal microsurgery in the management of craniopharyngioma. J Neurosurg 52:661–666. https://doi.org/10.3171/jns.1980.52.5.0661
Zacharia BE, Bruce SS, Goldstein H, Malone HR, Neugut AI, Bruce JN (2012) Incidence, treatment and survival of patients with craniopharyngioma in the surveillance, epidemiology and end results program. Neuro Oncol 14:1070–1078. https://doi.org/10.1093/neuonc/nos142
Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM (1998) The descriptive epidemiology of craniopharyngioma. J Neurosurg 89:547–551. https://doi.org/10.3171/jns.1998.89.4.0547
Makino K, Nakamura H, Yano S, Kuratsu J (2010) Population-based epidemiological study of primary intracranial tumors in childhood. Child’s Nerv Syst 26:1029–1034. https://doi.org/10.1007/s00381-010-1126-x
Fan J, Liu Y, Pan J, Peng Y, Peng J, Bao Y, Nie J, Wang C, Qiu B, Qi S (2021) Endoscopic endonasal versus transcranial surgery for primary resection of craniopharyngiomas based on a new QST classification system: a comparative series of 315 patients. J Neurosurg. https://doi.org/10.3171/2020.7.Jns20257
La Corte E, Younus I, Pivari F, Selimi A, Ottenhausen M, Forbes JA, Pisapia DJ, Dobri GA, Anand VK, Schwartz TH (2018) BRAF V600E mutant papillary craniopharyngiomas: a single-institutional case series. Pituitary 21:571–583. https://doi.org/10.1007/s11102-018-0909-z
Yamada H, Haratake J, Narasaki T, Oda T (1995) Embryonal craniopharyngioma. Case report of the morphogenesis of a craniopharyngioma. Cancer 75:2971–2977
Green AL, Yeh JS, Dias PS (2002) Craniopharyngioma in a mother and daughter. Acta Neurochir 144:403–404. https://doi.org/10.1007/s007010200058
Martinez-Barbera JP (2015) Molecular and cellular pathogenesis of adamantinomatous craniopharyngioma. Neuropathol Appl Neurobiol 41:721–732. https://doi.org/10.1111/nan.12226
Sekine S, Takata T, Shibata T, Mori M, Morishita Y, Noguchi M, Uchida T, Kanai Y, Hirohashi S (2004) Expression of enamel proteins and LEF1 in adamantinomatous craniopharyngioma: evidence for its odontogenic epithelial differentiation. Histopathology 45:573–579. https://doi.org/10.1111/j.1365-2559.2004.02029.x
Prieto R, Pascual JM (2013) Craniopharyngiomas with a mixed histological pattern: the missing link to the intriguing pathogenesis of adamantinomatous and squamous-papillary varieties? Neuropathology 33:682–686. https://doi.org/10.1111/neup.12030
Burger P, Scheithauer B, Vogel F (2002) Surgical pathology of the nervous system and its coverings, 4th edn. Churchill Livingstone, Philadelphia
Müller HL, Merchant TE, Warmuth-Metz M, Martinez-Barbera JP, Puget S (2019) Craniopharyngioma. Nat Rev Dis Primers 5:75. https://doi.org/10.1038/s41572-019-0125-9
Grob S, Mirsky DM, Donson AM, Dahl N, Foreman NK, Hoffman LM, Hankinson TC, Mulcahy Levy JM (2019) Targeting IL-6 Is a potential treatment for primary cystic craniopharyngioma. Front Oncol 9:791. https://doi.org/10.3389/fonc.2019.00791
Gaston-Massuet C, Andoniadou CL, Signore M, Jayakody SA, Charolidi N, Kyeyune R, Vernay B, Jacques TS, Taketo MM, Le Tissier P, Dattani MT, Martinez-Barbera JP (2011) Increased wingless (Wnt) signaling in pituitary progenitor/stem cells gives rise to pituitary tumors in mice and humans. Proc Natl Acad Sci USA 108:11482–11487. https://doi.org/10.1073/pnas.1101553108
Gonzalez-Meljem JM, Martinez-Barbera JP (2021) Adamantinomatous craniopharyngioma as a model to understand paracrine and senescence-induced tumourigenesis. Cell Mol Life Sci 78:4521–4544. https://doi.org/10.1007/s00018-021-03798-7
Brastianos PK, Taylor-Weiner A, Manley PE, Jones RT, Dias-Santagata D, Thorner AR, Lawrence MS, Rodriguez FJ, Bernardo LA, Schubert L, Sunkavalli A, Shillingford N, Calicchio ML, Lidov HG, Taha H, Martinez-Lage M, Santi M, Storm PB, Lee JY, Palmer JN, Adappa ND, Scott RM, Dunn IF, Laws ER Jr, Stewart C, Ligon KL, Hoang MP, Van Hummelen P, Hahn WC, Louis DN, Resnick AC, Kieran MW, Getz G, Santagata S (2014) Exome sequencing identifies BRAF mutations in papillary craniopharyngiomas. Nat Genet 46:161–165. https://doi.org/10.1038/ng.2868
Haston S, Pozzi S, Carreno G, Manshaei S, Panousopoulos L, Gonzalez-Meljem JM, Apps JR, Virasami A, Thavaraj S, Gutteridge A, Forshew T, Marais R, Brandner S, Jacques TS, Andoniadou CL, Martinez-Barbera JP (2017) MAPK pathway control of stem cell proliferation and differentiation in the embryonic pituitary provides insights into the pathogenesis of papillary craniopharyngioma. Development 144:2141–2152. https://doi.org/10.1242/dev.150490
Alexandraki KI, Kaltsas GA, Karavitaki N, Grossman AB (2019) The medical therapy of craniopharyngiomas: the way ahead. J Clin Endocrinol Metab 104:5751–5764. https://doi.org/10.1210/jc.2019-01299
Brastianos PK, Twohy E, Geyer SM, Gerstner ER, Kaufmann TJ, Ruff M, Bota DA, Reardon DA, Cohen AL, Fuente MIDL, Lesser GJ, Campian JL, Agarwalla P, Kumthekar P, Cahill DP, Shih HA, Brown PD, Santagata S, Barker FG, Galanis E (2021) Alliance A071601: phase II trial of BRAF/MEK inhibition in newly diagnosed papillary craniopharyngiomas. J Clin Oncol 39:2000–2000. https://doi.org/10.1200/JCO.2021.39.15_suppl.2000
Huang ZS, Xiao X, Li XD, Mo HZ, He WL, Deng YH, Lu LJ, Wu YK, Liu H (2021) Machine learning-based multiparametric magnetic resonance imaging radiomic model for discrimination of pathological subtypes of craniopharyngioma. J Magn Reson Imaging. https://doi.org/10.1002/jmri.27761
Puget S, Garnett M, Wray A, Grill J, Habrand JL, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A, Sainte-Rose C (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106:3–12. https://doi.org/10.3171/ped.2007.106.1.3
Hoffman HJ (1994) Surgical management of craniopharyngioma. Pediatr Neurosurg 21(Suppl 1):44–49. https://doi.org/10.1159/000120861
Mrowczynski OD, Langan ST, Rizk EB (2018) Craniopharyngiomas: a systematic review and evaluation of the current intratumoral treatment landscape. Clin Neurol Neurosurg 166:124–130. https://doi.org/10.1016/j.clineuro.2018.01.039
Kilday JP, Caldarelli M, Massimi L, Chen RH, Lee YY, Liang ML, Parkes J, Naiker T, van Veelen ML, Michiels E, Mallucci C, Pettorini B, Meijer L, Dorfer C, Czech T, Diezi M, Schouten-van Meeteren AYN, Holm S, Gustavsson B, Benesch M, Müller HL, Hoffmann A, Rutkowski S, Flitsch J, Escherich G, Grotzer M, Spoudeas HA, Azquikina K, Capra M, Jiménez-Guerra R, MacDonald P, Johnston DL, Dvir R, Constantini S, Kuo MF, Yang SH, Bartels U (2017) Intracystic interferon-alpha in pediatric craniopharyngioma patients: an international multicenter assessment on behalf of SIOPE and ISPN. Neuro Oncol 19:1398–1407. https://doi.org/10.1093/neuonc/nox056
Guimarães MM, Cardeal DD, Teixeira MJ, Lucio J, Sanders FH, Kuromoto RK, Matushita H (2021) Brachytherapy in paediatric craniopharyngiomas: a systematic review and meta-analysis of recent literature. Child’s Nerv Syst. https://doi.org/10.1007/s00381-021-05378-3
Müller HL (2016) Craniopharyngioma and hypothalamic injury: latest insights into consequent eating disorders and obesity. Curr Opin Endocrinol Diabetes Obes 23:81–89. https://doi.org/10.1097/med.0000000000000214
Wijnen M, van den Heuvel-Eibrink MM, Janssen J, Catsman-Berrevoets CE, Michiels EMC, van Veelen-Vincent MC, Dallenga AHG, van den Berge JH, van Rij CM, van der Lely AJ, Neggers S (2017) Very long-term sequelae of craniopharyngioma. Eur J Endocrinol 176:755–767. https://doi.org/10.1530/eje-17-0044
Müller HL (2020) Management of hypothalamic obesity. Endocrinol Metab Clin N Am 49:533–552. https://doi.org/10.1016/j.ecl.2020.05.009
Wijnen M, Olsson DS, van den Heuvel-Eibrink MM, Wallenius V, Janssen JA, Delhanty PJ, van der Lely AJ, Johannsson G, Neggers SJ (2017) Efficacy and safety of bariatric surgery for craniopharyngioma-related hypothalamic obesity: a matched case-control study with 2 years of follow-up. Int J Obes 41:210–216. https://doi.org/10.1038/ijo.2016.195
Whelan R, Prince E, Mirsky DM, Naftel R, Bhatia A, Pettorini B, Avula S, Staulcup S, Alexander AL, Meier M, Hankinson TC (2019) Interrater reliability of a method to assess hypothalamic involvement in pediatric adamantinomatous craniopharyngioma. J Neurosurg Pediatr. https://doi.org/10.3171/2019.8.Peds19295
Elowe-Gruau E, Beltrand J, Brauner R, Pinto G, Samara-Boustani D, Thalassinos C, Busiah K, Laborde K, Boddaert N, Zerah M, Alapetite C, Grill J, Touraine P, Sainte-Rose C, Polak M, Puget S (2013) Childhood craniopharyngioma: hypothalamus-sparing surgery decreases the risk of obesity. J Clin Endocrinol Metab 98:2376–2382. https://doi.org/10.1210/jc.2012-3928
Stripp DC, Maity A, Janss AJ, Belasco JB, Tochner ZA, Goldwein JW, Moshang T, Rorke LB, Phillips PC, Sutton LN, Shu HK (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58:714–720. https://doi.org/10.1016/s0360-3016(03)01570-0
Schoenfeld A, Pekmezci M, Barnes MJ, Tihan T, Gupta N, Lamborn KR, Banerjee A, Mueller S, Chang S, Berger MS, Haas-Kogan D (2012) The superiority of conservative resection and adjuvant radiation for craniopharyngiomas. J Neurooncol 108:133–139. https://doi.org/10.1007/s11060-012-0806-7
Smith TR, Cote DJ, Jane JA Jr, Laws ER Jr (2016) Physiological growth hormone replacement and rate of recurrence of craniopharyngioma: the Genentech National Cooperative Growth Study. J Neurosurg Pediatr 18:408–412. https://doi.org/10.3171/2016.4.Peds16112
Cossu G, Jouanneau E, Cavallo LM, Elbabaa SK, Giammattei L, Starnoni D, Barges-Coll J, Cappabianca P, Benes V, Baskaya MK, Bruneau M, Meling T, Schaller K, Chacko AG, Youssef AS, Mazzatenta D, Ammirati M, Dufour H, Laws E, Berhouma M, Daniel RT, Messerer M (2020) Surgical management of craniopharyngiomas in adult patients: a systematic review and consensus statement on behalf of the EANS skull base section. Acta Neurochir 162:1159–1177. https://doi.org/10.1007/s00701-020-04265-1
Younus I, Forbes JA, Ordóñez-Rubiano EG, Avendano-Pradel R, La Corte E, Anand VK, Schwartz TH (2018) Radiation therapy rather than prior surgery reduces extent of resection during endonasal endoscopic reoperation for craniopharyngioma. Acta Neurochir 160:1425–1431. https://doi.org/10.1007/s00701-018-3567-z
Yang I, Sughrue ME, Rutkowski MJ, Kaur R, Ivan ME, Aranda D, Barani IJ, Parsa AT (2010) Craniopharyngioma: a comparison of tumor control with various treatment strategies. Neurosurg Focus 28:E5. https://doi.org/10.3171/2010.1.Focus09307
Ordóñez-Rubiano EG, Forbes JA, Morgenstern PF, Arko L, Dobri GA, Greenfield JP, Souweidane MM, Tsiouris AJ, Anand VK, Kacker A, Schwartz TH (2018) Preserve or sacrifice the stalk? Endocrinological outcomes, extent of resection, and recurrence rates following endoscopic endonasal resection of craniopharyngiomas. J Neurosurg. https://doi.org/10.3171/2018.6.Jns18901
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250. https://doi.org/10.3171/jns.1999.90.2.0237
Elliott RE, Jane JA Jr, Wisoff JH (2011) Surgical management of craniopharyngiomas in children: meta-analysis and comparison of transcranial and transsphenoidal approaches. Neurosurgery 69:630–643. https://doi.org/10.1227/NEU.0b013e31821a872d (discussion 643)
Moussazadeh N, Prabhu V, Bander ED, Cusic RC, Tsiouris AJ, Anand VK, Schwartz TH (2016) Endoscopic endonasal versus open transcranial resection of craniopharyngiomas: a case-matched single-institution analysis. Neurosurg Focus 41:E7. https://doi.org/10.3171/2016.9.Focus16299
Jeswani S, Nuño M, Wu A, Bonert V, Carmichael JD, Black KL, Chu R, King W, Mamelak AN (2016) Comparative analysis of outcomes following craniotomy and expanded endoscopic endonasal transsphenoidal resection of craniopharyngioma and related tumors: a single-institution study. J Neurosurg 124:627–638. https://doi.org/10.3171/2015.3.Jns142254
Prieto R, Pascual JM, Hofecker V, Winter E, Castro-Dufourny I, Carrasco R, Barrios L (2020) Craniopharyngioma adherence: a reappraisal of the evidence. Neurosurg Rev 43:453–472. https://doi.org/10.1007/s10143-018-1010-9
Hu W, Qiu B, Mei F, Mao J, Zhou L, Liu F, Fan J, Liu Y, Wen G, Qi S, Bao Y, Pan J (2021) Clinical impact of craniopharyngioma classification based on location origin: a multicenter retrospective study. Ann Transl Med 9:1164. https://doi.org/10.21037/atm-21-2924
Forbes JA, Ordóñez-Rubiano EG, Tomasiewicz HC, Banu MA, Younus I, Dobri GA, Phillips CD, Kacker A, Cisse B, Anand VK, Schwartz TH (2018) Endonasal endoscopic transsphenoidal resection of intrinsic third ventricular craniopharyngioma: surgical results. J Neurosurg. https://doi.org/10.3171/2018.5.Jns18198
Schwartz TH, Morgenstern PF, Anand VK (2019) Lessons learned in the evolution of endoscopic skull base surgery. J Neurosurg 130:337–346. https://doi.org/10.3171/2018.10.Jns182154
Almeida JP, Workewych A, Takami H, Velasquez C, Oswari S, Asha M, Bernardo A, Gentili F (2020) Surgical anatomy applied to the resection of craniopharyngiomas: anatomic compartments and surgical classifications. World Neurosurg 142:611–625. https://doi.org/10.1016/j.wneu.2020.05.171
Younus I, Gerges MM, Uribe-Cardenas R, Morgenstern PF, Eljalby M, Tabaee A, Greenfield JP, Kacker A, Anand VK, Schwartz TH (2020) How long is the tail end of the learning curve? Results from 1000 consecutive endoscopic endonasal skull base cases following the initial 200 cases. J Neurosurg 134:750–760. https://doi.org/10.3171/2019.12.Jns192600
Leng LZ, Greenfield JP, Souweidane MM, Anand VK, Schwartz TH (2012) Endoscopic, endonasal resection of craniopharyngiomas: analysis of outcome including extent of resection, cerebrospinal fluid leak, return to preoperative productivity, and body mass index. Neurosurgery 70:110–123. https://doi.org/10.1227/NEU.0b013e31822e8ffc (discussion 123-114)
Omay SB, Almeida JP, Chen YN, Shetty SR, Liang B, Ni S, Anand VK, Schwartz TH (2018) Is the chiasm-pituitary corridor size important for achieving gross-total resection during endonasal endoscopic resection of craniopharyngiomas? J Neurosurg 129:642–647. https://doi.org/10.3171/2017.6.Jns163188
Patel KS, Raza SM, McCoul ED, Patrona A, Greenfield JP, Souweidane MM, Anand VK, Schwartz TH (2015) Long-term quality of life after endonasal endoscopic resection of adult craniopharyngiomas. J Neurosurg 123:571–580. https://doi.org/10.3171/2014.12.Jns141591
Alalade AF, Ogando-Rivas E, Boatey J, Souweidane MM, Anand VK, Greenfield JP, Schwartz TH (2018) Suprasellar and recurrent pediatric craniopharyngiomas: expanding indications for the extended endoscopic transsphenoidal approach. J Neurosurg Pediatr 21:72–80. https://doi.org/10.3171/2017.7.Peds17295
Mazzatenta D, Zoli M, Guaraldi F, Ambrosi F, Faustini Fustini M, Pasquini E, Asioli S, Zucchelli M (2020) Outcome of endoscopic endonasal surgery in pediatric craniopharyngiomas. World Neurosurg 134:e277–e288. https://doi.org/10.1016/j.wneu.2019.10.039
Soldozy S, Yeghyayan M, Yağmurlu K, Norat P, Taylor DG, Kalani MYS, Jane JA, Syed HR (2020) Endoscopic endonasal surgery outcomes for pediatric craniopharyngioma: a systematic review. Neurosurg Focus 48:E6. https://doi.org/10.3171/2019.10.Focus19728
Gerges MM, Youngerman B, Anand VK, Greenfield JP, Schwartz TH (2020) Endoscopic endonasal resection of giant pediatric craniopharyngioma: impact on hypothalamic edema. Neurosurg Focus: Video FOCVID 2:V6. https://doi.org/10.3171/2020.4.FocusVid.19926
Wannemuehler TJ, Rubel KE, Hendricks BK, Ting JY, Payner TD, Shah MV, Cohen-Gadol AA (2016) Outcomes in transcranial microsurgery versus extended endoscopic endonasal approach for primary resection of adult craniopharyngiomas. Neurosurg Focus 41:E6. https://doi.org/10.3171/2016.9.Focus16314
Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH (2012) Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of craniopharyngiomas. World Neurosurg 77:329–341. https://doi.org/10.1016/j.wneu.2011.07.011
Veeravagu A, Lee M, Jiang B, Chang SD (2010) The role of radiosurgery in the treatment of craniopharyngiomas. Neurosurg Focus 28:E11. https://doi.org/10.3171/2010.2.Focus09311
Greenfield BJ, Okcu MF, Baxter PA, Chintagumpala M, Teh BS, Dauser RC, Su J, Desai SS, Paulino AC (2015) Long-term disease control and toxicity outcomes following surgery and intensity modulated radiation therapy (IMRT) in pediatric craniopharyngioma. Radiother Oncol 114:224–229. https://doi.org/10.1016/j.radonc.2014.11.035
Bishop AJ, Greenfield B, Mahajan A, Paulino AC, Okcu MF, Allen PK, Chintagumpala M, Kahalley LS, McAleer MF, McGovern SL, Whitehead WE, Grosshans DR (2014) Proton beam therapy versus conformal photon radiation therapy for childhood craniopharyngioma: multi-institutional analysis of outcomes, cyst dynamics, and toxicity. Int J Radiat Oncol Biol Phys 90:354–361. https://doi.org/10.1016/j.ijrobp.2014.05.051
Beltran C, Roca M, Merchant TE (2012) On the benefits and risks of proton therapy in pediatric craniopharyngioma. Int J Radiat Oncol Biol Phys 82:e281-287. https://doi.org/10.1016/j.ijrobp.2011.01.005
Ajithkumar T, Mazhari AL, Stickan-Verfürth M, Kramer PH, Fuentes CS, Lambert J, Thomas H, Müller H, Fleischhack G, Timmermann B (2018) Proton therapy for craniopharyngioma—an early report from a single European Centre. Clin Oncol (R Coll Radiol) 30:307–316. https://doi.org/10.1016/j.clon.2018.01.012
Lee CC, Yang HC, Chen CJ, Hung YC, Wu HM, Shiau CY, Guo WY, Pan DH, Chung WY, Liu KD (2014) Gamma Knife surgery for craniopharyngioma: report on a 20-year experience. J Neurosurg 121(Suppl):167–178. https://doi.org/10.3171/2014.8.Gks141411
Losa M, Pieri V, Bailo M, Gagliardi F, Barzaghi LR, Gioia L, Del Vecchio A, Bolognesi A, Mortini P (2018) Single fraction and multisession Gamma Knife radiosurgery for craniopharyngioma. Pituitary 21:499–506. https://doi.org/10.1007/s11102-018-0903-5
Minniti G, Esposito V, Amichetti M, Enrici RM (2009) The role of fractionated radiotherapy and radiosurgery in the management of patients with craniopharyngioma. Neurosurg Rev 32:125–132. https://doi.org/10.1007/s10143-009-0186-4 (discussion 132)
Kobayashi T, Tsugawa T, Hatano M, Hashizume C, Mori Y, Shibamoto Y (2015) Gamma knife radiosurgery of craniopharyngioma: results of 30 cases treated at Nagoya Radiosurgery Center. Nagoya J Med Sci 77:447–454
Tsugawa T, Kobayashi T, Hasegawa T, Iwai Y, Matsunaga S, Yamamoto M, Hayashi M, Kenai H, Kano T, Mori H, Nagano O, Hasegawa S, Inoue A, Nagatomo Y, Onoue S, Sato M, Yasuda S (2020) Gamma knife surgery for residual or recurrent craniopharyngioma after surgical resection: a multi-institutional retrospective study in Japan. Cureus 12:e6973. https://doi.org/10.7759/cureus.6973
Dho YS, Kim YH, Kim JW, Park CK, Chung HT, Kim SK, Paek SH, Wang KC, Kim DG (2018) Optimal strategy of gamma knife radiosurgery for craniopharyngiomas. J Neurooncol 140:135–143. https://doi.org/10.1007/s11060-018-2943-0
Ogino A, Niranjan A, Kano H, Flickinger JC, Lunsford LD (2021) Optimizing stereotactic radiosurgery in patients with recurrent or residual craniopharyngiomas. J Neurooncol 154:113–120. https://doi.org/10.1007/s11060-021-03806-7
Pikis S, Mantziaris G, Lavezzo K, Dabhi N, Sheehan J (2021) Stereotactic radiosurgery for craniopharyngiomas. Acta Neurochir 163:3201–3207. https://doi.org/10.1007/s00701-021-04990-1
Prieto R, Pascual JM, Subhi-Issa I, Jorquera M, Yus M, Martínez R (2013) Predictive factors for craniopharyngioma recurrence: a systematic review and illustrative case report of a rapid recurrence. World Neurosurg 79:733–749. https://doi.org/10.1016/j.wneu.2012.07.033
Dhandapani S, Singh H, Negm HM, Cohen S, Souweidane MM, Greenfield JP, Anand VK, Schwartz TH (2017) Endonasal endoscopic reoperation for residual or recurrent craniopharyngiomas. J Neurosurg 126:418–430. https://doi.org/10.3171/2016.1.Jns152238
Acknowledgements
The authors acknowledge the medical artist Matthew Holt.
Funding
There are no sources of funding to declare.
Author information
Authors and Affiliations
Contributions
FH and TS designed and conceived of this manuscript. FH performed the literature review and compiled the primary manuscript. FH and TS analyzed data. FH and TS compiled the figures and tables. All authors critically revised the manuscript and approved the manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript. Each author certifies that there are no financial arrangements (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that could pose a conflict of interest in connection with the submitted article.
Ethical approval
This review is waived from committee approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Henderson, F., Schwartz, T.H. Update on management of craniopharyngiomas. J Neurooncol 156, 97–108 (2022). https://doi.org/10.1007/s11060-021-03906-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03906-4