Abstract
Introduction
The outcome of awake surgery has been evaluated based on functional factors, return to work, and oncological aspects, and there have been no reports directly examining QOL. This study aimed to investigate the outcome of QOL following awake surgery and to determine the functional factors influencing QOL.
Methods
Seventy patients with WHO grade II/III gliomas were included. For the assessment of QOL, we used the SF-36 and calculated summary and sub-component scores. Three summary component scores, including physical (PCS), mental (MCS), and role/social summary (RCS) component scores, were computed based on sub-component scores. Additionally, various assessments of neurological/neuropsychological function were performed. We performed univariate and multiple regression analyses to investigate the functional factors influencing the SF-36.
Results
PCS and MCS were maintained, but only RCS was low to 42.0 ± 16.1. We then focused on the RCS and its sub-components: general health (GH), role physical (RP), social functioning (SF), and role emotional (RE). Multiple regression analysis showed following significant correlations between the sub-component scores and brain functions: GH to executive function and movement (p = 0.0033 and 0.032), RP to verbal fluency and movement (p = 0.0057 and 0.0010), and RE to verbal fluency (p = 0.020). Furthermore, when the sub-component scores were compared between groups with and without functional deficits related to GH, RP, and RE, each score was significantly lower in the groups with functional deficits (p = 0.012, 0.014, and 0.0049, respectively).
Conclusions
In patients who underwent awake surgery, a subset of patients had low QOL because of poor RCS. Functional factors influencing QOL included executive function, verbal fluency, and movement.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol 30:2559–2565. https://doi.org/10.1200/JCO.2011.38.4818
Hervey-Jumper SL, Berger MS (2016) Maximizing safe resection of low- and high-grade glioma. J Neuro-Oncol 130:269–282. https://doi.org/10.1007/s11060-016-2110-4
Nakajima R, Kinoshita M, Okita H, Yahata T, Nakada M (2019) Awake surgery for glioblastoma can preserve independence level, but is dependent on age and the preoperative condition. J Neuro-Oncol 144:155–163. https://doi.org/10.1007/s11060-019-03216-w
Kinoshita M, Nakajima R, Shinohara H, Miyashita K, Tanaka S, Okita H, Nakada M, Hayashi Y (2016) Chronic spatial working memory deficit associated with the superior longitudinal fasciculus: a study using voxel-based lesion-symptom mapping and intraoperative direct stimulation in right prefrontal glioma surgery. J Neurosurg 125:1024–1032. https://doi.org/10.3171/2015.10.JNS1591
Nakajima R, Kinoshita M, Okita H, Yahata T, Matsui M, Nakada M (2018) Neural networks mediating high-level mentalizing in patients with right cerebral hemispheric gliomas. Front Behav Neurosci 12:33. https://doi.org/10.3389/fnbeh.2018.00033
Thiebaut de Schotten M, Urbanski M, Duffau H, Volle E, Levy R, Dubois B, Bartolomeo P (2005) Direct evidence for a parietal-frontal pathway subserving spatial awareness in humans. Science 309:2226–2228. https://doi.org/10.1126/science.1116251
Wager M, Du Boisgueheneuc F, Pluchon C, Bouyer C, Stal V, Bataille B, Guillevin CM, Gil R (2013) Intraoperative monitoring of an aspect of executive functions: administration of the Stroop test in nine adult patients during awake surgery for resection of frontal glioma. Neurosurgery. https://doi.org/10.1227/NEU.0b013e31827bf1d6
Yordanova YN, Duffau H, Herbet G (2017) Neural pathways subserving face-based mentalizing. Brain Struct Funct 222:3087–3105. https://doi.org/10.1007/s00429-017-1388-0
Herbet G, Moritz-Gasser S, Duffau H (2016) Direct evidence for the contributive role of the right inferior fronto-occipital fasciculus in non-verbal semantic cognition. Brain Struct Funct 222:1597–1610. https://doi.org/10.1007/s00429-016-1294-x
Nakada M, Nakajima R, Okita H, Nakade Y, Yuno T, Tanaka S, Kinoshita M (2020) Awake surgery for right frontal lobe glioma can preserve visuospatial cognition and spatial working memory. J Neuro-Oncol. https://doi.org/10.1007/s11060-020-03656-9
Karimi M, Brazier J (2016) Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics 34:645–649. https://doi.org/10.1007/s40273-016-0389-9
Duffau H, Mandonnet E (2013) The “onco-functional balance” in surgery for diffuse low-grade glioma: integrating the extent of resection with quality of life. Acta Neurochir 155:951–957. https://doi.org/10.1007/s00701-013-1653-9
Jalali R, Dutta D (2012) Factors influencing quality of life in adult patients with primary brain tumors. Neuro-Oncol. https://doi.org/10.1093/neuonc/nos205
Henriksson R, Asklund T, Poulsen HS (2011) Impact of therapy on quality of life, neurocognitive function and their correlates in glioblastoma multiforme: a review. J Neuro-Oncol 104:639–646. https://doi.org/10.1007/s11060-011-0565-x
Bergner M, Bobbitt RA, Carter WB, Gilson BS (1981) The sickness impact profile: development and final revision of a health status measure. Med Care 19:787–805. https://doi.org/10.1097/00005650-198108000-00001
Williams AW, Ware JE, Donald CA (1981) A model of mental health, life events, and social supports applicable to general populations. J Health Soc Behav 22:324–336
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376. https://doi.org/10.1093/jnci/85.5.365
Ware JE Jr (1987) Standards for validating health measures: definition and content. J Chronic Dis 40:473–480. https://doi.org/10.1016/0021-9681(87)90003-8
Suzukamo Y, Fukuhara S, Green J, Kosinski M, Gandek B, Ware JE (2011) Validation testing of a three-component model of short form-36 scores. J Clin Epidemiol 64:301–308. https://doi.org/10.1016/j.jclinepi.2010.04.017
Bunevicius A (2017) Reliability and validity of the SF-36 health survey questionnaire in patients with brain tumors: a cross-sectional study. Health Qual Life Outcomes 15:92. https://doi.org/10.1186/s12955-017-0665-1
Boele FW, Douw L, de Groot M, van Thuijl HF, Cleijne W, Heimans JJ, Taphoorn MJ, Reijneveld JC, Klein M (2013) The effect of modafinil on fatigue, cognitive functioning, and mood in primary brain tumor patients: a multicenter randomized controlled trial. Neuro-Oncol 15:1420–1428. https://doi.org/10.1093/neuonc/not102
Fountain DM, Allen D, Joannides AJ, Nandi D, Santarius T, Chari A (2016) Reporting of patient-reported health-related quality of life in adults with diffuse low-grade glioma: a systematic review. Neuro-Oncol 18:1475–1486. https://doi.org/10.1093/neuonc/now107
Kim CW, Joo JD, Kim YH, Han JH, Kim CY (2016) Health-related quality of life in brain tumor patients treated with surgery: preliminary result of a single institution. Brain Tumor Res Treat 4:87–93. https://doi.org/10.14791/btrt.2016.4.2.87
Schiavolin S, Quintas R, Pagani M, Brock S, Acerbi F, Visintini S, Cusin A, Schiariti M, Broggi M, Ferroli P, Leonardi M (2014) Quality of life, disability, well-being, and coping strategies in patients undergoing neurosurgical procedures: preoperative results in an Italian sample. Sci World J 2014:790387. https://doi.org/10.1155/2014/790387
Daigle K, Fortin D, Mathieu D, Saint-Pierre AB, Pare FM, de la Sablonniere A, Goffaux P (2013) Effects of surgical resection on the evolution of quality of life in newly diagnosed patients with glioblastoma: a report on 19 patients surviving to follow-up. Curr Med Res Opin 29:1307–1313. https://doi.org/10.1185/03007995.2013.823858
Veilleux N, Goffaux P, Boudrias M, Mathieu D, Daigle K, Fortin D (2010) Quality of life in neurooncology–age matters. J Neurosurg 113:325–332. https://doi.org/10.3171/2010.2.JNS091707
Starnoni D, Berthiller J, Idriceanu TM, Meyronet D, d’Hombres A, Ducray F, Guyotat J (2018) Returning to work after multimodal treatment in glioblastoma patients. Neurosurg Focus 44:E17. https://doi.org/10.3171/2018.3.FOCUS1819
Ng S, Herbet G, Moritz-Gasser S, Duffau H (2020) Return to work following surgery for incidental diffuse low-grade glioma: a prospective series with 74 patients. Neurosurgery 87:720–729. https://doi.org/10.1093/neuros/nyz513
Muto J, Dezamis E, Rigaux-Viode O, Peeters S, Roux A, Zanello M, Mellerio C, Sauvageon X, Varlet P, Oppenheim C, Pallud J (2018) Functional-based resection does not worsen quality of life in patients with a diffuse low-grade glioma involving eloquent brain regions: a prospective cohort study. World Neurosurg 113:e200–e212. https://doi.org/10.1016/j.wneu.2018.01.213
Nickel K, Renovanz M, Konig J, Stockelmaier L, Hickmann AK, Nadji-Ohl M, Engelke J, Weimann E, Freudenstein D, Ganslandt O, Bullinger L, Wirtz CR, Coburger J (2018) The patients’ view: impact of the extent of resection, intraoperative imaging, and awake surgery on health-related quality of life in high-grade glioma patients-results of a multicenter cross-sectional study. Neurosurg Rev 41:207–219. https://doi.org/10.1007/s10143-017-0836-x
Wolf J, Campos B, Bruckner T, Vogt L, Unterberg A, Ahmadi R (2016) Evaluation of neuropsychological outcome and “quality of life” after glioma surgery. Langenbecks Arch Surg 401:541–549. https://doi.org/10.1007/s00423-016-1403-6
Tabor JK, Bonda D, LeMonda BC, D’Amico RS (2021) Neuropsychological outcomes following supratotal resection for high-grade glioma: a review. J Neuro-Oncol 152:429–437. https://doi.org/10.1007/s11060-021-03731-9
Kayama T (2012) The guidelines for awake craniotomy guidelines committee of the Japan awake surgery conference. Neurol Med Chir 52:119–141
Sawner KA, LaVigne JM (1970) Brunnstrom’s movement therapy in hemiplegia: a neurophysiological approach, 2nd edn. J. B. Lippincitt Company, New York, pp 41–65
Nakajima R, Kinoshita M, Okita H, Yahata T, Nakada M (2019) Glioma surgery under awake condition can lead to good independence and functional outcome excluding deep sensation and visuospatial cognition. Neuro-Oncol Pract 6:354–363. https://doi.org/10.1093/nop/npy054
Yoshida A, Motomura K, Natsume A, Chalise L, Iijima K, Hara D, Kadono I, Wakai K, Wakabayashi T (2020) Preoperative predictive factors affecting return to work in patients with gliomas undergoing awake brain mapping. J Neuro-Oncol 146:195–205. https://doi.org/10.1007/s11060-019-03371-0
Satoer D, Visch-Brink E, Dirven C, Vincent A (2016) Glioma surgery in eloquent areas: can we preserve cognition? Acta Neurochir 158:35–50. https://doi.org/10.1007/s00701-015-2601-7
Weyer-Jamora C, Brie MS, Luks TL, Smith EM, Hervey-Jumper SL, Taylor JW (2021) Postacute cognitive rehabilitation for adult brain tumor patients. Neurosurgery. https://doi.org/10.1093/neuros/nyaa552
Jakola AS, Unsgard G, Solheim O (2011) Quality of life in patients with intracranial gliomas: the impact of modern image-guided surgery. J Neurosurg 114:1622–1630. https://doi.org/10.3171/2011.1.JNS101657
Gabel N, Altshuler DB, Brezzell A, Briceno EM, Boileau NR, Miklja Z, Kluin K, Ferguson T, McMurray K, Wang L, Smith SR, Carlozzi NE, Hervey-Jumper SL (2019) Health related quality of life in adult low and high-grade glioma patients using the national institutes of health patient reported outcomes measurement information system (PROMIS) and neuro-QOL assessments. Front Neurol. https://doi.org/10.3389/fneur.2019.00212
Zhang SY, Qiu SW, Pan MR, Zhao MJ, Zhao RJ, Liu L, Li HM, Wang YF, Qian QJ (2021) Adult ADHD, executive function, depressive/anxiety symptoms, and quality of life: a serial two-mediator model. J Affect Disord 293:97–108. https://doi.org/10.1016/j.jad.2021.06.020
Wagner JL, Mueller M, Hellier TS, Smith G, Modi A (2021) ADHD and epilepsy-related QoL in youth with epilepsy. Epilepsy Behav 123:108250. https://doi.org/10.1016/j.yebeh.2021.108250
Puglisi G, Howells H, Sciortino T, Leonetti A, Rossi M, Conti Nibali M, Gabriel Gay L, Fornia L, Bellacicca A, Vigano L, Simone L, Catani M, Cerri G, Bello L (2019) Frontal pathways in cognitive control: direct evidence from intraoperative stimulation and diffusion tractography. Brain 142:2451–2465. https://doi.org/10.1093/brain/awz178
Kinoshita M, de Champfleur NM, Deverdun J, Moritz-Gasser S, Herbet G, Duffau H (2015) Role of fronto-striatal tract and frontal aslant tract in movement and speech: an axonal mapping study. Brain Struct Funct 220:3399–3412. https://doi.org/10.1007/s00429-014-0863-0
Kemerdere R, de Champfleur NM, Deverdun J, Cochereau J, Moritz-Gasser S, Herbet G, Duffau H (2016) Role of the left frontal aslant tract in stuttering: a brain stimulation and tractographic study. J Neurol 263:157–167. https://doi.org/10.1007/s00415-015-7949-3
Cochereau J, Lemaitre AL, Wager M, Moritz-Gasser S, Duffau H, Herbet G (2020) Network-behavior mapping of lasting executive impairments after low-grade glioma surgery. Brain Struct Funct 225:2415–2429. https://doi.org/10.1007/s00429-020-02131-5
Young JS, Morshed RA, Mansoori Z, Cha S, Berger MS (2020) Disruption of frontal aslant tract is not associated with long-term postoperative language deficits. World Neurosurg 133:192–195. https://doi.org/10.1016/j.wneu.2019.09.128
Saito T, Muragaki Y, Tamura M, Maruyama T, Nitta M, Tsuzuki S, Fukuchi S, Ohashi M, Kawamata T (2019) Awake craniotomy with transcortical motor evoked potential monitoring for resection of gliomas in the precentral gyrus: utility for predicting motor function. J Neurosurg. https://doi.org/10.3171/2018.11.JNS182609
Acknowledgements
None.
Funding
This work was supported by JSPS KAKENHI Grant Numbers JP 21H03301 and 21K19705.
Author information
Authors and Affiliations
Contributions
Conception and design: MN and RN Acquisition of data: RN. Analysis and interpretation of data: RN. Drafting article: MN, RN. Critically revising the article: All authors reviewed the final version of the manuscript and approved it for submission. Study supervision: MN.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
This study was performed in accordance with the guidelines of the Internal Review Board of Kanazawa University and was approved by the Medical Ethics Committee of Kanazawa University (Approval number 1731).
Consent to participate
Written informed consent to participate in this study was obtained from all the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
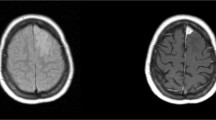
11060_2021_3904_MOESM2_ESM.tiff
Supplementary file2—Neurological and neuropsychological function at 6 months postoperatively for all patients are shown. Red, impaired; blue, un-impaired (TIFF 638 kb)
11060_2021_3904_MOESM3_ESM.tiff
Supplementary file3—Results of sub-component score of all participants are shown.Red line, mean; blue line, standard deviation (TIFF 1070 kb)
11060_2021_3904_MOESM5_ESM.tiff
Supplementary file5—There was no significant difference in KPS between patients who returned and did not return to work (A). Similarly, there was no significant difference in RCS between the "could not return to work" group and "return to work" group (B). In contrast, when KPS=100 was compared with KPS≤90, RCS was significantly higher in the former group (C). Red line, mean; blue line, standard deviation; **p<.01 (TIFF 1158 kb)
Rights and permissions
About this article
Cite this article
Nakajima, R., Kinoshita, M., Okita, H. et al. Quality of life following awake surgery depends on ability of executive function, verbal fluency, and movement. J Neurooncol 156, 173–183 (2022). https://doi.org/10.1007/s11060-021-03904-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03904-6