Abstract
Introduction
Glioma surgery near the functional area is still a dilemma. Intraoperative neurophysiologic monitoring (IONM) and functional mapping can play a role to maximize the extent of resection (EOR), while minimizing the risk of sequelae. We herein review the utility of tailored intraoperative mapping and monitoring in patients undergoing glioma surgery in our institute.
Methods
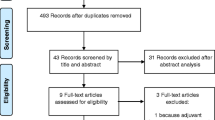
Patients were divided into two groups on the basis of application tailored IONM (group A, 2013–2017, n = 53) or not (group B, 2008–2012, n = 49) between January 2008 and December 2017. The setup, tailored IONM protocols, surgery, and clinical results of all patients with eloquent glioma were analyzed with the EOR, functionality scores, overall survival (OS) and progression-free survival (PFS) retrospectively.
Results
The 102 patients were considered eligible for analysis. High grade and low grade gliomas accounted for 73 (72%) and 29 (28%) cases, respectively. There was a positive association between the application of neuromonitor and post-operative functional preservation, but no significant statistical differences over the EOR, OS and PFS between the two groups.
Conclusions
In our experience, tailored intraoperative functional mapping provides an effective neurological function preservation. Routine implementation of neurophysiological monitoring with adequate pre-operative planning and intraoperative teamwork in eloquent glioma can get more satisfied functional preservation. Due to the maturation and experience of our IONM team may also be the variation factor, prospective studies with a more prominent sample and proper multivariate analysis will be expected to determine the real benefit.


Similar content being viewed by others
References
Sanai N et al (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115(1):3–8
Chaichana KL et al (2014) Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol 16(1):113–122
Pessina F et al (2017) Maximize surgical resection beyond contrast-enhancing boundaries in newly diagnosed glioblastoma multiforme: is it useful and safe? A single institution retrospective experience. J Neurooncol 135(1):129–139
Tamura M et al (2015) Strategy of surgical resection for glioma based on intraoperative functional mapping and monitoring. Neurol Med Chir (Tokyo) 55(5):383–398
Saito T et al (2018) Neurophysiological monitoring and awake craniotomy for resection of intracranial gliomas. Prog Neurol Surg 30:117–158
Bello L et al (2014) Tailoring neurophysiological strategies with clinical context enhances resection and safety and expands indications in gliomas involving motor pathways. Neuro Oncol 16(8):1110–1128
Schucht P et al (2017) A review of monopolar motor mapping and a comprehensive guide to continuous dynamic motor mapping for resection of motor eloquent brain tumors. Neurochirurgie 63(3):175–180
Szelenyi A et al (2011) Intra-operative subcortical electrical stimulation: a comparison of two methods. Clin Neurophysiol 122(7):1470–1475
Stummer W et al (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7(5):392–401
Coburger J et al (2015) Surgery for glioblastoma: impact of the combined use of 5-aminolevulinic acid and intraoperative MRI on extent of resection and survival. PLoS ONE 10(6):e0131872
Barbosa BJ et al (2016) Insular gliomas and the role of intraoperative assistive technologies: results from a volumetry-based retrospective cohort. Clin Neurol Neurosurg 149:104–110
Awad AW et al (2017) Impact of removed tumor volume and location on patient outcome in glioblastoma. J Neurooncol 135(1):161–171
Fukui A et al (2017) Volumetric analysis using low-field intraoperative magnetic resonance imaging for 168 newly diagnosed supratentorial glioblastomas: effects of extent of resection and residual tumor volume on survival and recurrence. World Neurosurg 98:73–80
Coburger J et al (2018) Counseling patients with a glioblastoma amenable only for subtotal resection: results of a multicenter retrospective assessment of survival and neurologic outcome. World Neurosurg 114:e1180–e1185
Sanai N, Berger MS (2008) Glioma extent of resection and its impact on patient outcome. Neurosurgery 62(4):753–764
Nitta M et al (2013) Updated therapeutic strategy for adult low-grade glioma stratified by resection and tumor subtype. Neurol Med Chir (Tokyo) 53(7):447–454
Duffau H (2015) Resecting diffuse low-grade gliomas to the boundaries of brain functions: a new concept in surgical neuro-oncology. J Neurosurg Sci 59(4):361–371
Ghinda D et al (2016) Contribution of combined intraoperative electrophysiological investigation with 3-T intraoperative MRI for awake cerebral glioma surgery: comprehensive review of the clinical implications and radiological outcomes. Neurosurg Focus 40(3):E14
Hervey-Jumper SL, Berger MS (2016) Maximizing safe resection of low- and high-grade glioma. J Neurooncol 130(2):269–282
Krivosheya D, Prabhu SS (2017) Combining functional studies with intraoperative MRI in glioma surgery. Neurosurg Clin N Am 28(4):487–497
Yordanova YN, Duffau H (2017) Supratotal resection of diffuse gliomas—an overview of its multifaceted implications. Neurochirurgie 63(3):243–249
Ojemann JG, Miller JW, Silbergeld DL (1996) Preserved function in brain invaded by tumor. Neurosurgery 39(2):253–258
Krivosheya D et al (2016) Technical principles in glioma surgery and preoperative considerations. J Neurooncol 130(2):243–252
Bertani G et al (2009) Intraoperative mapping and monitoring of brain functions for the resection of low-grade gliomas: technical considerations. Neurosurg Focus 27(4):E4
Goldring S (1978) A method for surgical management of focal epilepsy, especially as it relates to children. J Neurosurg 49(3):344–356
Krieg SM et al (2013) Reliability of intraoperative neurophysiological monitoring using motor evoked potentials during resection of metastases in motor-eloquent brain regions: clinical article. J Neurosurg 118(6):1269–1278
Okamoto E et al (2015) Variability in amplitude and stimulation threshold values in motor evoked potential (MEP) monitoring during the resection of brain lesions. Clin Neurophysiol 126(6):1271–1278
Plans G, et al (2017) Evaluation of the high-frequency monopolar stimulation technique for mapping and monitoring the corticospinal tract in patients with supratentorial gliomas. a proposal for intraoperative management based on neurophysiological data analysis in a series of 92 patients. Neurosurgery 81(4): 585–594
Huberfeld G et al (2017) Preoperative and intraoperative neurophysiological investigations for surgical resections in functional areas. Neurochirurgie 63(3):142–149
Duffau H et al (2005) Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: a comparative study between two series without (1985–96) and with (1996–2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry 76(6):845–851
De Witt Hamer PC et al (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol 30(20):2559–2565
Zhang N et al (2018) Long-term functional and oncologic outcomes of glioma surgery with and without intraoperative neurophysiologic monitoring: a retrospective cohort study in a single center. World Neurosurg 119:e94–e105
Gil-Robles S, Duffau H (2010) Surgical management of World Health Organization Grade II gliomas in eloquent areas: the necessity of preserving a margin around functional structures. Neurosurg Focus 28(2):E8
Pallud J, Dezamis E (2017) Functional and oncological outcomes following awake surgical resection using intraoperative cortico-subcortical functional mapping for supratentorial gliomas located in eloquent areas. Neurochirurgie 63(3):208–218
Chang EF et al (2011) Functional mapping-guided resection of low-grade gliomas in eloquent areas of the brain: improvement of long-term survival Clinical article. J Neurosurg 114(3):566–573
Acknowledgements
The authors express appreciation to Dr. Jui-Hu Hsiao for assistance in data processing, Ms. Tsu-Hui Wu for technical contribution in IONM data, Dr. MT Chiao and Dr. YJ Liang for the manuscript computer processing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. The Taiwan National Health Insurance Research Database contained unidentifiable secondary data. Information that might identify the individual patients was all encrypted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, SY., Chen, JP., Cheng, WY. et al. The role of tailored intraoperative neurophysiological monitoring in glioma surgery: a single institute experience. J Neurooncol 146, 459–467 (2020). https://doi.org/10.1007/s11060-019-03347-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03347-0