Abstract
Introduction
Cerebrovascular disease (CVD) and cancer are among the most common causes of mortality worldwide, preceded only by ischemic heart disease (IHD). Thrombocytopenia was shown to be associated with poor outcomes in IHD and CVD in the general population. This study aimed to assess the relationship of thrombocytopenia with poor outcomes in cancer patients with CVD.
Materials and methods
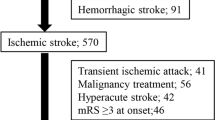
Data on patients with concomitant CVD and cancer who were initially treated at a cancer referral center between January 2010 and December 2017 were included. Thrombocytopenia was defined as a platelet count < 150,000/mm3 during the first 24 h of CVD symptom onset. The IRB (CI/837/17) approved the review of clinical records.
Results
Among 268 cancer patients with CVD included in the study, 210 met the inclusion criteria. Median overall survival of the entire cohort was 7.2 months, which was significantly shorter in males (p = 0.029) and patients with hematologic tumors (p = 0.009), hemorrhagic CVD (p < 0.001), altered mental status (p < 0.001), and thrombocytopenia (p < 0.001). Multiple regression logistic analysis revealed that thrombocytopenia (risk ratio [RR] 1.6, 95% confidence interval [CI] 1.1–2.4) and altered mental status (RR 2.7, 95% CI 1.9–4.0) remained statistically significant risk factors for mortality.
Conclusion
In cancer patients with CVD, thrombocytopenia at the time of CVD diagnosis and altered mental status during initial clinical evaluation were associated with higher mortality, which should be confirmed in future studies.

Similar content being viewed by others
References
Hankey GJ (2017) Stroke. The Lancet 389(10069):641–654. https://doi.org/10.1016/S0140-6736(16)30962-X
GBD 2015 Mortality and causes of death collaborators (2016) Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053):1459–1544. https://doi.org/10.1016/S0140-6736(16)31012-1
Sinkovic A, Majal M (2015) The impact of thrombocytopenia on outcome in patients with acute coronary syndromes: a single center retrospective study. Biomed Res Int. https://doi.org/10.1155/2015/907304
McClure MW, Berkowitz SD, Sparapani R et al (1999) Clinical significance of thrombocytopenia during a non-ST-elevation acute coronary syndrome. The platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrilin therapy (PURSUIT) trial experience. Circulation 99(22):2892–2900. https://doi.org/10.1161/01.CIR.99.22.2892
Caixeta A, Dangas G-D, Mehran R et al (2011) Incidence and clinical consequences of acquired thrombocytopenia after antithrombotic therapies in patients with acute coronary syndromes: results from the Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial. Am Heart J 161(2):298–306.e1. https://doi.org/10.1016/j.ahj.2010.10.035
Vora AN, Chenier M, Schulte PPJ et al (2014) Long-term outcomes associated with hospital acquired thrombocytopenia among patients with non-ST-segment elevation acute coronary syndrome. Am Heart J 168(2):189–196. https://doi.org/10.1016/j.ahj.2014.04.010
Ayoub Karab O, Gbolahan M, Meera et al (2018) Impact of baseline thrombocytopenia on in-hospital outcomes after percutaneous coronary interventions: analysis over 70,000 patients. JACC 71(11:10–12):A1164
Liu Shuai S, Chenxi Z, Yanyan et al (2018) The impact of acquired thrombocytopenia on long-term outcomes of patients undergoing elective percutaneous coronary intervention: an analysis of 8,271 consecutive patients. Catheter Cardiovasc Interv 91(1):558–565. https://doi.org/10.1002/ccd.27498
Furlan JC, Fang J, Silver FL (2016) Outcomes after acute ischemic stroke in patients with thrombocytopenia or thrombocytosis. J Neurol Sci 362:198–203. https://doi.org/10.1016/j.jns.2016.01.044
Mayda-Domac F, Mısırlı H, Yılmaz M (2010) Prognostic role of mean platelet volume and platelet count in ischemic and hemorrhagic stroke. J Stroke Cerebrovasc Dis 19(1):66–72. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.03.003
Riddle Matthew C et al (2018) American diabetes association: standards of medical care in diabetes. J Clin Appl Res Educ 41:13–27. https://doi.org/10.2337/dc18-SPPC01
James PA et al (2014) 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 5(5):507–520. https://doi.org/10.1001/jama.2013.284427.311
Posfai E, Marton I, Szoke A, Borbényi Z, Vecsei L, Csomor A et al (2014) Stroke in essential thrombocythemia. J Neurol Sci 336(1–2):260–262. https://doi.org/10.1016/j.jns.2013.10.016
Park HK, Lee SH (2014) Ischemic stroke associated with immune thrombocytopenia: lesion patterns and characteristics. Neurol Sci 35(11):1801–1806. https://doi.org/10.1007/s10072-014-1843-0
Sico JJ, Phipps MS, Concato J, Wells CK, Lo AC, Nadeau SE et al (2013) Thrombocytopenia and in-hospital mortality risk among ischemic stroke patients. J Stroke Cerebrovasc Dis 22(7):e99–e102. https://doi.org/10.1016/j.jstrokecerebrovasdis.2012.08.005
Schiffer CA, Bohlke K, Delaney M et al (2018) Platelet transfusion for patients with cancer: American Society of Clinical Oncology clinical practice guidelines update. J Clin Oncol 36:283–299. https://doi.org/10.1200/JCO.2017.76.1734
Zhang YY, Chan DKY, Cordato D (2006) Stroke risk factor, pattern and outcome in patients with cancer. Acta Neurol Scand 114(6):378–383. https://doi.org/10.1111/j.1600-0404.2006.00709.x
Cestari DM, Weine DM, Panageas KS (2004) Stroke in patients with cancer: incidence and etiology. Neurology 62(11):2025–2030. https://doi.org/10.1212/01.WNL.0000129912.56486.2B
Zhang YY, Cordato D, Shen Q et al (2007) Risk factor, pattern, etiology and outcome in ischemic stroke patients with cancer: a nested case-control study. Cerebrovasc Disease 23:181–187. https://doi.org/10.1159/000097639
Nguyen T, DeAngelis LM (2006) Stroke in cancer patients. Curr Neurol Neurosci Rep 6(3):187–192. https://doi.org/10.1007/s11910-006-0004-0
Bang OY, Seok JM, Kim SG et al (2011) Ischemic stroke and cancer: stroke severely impacts cancer patients, while cancer increases the number of strokes. J Clin Neurol 7(2):53–59. https://doi.org/10.3988/jcn.2011.7.2.53
Navi BB, Iadecola C (2018) Ischemic stroke in cancer patients: A review of an underappreciated pathology. Ann Neurol. https://doi.org/10.1002/ana.25227 (in press)
Kneihsl M, Enzinger C, Wünsch G et al (2016) Poor short-term outcome in patients with ischaemic stroke and active cancer. J Neurol 263(1):150–156. https://doi.org/10.1007/s00415-015-7954-6
Rodrigues M, Costa R, Brito S, Pissarra A, Lourenço A, Grenho F, Campos L (2016) Ischemic stroke and cancer correlation: a stroke unit experience. Ann Oncol 28(5):40
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional research and ethics committees.
Informed consent
Informed consent was not considered necessary by the institutional research and ethics committees for this was a retrospective observational study.
Rights and permissions
About this article
Cite this article
Cacho-Díaz, B., Spínola-Maroño, H., Mendoza-Olivas, L.G. et al. Platelet count is associated with outcome in cancer patients with stroke. J Neurooncol 140, 569–574 (2018). https://doi.org/10.1007/s11060-018-2982-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2982-6