Abstract
Purpose
Advances in the treatment of pediatric medulloblastoma have led to improved survival rates, though treatment-related toxicity leaves children with significant long-term deficits. There is significant variability in the cognitive outcome of medulloblastoma survivors, and it has been suggested that this variability may be attributable to genetic factors. The aim of this study was to explore the contributions of single nucleotide polymorphisms (SNPs) in two genes, peroxisome proliferator activated receptor (PPAR) and glutathione-S-transferase (GST), to changes in general intellectual functioning in medulloblastoma survivors.
Methods
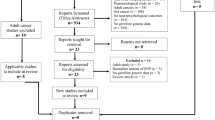
Patients (n = 44, meanage = 6.71 years, 61.3% males) were selected on the basis of available tissue samples and neurocognitive measures. Patients received surgical tumor resection, craniospinal radiation, radiation boost to the tumor site, and multiagent chemotherapy. Genotyping analyses were completed using the Illumina Human Omni2.5 BeadChip, and 41 single nucleotide polymorphisms (SNPs) were assessed across both genes. We used a machine learning algorithm to identify polymorphisms that were significantly associated with declines in general intellectual functioning following treatment for medulloblastoma.
Results
We identified age at diagnosis, radiation therapy, chemotherapy, and eight SNPs associated with PPARs as predictors of general intellectual functioning. Of the eight SNPs identified, PPARα (rs6008197), PPARγ (rs13306747), and PPARδ (rs3734254) were most significantly associated with long-term changes in general intellectual functioning in medulloblastoma survivors.
Conclusions
PPAR polymorphisms may predict intellectual outcome changes in children treated for medulloblastoma. Importantly, emerging evidence suggests that PPAR agonists may provide an opportunity to minimize the effects of treatment-related cognitive sequelae in these children.


Similar content being viewed by others
References
Packer RJ, Cogen P, Vezina G, Rorke LB (1999) Medulloblastoma: clinical and biologic aspects. Neuro Oncol 1:232–250. https://doi.org/10.1093/neuonc/1.3.232
Mulhern RK, Kepner JL, Thomas PR et al (1998) Neuropsychologic functioning of survivors of childhood medulloblastoma randomized to receive conventional or reduced-dose craniospinal irradiation: a Pediatric Oncology Group study. J Clin Oncol 16:1723–1728. https://doi.org/10.1200/JCO.1998.16.5.1723
Walter AW, Mulhern RK, Gajjar A et al (1999) Survival and neurodevelopmental outcome of young children with medulloblastoma at St Jude Children’s Research Hospital. J Clin Oncol 17:3720–3728. https://doi.org/10.1200/JCO.1999.17.12.3720
Palmer SL, Gajjar A, Reddick WE et al (2003) Predicting intellectual outcome among children treated with 35–40 Gy Craniospinal irradiation for medulloblastoma. Neuropsychology 17:548–555. https://doi.org/10.1037/0894-4105.17.4.548
Mabbott DJ (2006) Diffusion tensor imaging of white matter after cranial radiation in children for medulloblastoma: correlation with IQ. Neuro Oncol 8:244–252. https://doi.org/10.1215/15228517-2006-002
Moxon-Emre I, Bouffet E, Taylor MD et al (2014) Impact of craniospinal dose, boost volume, and neurologic complications on intellectual outcome in patients with medulloblastoma. J Clin Oncol 32:1760–1768. https://doi.org/10.1200/JCO.2013.52.3290
Barahmani N, Carpentieri S, Li XN et al (2009) Glutathione S-transferase M1 and T1 polymorphisms may predict adverse effects after therapy in children with medulloblastoma. Neuro Oncol 11:292–300. https://doi.org/10.1215/15228517-2008-089
Brackett J, Krull KR, Scheurer ME et al (2012) Antioxidant enzyme polymorphisms and neuropsychological outcomes in medulloblastoma survivors: a report from the Childhood Cancer Survivor Study. Neuro Oncol 14:1018–1025. https://doi.org/10.1093/neuonc/nos123
Wefel JS, Noll KR, Scheurer ME (2016) Neurocognitive functioning and genetic variation in patients with primary brain tumours. Lancet Oncol 17:e97–e108
Williams JG, Kubelik AR, Livak KJ et al (1990) DNA polymorphisms amplified by arbitrary primers are useful as genetic markers. Nucl Acids Res 18:6531–6535. https://doi.org/10.1093/nar/18.22.6531
Monje ML, Palmer T (2003) Radiation injury and neurogenesis. Curr Opin Neurol 16:129–134
Gao HM, Hong JS (2008) Why neurodegenerative diseases are progressive: uncontrolled inflammation drives disease progression. Trends Immunol 29:357–365. https://doi.org/10.1016/j.it.2008.05.002
Hayes JD, Pulford DJ (1995) The Glutathione-S-Transferase supergene family—regulation of Gst and the Contribution of the isoenzymes to cancer chemoprotection and drug-resistance. Crit Rev Biochem Mol Biol 30:445–600. https://doi.org/10.3109/10409239509083491
Berger J, Moller DE, Moller D et al (2002) The Mechanisms of action of PPARs. Annu Rev Med 53:409–435. https://doi.org/10.1146/annurev.med.53.082901.104018
Warden A, Truitt J, Merriman M et al (2016) Localization of PPAR isotypes in the adult mouse and human brain. Sci Rep 6:27618. https://doi.org/10.1038/srep27618
Kersten S, Desvergne B, Wahli W (2000) Roles of PPARS in health and disease. Nature 405:421–424. https://doi.org/10.1038/35013000
Ramanan S, Zhao W, Riddle DR, Robbins ME (2010) Review article: role of PPARs in radiation-induced brain injury. PPAR Research
Heneka MT, Sastre M, Dumitrescu-Ozimek L et al (2005) Acute treatment with the PPARγ agonist pioglitazone and ibuprofen reduces glial inflammation and Aβ1-42 levels in APPV717I transgenic mice. Brain 128:1442–1453. https://doi.org/10.1093/brain/awh452
Watson GS, Cholerton BA, Reger MA et al (2005) Preserved cognition in patients with early Alzheimer disease and amnestic mild cognitive impairment during treatment with rosiglitazone: a preliminary study. Am J Geriatr Psychiatry 13:950–958. https://doi.org/10.1176/appi.ajgp.13.11.950
Ramanan S, Kooshki M, Zhao W et al (2009) The PPARα agonist fenofibrate preserves hippocampal neurogenesis and inhibits microglial activation after whole-brain irradiation. Int J Radiat Oncol Biol Phys 75:870–877. https://doi.org/10.1016/j.ijrobp.2009.06.059
Zhao W, Payne V, Tommasi E et al (2007) Administration of the peroxisomal proliferator-activated receptor γ agonist pioglitazone during fractionated brain irradiation prevents radiation-induced cognitive impairment. Int J Radiat Oncol Biol Phys 67:6–9. https://doi.org/10.1016/j.ijrobp.2006.09.036
Daynes RA, Jones DC (2002) Emerging roles of PPARs in inflammation and immunity. Nat Rev Immunol 2:748–759
Ricote M, Glass CK (2007) PPARs and molecular mechanisms of transrepression. Biochim Biophys Acta 1771:926–935
McKinney BA, Reif DM, Ritchie MD, Moore JH (2006) Machine learning for detecting gene-gene interactions: a review. Appl Bioinform 5:77–88
Breiman L (2001) Random Forests. Mach Learn 45:5–32. https://doi.org/10.1023/A:1010933404324
Chen X, Ishwaran H (2012) Random forests for genomic data analysis. Genomics 99:323–329
Lunetta KL, Hayward LB, Segal J, van Eerdewegh P (2004) Screening large-scale association study data: exploiting interactions using random forests. BMC Genet. https://doi.org/10.1186/1471-2156-5-32
Wechsler D (2002) WPPSI-III administration and scoring manual. Psychol Corp. https://doi.org/10.1177/1073191102009001003
Wechsler D (2004) The Wechsler intelligence scale for children—fourth edition
Liu YR, Hu TM, Lan TH et al (2014) Association of the PPAR-γ gene with altered glucose levels and psychosis profile in schizophrenia patients exposed to antipsychotics. Psychiatry Investig 11:179–185. https://doi.org/10.4306/pi.2014.11.2.179
Glas J, Seiderer J, Markus C et al (2011) Role of PPARG gene variants in inflammatory bowel disease. Inflamm Bowel Dis 17:1057–1058
Combarros O, Rodríguez-Rodríguez E, Mateo I et al (2011) APOE dependent-association of PPAR-γ genetic variants with Alzheimer’s disease risk. Neurobiol Aging. https://doi.org/10.1016/j.neurobiolaging.2009.07.004
Wang H, Taverna D, Stram DO et al (2013) Genetic variation in the inflammation and innate immunity pathways and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev 22:2094–2101. https://doi.org/10.1158/1055-9965.EPI-13-0694
Costa M, Squassina A, Congiu D et al (2013) Investigation of endocannabinoid system genes suggests association between peroxisome proliferator activator receptor-α gene (PPARA) and schizophrenia. Eur Neuropsychopharmacol 23:749–759. https://doi.org/10.1016/j.euroneuro.2012.07.007
Zandi PP, Belmonte PL, Willour VL et al (2008) Association study of Wnt signaling pathway genes in bipolar disorder. Arch Gen Psychiatry 65:785–793. https://doi.org/10.1001/archpsyc.65.7.785
Johnson DC, Corthals SL, Walker B et al (2011) Genetic factors underlying the risk of thalidomide-related neuropathy in patients with multiple myeloma. J Clin Oncol 29:797–804. https://doi.org/10.1200/JCO.2010.28.0792
Holzapfel J, Heun R, Lütjohann D et al (2006) PPARD haplotype influences cholesterol metabolism but is no risk factor of Alzheimer’s disease. Neurosci Lett 408:57–61. https://doi.org/10.1016/j.neulet.2006.08.029
Rednam S, Scheurer ME, Adesina A et al (2013) Glutathione S-transferase P1 single nucleotide polymorphism predicts permanent ototoxicity in children with medulloblastoma. Pediatr Blood Cancer 60:593–598. https://doi.org/10.1002/pbc.24366
Harris SE, Fox H, Wright AF et al (2007) A genetic association analysis of cognitive ability and cognitive ageing using 325 markers for 109 genes associated with oxidative stress or cognition. BMC Genet 8:43. https://doi.org/10.1186/1471-2156-8-43
Pyper SR, Viswakarma N, Yu S, Reddy JK (2010) PPARα: energy combustion, hypolipidemia, inflammation and cancer. Nucl Recept Signal. https://doi.org/10.1621/nrs.08002
Altshuler DM, Durbin RM, Abecasis GR et al (2012) An integrated map of genetic variation from 1,092 human genomes. Nature 491:56–65. https://doi.org/10.1038/nature11632
Price AL, Patterson NJ, Plenge RM et al (2006) Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 38:904–909. https://doi.org/10.1038/ng1847
Ishwaran H, Kogalur UB, Blackstone EH, Lauer MS (2008) Random survival forests. Ann Appl Stat 2:841–860. https://doi.org/10.1214/08-AOAS169
Aleshin S, Strokin M, Sergeeva M, Reiser G (2013) Peroxisome proliferator-activated receptor (PPAR)beta/delta, a possible nexus of PPARalpha- and PPARgamma-dependent molecular pathways in neurodegenerative diseases: Review and novel hypotheses. Neurochem Int 63:322–330
Aleshin S, Reiser G (2013) Role of the peroxisome proliferator-activated receptors (PPAR)-α, β/δ and γ triad in regulation of reactive oxygen species signaling in brain. Biol Chem 394:1553–1570
Cole PD, Finkelstein Y, Stevenson KE et al (2015) Polymorphisms in genes related to oxidative stress are associated with inferior cognitive function after therapy for childhood acute lymphoblastic leukemia. J Clin Oncol 33:2205–2211. https://doi.org/10.1200/JCO.2014.59.0273
Acknowledgements
Funding for this work was provided by the Garron Family Cancer Center Small Grant Competition at The Hospital for Sick Children in Toronto. We thank Dr. Chao Lu for help with DNA microarray analysis, and Aziz Mezlini for help with our statistical approach.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2018_3083_MOESM1_ESM.tif
Supplementary material 1 Supplementary fig 1. Density plot of VIMP scores for variables with scores less than or equal to zero across all iterations of the prediction RFR model. Due to space considerations axes labels have been omitted. The dashed red line indicates a vimp score of zero. Values to the left of the dashed line indicate negative vimp scores. Supplementary fig 2. Boxplots showing the relationships between intellectual outcome and age at diagnosis, radiation therapy, and chemotherapy. Intellectual outcome was determined as the predicted change in FSIQ scores over time based on RFR model estimates. Older age at diagnosis predicted better intellectual outcome, while reduced craniospinal radiation with a tumor bed boost, as well as the SJMB03 chemotherapy protocol predicted better intellectual outcome. Radiation therapy: S-PF – Standard dose + posterior fossa boost, S-TB – Standard dose + tumor bed boost, R-PF – Reduced dose + posterior fossa boost, R-TB – Reduced dose + tumor bed boost. Chemotherapy protocols: CCCG 9961 (Vincristine, Lomustine, Cisplatin); POG 9631 (Etoposide, Cisplatin, Cyclophosphamide, Vincristine); SJMB03 (Vincristine, Cisplatin, Cyclophosphamide, Amifostine); 99703 (Vincristine, Cisplatin, Cyclophosphamide, Etoposide); ACNS 0331 (Lomustine, Cisplatin, Vincristine, Cyclophosphamide) (TIF 244 KB)
Rights and permissions
About this article
Cite this article
Oyefiade, A., Erdman, L., Goldenberg, A. et al. PPAR and GST polymorphisms may predict changes in intellectual functioning in medulloblastoma survivors. J Neurooncol 142, 39–48 (2019). https://doi.org/10.1007/s11060-018-03083-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-03083-x