Abstract
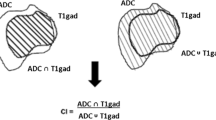
Radiation necrosis is a serious potential adverse event of stereotactic radiosurgery that cannot be reliably differentiated from recurrent tumor using conventional imaging techniques. Intravoxel incoherent motion (IVIM) is a magnetic resonance imaging (MRI) based method that uses a diffusion-weighted sequence to estimate quantitative perfusion and diffusion parameters. This study evaluated the IVIM-derived apparent diffusion coefficient (ADC) and perfusion fraction (f), and compared the results to the gold standard histopathological-defined outcomes of radiation necrosis or recurrent tumor. Nine patients with ten lesions were included in this study; all lesions exhibited radiographic progression after stereotactic radiosurgery for brain metastases that subsequently underwent surgical resection due to uncertainty regarding the presence of radiation necrosis versus recurrent tumor. Pre-surgical IVIM was performed to obtain f and ADC values and the results were compared to histopathology. Five lesions exhibited pathological radiation necrosis and five had predominantly recurrent tumor. The IVIM perfusion fraction reliably differentiated tumor recurrence from radiation necrosis (fmean = 10.1 ± 0.7 vs. 8.3 ± 1.2, p = 0.02; cutoff value of 9.0 yielding a sensitivity/specificity of 100%/80%) while the ADC did not distinguish between the two (ADCmean = 1.1 ± 0.2 vs. 1.2 ± 0.4, p = 0.6). IVIM shows promise in differentiating recurrent tumor from radiation necrosis for brain metastases treated with radiosurgery, but needs to be validated in a larger cohort.




Similar content being viewed by others
References
Linskey ME, Andrews DW, Asher AL, Burri SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Kalkanis SN (2010) The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96:45–68. doi:10.1007/s11060-009-0073-4
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. doi:10.1016/S1470-2045(09)70263-3
Soliman H, Das S, Larson DA, Sahgal A (2016) Stereotactic radiosurgery (SRS) in the modern management of patients with brain metastases. Oncotarget. doi:10.18632/oncotarget.7131
Chao ST, Ahluwalia MS, Barnett GH, Stevens GHJ, Murphy ES, Stockham AL, Shiue K, Suh JH (2013) Challenges with the diagnosis and treatment of cerebral radiation necrosis. Int J Radiat Oncol Biol Phys 87:449–457. doi:10.1016/j.ijrobp.2013.05.015
Le Rhun E, Dhermain F, Vogin G, Reyns N, Metellus P (2016) Radionecrosis after stereotactic radiotherapy for brain metastases. Expert Rev Neurother 16:1–12. doi:10.1080/14737175.2016.1184572
Parvez K, Parvez A, Zadeh G (2014) The diagnosis and treatment of pseudoprogression, radiation necrosis and brain tumor recurrence. Int J Mol Sci 15:11832–11846. doi:10.3390/ijms150711832
Kohutek ZA, Yamada Y, Chan TA, Brennan CW, Tabar V, Gutin PH, Jonathan Yang T, Rosenblum MK, Ballangrud A, Young RJ, Zhang Z, Beal K (2015) Long-term risk of radionecrosis and imaging changes after stereotactic radiosurgery for brain metastases. J Neurooncol 125:149–156. doi:10.1007/s11060-015-1881-3
Truong MT, St Clair EG, Donahue BR, Rush SC, Miller DC, Formenti SC, Knopp EA, Han K, Golfinos JG (2006) Results of surgical resection for progression of brain metastases previously treated by gamma knife radiosurgery. Neurosurgery 59:86–97. doi:10.1227/01.NEU.0000219858.80351.38
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele N, Grewal J, Prabhu S, Loghin M, Gilbert MR, Jackson EF (2012) Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys 79:1487–1495. doi:10.1016/j.ijrobp.2009.12.061.Randomized
Dequesada IM, Quisling RG, Yachnis A, Friedman WA (2008) Can standard magnetic resonance imaging reliably distinguish recurrent tumor from radiation necrosis after radiosurgery for brain metastases? A radiographic-pathological study. Neurosurgery 63:898–903. doi:10.1227/01.NEU.0000333263.31870.31
Hein PA, Eskey CJ, Dunn JF, Hug EB (2004) Diffusion-weighted imaging in the follow-up of treated high-grade gliomas: tumor recurrence versus radiation injury. Am J Neuroradiol 25:201–209
Bisdas S, Naegele T, Ritz R, Dimostheni A, Pfannenberg C, Reimold M, Koh TS, Ernemann U (2011) Distinguishing recurrent high-grade gliomas from radiation injury. A pilot study using dynamic contrast-enhanced MR imaging. Acad Radiol 18:575–583. doi:10.1016/j.acra.2011.01.018
Barajas RF, Chang JS, Sneed PK, Segal MR, McDermott MW, Cha S (2009) Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility—weighted contrast-enhanced perfusion MR imaging. Am J Neuroradiol 30:367–372. doi:10.3174/ajnr.A1362
Schlemmer HP, Bachert P, Henze M, Buslei R, Herfarth KK, Debus J, van Kaick G (2002) Differentiation of radiation necrosis from tumor progression using proton magnetic resonance spectroscopy. Neuroradiology 44:216–222. doi:10.1007/s002340100703
Tie J, Gunawardana DH, Rosenthal MA (2008) Differentiation of tumor recurrence from radiation necrosis in high-grade gliomas using 201Tl-SPECT. J Clin Neurosci 15:1327–1334. doi:10.1016/j.jocn.2007.12.008
Di Chiro G, Oldfield E, Wright DC, Demichele D, Katz DA, Patronas NJ, Doppman JL, Larson SM, Ito M, Kufta CV (1988) Cerebral necrosis after radiotherapy and or intraarterial chemotherapy for brain-tumors—pet and neuropathologic studies. Am J Roentgenol 150:189–197. doi:10.2214/ajr.150.1.189
Terakawa Y, Tsuyuguchi N, Iwai Y, Yamanaka K, Higashiyama S, Takami T, Ohata K (2008) Diagnostic accuracy of 11 C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy. J Nucl Med 49:694–699. doi:10.2967/jnumed.107.048082
Telera S, Fabi A, Pace A, Vidiri A, Anelli V, Carapella CM, Marucci L, Crispo F, Sperduti I, Pompili A (2013) Radionecrosis induced by stereotactic radiosurgery of brain metastases: results of surgery and outcome of disease. J Neurooncol 113:313–325. doi:10.1007/s11060-013-1120-8
Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401–407. doi:10.1148/radiology.161.2.3763909
Kim DY, Kim HS, Goh MJ, Choi CG, Kim SJ (2014) Utility of intravoxel incoherent motion MR imaging for distinguishing recurrent metastatic tumor from treatment effect following gamma knife radiosurgery: initial experience. Am J Neuroradiol 35:2082–2090. doi:10.3174/ajnr.A3995
Federau C, O’Brien K, Meuli R, Hagmann P, Maeder P (2014) Measuring brain perfusion with intravoxel incoherent motion (IVIM): initial clinical experience. J Magn Reson Imaging 39:624–632. doi:10.1002/jmri.24195
Turner R, Le Bihan D, Maier J, Vavrek R, Hedges LK, Pekar J (1990) Echo-planar imaging of intravoxel incoherent motion. Radiology 177:407–414. doi:10.1148/radiology.177.2.2217777
Le Bihan D (1988) Intravoxel incoherent motion imaging using steady-state free precession. Magn Reson Med 7:346–351
Conklin J, Heyn C, Roux M, Cerny M, Wintermark M, Federau C (2016) A simplified model for intravoxel incoherent motion perfusion imaging of the brain. Am J Neuroradiol 37:2251–2257. doi:10.3174/ajnr.A4929
Kim HS, Suh CH, Kim N, Choi CG, Kim SJ (2014) Histogram analysis of intravoxel incoherent motion for differentiating recurrent tumor from treatment effect in patients with glioblastoma: initial clinical experience. Am J Neuroradiol 35:490–497. doi:10.3174/ajnr.A3719
Szeifert GT, Atteberry DS, Kondziolka D, Levivier M, Lunsford LD (2006) Cerebral metastases pathology after radiosurgery: a multicenter study. Cancer 106:2672–2681. doi:10.1002/cncr.21946
Tihan T, Barletta J, Parney I, Lamborn K, Sneed PK, Chang S (2006) Prognostic value of detecting recurrent glioblastoma multiforme in surgical specimens from patients after radiotherapy: should pathology evaluation alter treatment decisions? Hum Pathol 37:272–282
Williams BJ, Suki D, Fox BD, Pelloski CE, Maldaun MVC, Sawaya RE, Lang FF, Rao G (2009) Stereotactic radiosurgery for metastatic brain tumors: a comprehensive review of complications. J Neurosurg 111:439–448. doi:10.3171/2008.11.JNS08984
Jagannathan J, Bourne TD, Schlesinger D, Yen C-P, Shaffrey ME, Laws ER, Sheehan JP (2010) Clinical and pathological characteristics of brain metastasis resected after failed radiosurgery. Neurosurgery 66:208–217. doi:10.1227/01.NEU.0000359318.90478.69
Vecil GG, Suki D, Maldaun MVC, Lang FF, Sawaya R (2005) Resection of brain metastases previously treated with stereotactic radiosurgery. J Neurosurg 102:209–215. doi:10.3171/jns.2005.102.2.0209
Alomari A, Rauch PJ, Orsaria M, Minja FJ, Chiang VL, Vortmeyer AO (2014) Radiologic and histologic consequences of radiosurgery for brain tumors. J Neurooncol 117:33–42. doi:10.1007/s11060-014-1359-8
Provenzale JM, Mukundan S, Barboriak DP (2006) Diffusion-weighted and perfusion MR imaging for brain tumor characterization and assessment of treatment response. Radiology 239:632–649. doi:10.1148/radiol.2393042031
Al Sayyari A, Buckley R, McHenery C, Pannek K, Coulthard A, Rose S (2010) Distinguishing recurrent primary brain tumor from radiation injury: a preliminary study using a susceptibility-weighted MR imaging-guided apparent diffusion coefficient analysis strategy. Am J Neuroradiol 31:1049–1054. doi:10.3174/ajnr.A2011
Federau C, Meuli R, O’Brien K, Maeder P, Hagmann P (2014) Perfusion measurement in brain gliomas with intravoxel incoherent motion MRI. Am J Neuroradiol 35:256–262. doi:10.3174/ajnr.A3686
Bisdas S, Braun C, Skardelly M, Schittenhelm J, Teo TH, Thng CH, Klose U, Koh TS (2014) Correlative assessment of tumor microcirculation using contrast-enhanced perfusion MRI and intravoxel incoherent motion diffusion-weighted MRI: is there a link between them? NMR Biomed 27:1184–1191. doi:10.1002/nbm.3172
Lee HJ, Rha SY, Chung YE, Shim HS, Kim YJ, Hur J, Hong YJ, Choi BW (2014) Tumor perfusion-related parameter of diffusion-weighted magnetic resonance imaging: correlation with histological microvessel density. Magn Reson Med 71:1554–1558. doi:10.1002/mrm.24810
Iima M, Reynaud O, Tsurugizawa T, Ciobanu L, Li JR, Geffroy F, Djemai B, Umehana M, Le Bihan D (2014) Characterization of glioma microcirculation and tissue features using intravoxel incoherent motion magnetic resonance imaging in a rat brain model. Investig Radiol 49:485–490. doi:10.1097/RLI.0000000000000040
Wirestam R, Borg M, Brockstedt S, Lindgren A, Holtas S, Stahlberg F (2001) Perfusion-related parameters in intravoxel incoherent motion MR imaging compared with CBV and CBF measured by dynamic susceptibility-contrast MR technique. Acta Radiol 42:123–128
Pekar J, Moonen CT, van Zijl PC (1992) On the precision of diffusion/perfusion imaging by gradient sensitization. Magn Reson Med 23:122–129
Ellingson BM, Bendszus M, Boxerman J, Barboriak D, Erickson BJ, Smits M, Nelson SJ, Gerstner E, Alexander B, Goldmacher G, Wick W, Vogelbaum M, Weller M, Galanis E, Kalpathy-Cramer J, Shankar L, Jacobs P, Pope WB, Yang D, Chung C, Knopp MV, Cha S, van den Bent MJ, Chang S, Yung WK, Cloughesy TF, Wen PY, Gilbert MR (2015) Consensus recommendations for a standardized brain tumor imaging protocol in clinical trials. Neuro Oncol 17:1188–1198. doi:10.1093/neuonc/nov095
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Detsky, J.S., Keith, J., Conklin, J. et al. Differentiating radiation necrosis from tumor progression in brain metastases treated with stereotactic radiotherapy: utility of intravoxel incoherent motion perfusion MRI and correlation with histopathology. J Neurooncol 134, 433–441 (2017). https://doi.org/10.1007/s11060-017-2545-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2545-2