Abstract
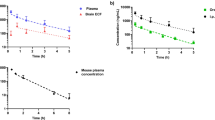
The blood–brain barrier (BBB) significantly reduces the delivery of many systemically administered agents to the central nervous system. Although temozolomide is the only chemotherapy to improve survival in patients with glioblastoma, its concentration in brain is only 20 % of that in blood. Regadenoson, an FDA approved adenosine receptor agonist used for cardiac stress testing, transiently disrupts rodent BBB allowing high molecular weight dextran (70 kD) to enter the brain. This study was conducted to determine if regadenoson could facilitate entry of temozolomide into normal rodent brain. Temozolomide (50 mg/kg) was administered by oral gavage to non-tumor bearing F344 rats. Two-thirds of the animals received a single dose of intravenous regadenoson 60–90 min later. All animals were sacrificed 120 or 360 min after temozolomide administration. Brain and plasma temozolomide concentrations were determined using HPLC/MS/MS. Brain temozolomide concentrations were significantly higher at 120 min when it was given with regadenoson versus alone (8.1 ± 2.7 and 5.1 ± 3.5 µg/g, P < 0.05). A similar trend was noted in brain:plasma ratios (0.45 ± 0.08 and 0.29 ± 0.09, P < 0.05). Brain concentrations and brain:plasma ratios were not significantly different 360 min after temozolomide administration. No differences were seen in plasma temozolomide concentrations with or without regadenoson. These results suggest co-administration of regadenoson with temozolomide results in 60 % higher temozolomide levels in normal brain without affecting plasma concentrations. This novel approach to increasing intracranial concentrations of systemically administered agents has potential to improve the efficacy of chemotherapy in neuro-oncologic disorders.

Similar content being viewed by others
References
Neuwelt EA (2004) Mechanisms of disease: the blood–brain barrier. Neurosurgery 54:131–140 (Discussion 141–142)
Pardridge WM (2015) Blood–brain barrier drug delivery of IgG fusion proteins with a transferrin receptor monoclonal antibody. Expert Opin Drug Deliv 12:207–222. doi:10.1517/17425247.2014.952627
Kroll RA, Neuwelt EA (1998) Outwitting the blood–brain barrier for therapeutic purposes: osmotic opening and other means. Neurosurgery 42:1083–1099 (Discussion 1099–1100)
Attenello FJ, Mukherjee D, Datoo G, McGirt MJ, Bohan E, Weingart JD, Olivi A, Quinones-Hinojosa A, Brem H (2008) Use of Gliadel (BCNU) wafer in the surgical treatment of malignant glioma: a 10-year institutional experience. Ann Surg Oncol 15:2887–2893. doi:10.1245/s10434-008-0048-2
White E, Bienemann A, Pugh J, Castrique E, Wyatt M, Taylor H, Cox A, McLeod C, Gill S (2012) An evaluation of the safety and feasibility of convection-enhanced delivery of carboplatin into the white matter as a potential treatment for high-grade glioma. J Neurooncol 108:77–88. doi:10.1007/s11060-012-0833-4
Chowdhary SA, Ryken T, Newton HB (2015) Survival outcomes and safety of carmustine wafers in the treatment of high-grade gliomas: a meta-analysis. J Neurooncol 122:367–382. doi:10.1007/s11060-015-1724-2
Neuwelt EA, Frenkel EP, Diehl JT, Maravilla KR, Vu LH, Clark WK, Rapoport SI, Barnett PA, Hill SA, Lewis SE et al (1979) Osmotic blood–brain barrier disruption: a new means of increasing chemotherapeutic agent delivery. Trans Am Neurol Assoc 104:256–260
Valtonen S, Timonen U, Toivanen P, Kalimo H, Kivipelto L, Heiskanen O, Unsgaard G, Kuurne T (1997) Interstitial chemotherapy with carmustine-loaded polymers for high-grade gliomas: a randomized double-blind study. Neurosurgery 41:44–48 (Discussion 48–49)
Brem H, Piantadosi S, Burger PC, Walker M, Selker R, Vick NA, Black K, Sisti M, Brem S, Mohr G, The Polymer-brain Tumor Treatment Group (1995) Placebo-controlled trial of safety and efficacy of intraoperative controlled delivery by biodegradable polymers of chemotherapy for recurrent gliomas. Lancet 345:1008–1012
Kemper EM, Boogerd W, Thuis I, Beijnen JH, van Tellingen O (2004) Modulation of the blood–brain barrier in oncology: therapeutic opportunities for the treatment of brain tumours? Cancer Treat Rev 30:415–423. doi:10.1016/j.ctrv.2004.04.001
Elliott PJ, Hayward NJ, Dean RL, Blunt DG, Bartus RT (1996) Intravenous RMP-7 selectively increases uptake of carboplatin into rat brain tumors. Cancer Res 56:3998–4005
Warren K, Jakacki R, Widemann B, Aikin A, Libucha M, Packer R, Vezina G, Reaman G, Shaw D, Krailo M et al (2006) Phase II trial of intravenous lobradimil and carboplatin in childhood brain tumors: a report from the Children’s Oncology Group. Cancer Chemother Pharmacol 58:343–347. doi:10.1007/s00280-005-0172-7
Carman AJ, Mills JH, Krenz A, Kim DG, Bynoe MS (2011) Adenosine receptor signaling modulates permeability of the blood–brain barrier. J Neurosci 31:13272–13280. doi:10.1523/JNEUROSCI.3337-11.2011
Fredholm BB, Ijzerman AP, Jacobson KA, Klotz KN, Linden J (2001) International Union of Pharmacology. XXV. Nomenclature and classification of adenosine receptors. Pharmacol Rev 53:527–552
Marala RB, Mustafa SJ (1998) Immunological characterization of adenosine A2A receptors in human and porcine cardiovascular tissues. J Pharmacol Exp Ther 286:1051–1057
Kassner A, Thornhill R (2011) Measuring the integrity of the human blood–brain barrier using magnetic resonance imaging. Methods Mol Biol 686:229–245. doi:10.1007/978-1-60761-938-3_10
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, Lieu H, Mahmarian JJ, Olmsted A, Underwood SR et al (2007) Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 14:645–658
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Portnow J, Badie B, Chen M, Liu A, Blanchard S, Synold TW (2009) The neuropharmacokinetics of temozolomide in patients with resectable brain tumors: potential implications for the current approach to chemoradiation. Clin Cancer Res 15:7092–7098. doi:10.1158/1078-0432.CCR-09-1349
Ostermann S, Csajka C, Buclin T, Leyvraz S, Lejeune F, Decosterd LA, Stupp R (2004) Plasma and cerebrospinal fluid population pharmacokinetics of temozolomide in malignant glioma patients. Clin Cancer Res 10:3728–3736. doi:10.1158/1078-0432.CCR-03-0807
Doolittle ND, Muldoon LL, Culp AY, Neuwelt EA (2014) Delivery of chemotherapeutics across the blood–brain barrier: challenges and advances. Adv Pharmacol 71:203–243. doi:10.1016/bs.apha.2014.06.002
Vykhodtseva N, McDannold N, Hynynen K (2008) Progress and problems in the application of focused ultrasound for blood–brain barrier disruption. Ultrasonics 48:279–296. doi:10.1016/j.ultras.2008.04.004
Grossman R, Tyler B, Rudek MA, Kim E, Zadnik P, Khan U, Blakeley JO, Pathak AP, Brem H (2013) Microdialysis measurement of intratumoral temozolomide concentration after cediranib, a pan-VEGF receptor tyrosine kinase inhibitor, in a U87 glioma model. Cancer Chemother Pharmacol 72:93–100. doi:10.1007/s00280-013-2172-3
Zhou Q, Guo P, Wang X, Nuthalapati S, Gallo JM (2007) Preclinical pharmacokinetic and pharmacodynamic evaluation of metronomic and conventional temozolomide dosing regimens. J Pharmacol Exp Ther 321:265–275
Denny BJ, Wheelhouse RT, Stevens MF, Tsang LL, Slack JA (1994) NMR and molecular modeling investigation of the mechanism of activation of the antitumor drug temozolomide and its interaction with DNA. Biochemistry 33:9045–9051
Rudek MA, Donehower RC, Statkevich P, Batra VK, Cutler DL, Baker SD (2004) Temozolomide in patients with advanced cancer: phase I and pharmacokinetic study. Pharmacotherapy 24:16–25
Tator CH, Morley TP, Olszewski J (1965) A study of the factors responsible for the accumulation of radioactive iodinated human serum albumin (Rihsa) by intracranial tumours and other lesions. J Neurosurg 22:60–76. doi:10.3171/jns.1965.22.1.0060
Neuwelt EA, Varallyay CG, Manninger S, Solymosi D, Haluska M, Hunt MA, Nesbit G, Stevens A, Jerosch-Herold M, Jacobs PM et al (2007) The potential of ferumoxytol nanoparticle magnetic resonance imaging, perfusion, and angiography in central nervous system malignancy: a pilot study. Neurosurgery 60:601–611. doi:10.1227/01.NEU.0000255350.71700.37 (Discussion 611–612)
Hossmann KA, Bothe HW, Bodsch W, Paschen W (1983) Pathophysiological aspects of blood–brain barrier disturbances in experimental brain tumors and brain abscesses. Acta Neuropathol Suppl 8:89–102
Salcman M, Scott EW, Schepp RS, Knipp HC, Broadwell RD (1982) Transplantable canine glioma model for use in experimental neuro-oncology. Neurosurgery 11:372–381
Acknowledgments
This work was supported in part by fellowship support T32GM066691 in Johns Hopkins Clinical pharmacology training program (Sadhana Jackson). The project described was supported by the Analytical Pharmacology Core of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins (National Institutes of Health grants P30 CA006973 and UL1 TR 001079, and Shared Instrument Grant 1S10RR026824-01). Grant Number UL1 TR 001079 is from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health, and National Institutes of Health Roadmap for Medical Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Jackson, S., Anders, N.M., Mangraviti, A. et al. The effect of regadenoson-induced transient disruption of the blood–brain barrier on temozolomide delivery to normal rat brain. J Neurooncol 126, 433–439 (2016). https://doi.org/10.1007/s11060-015-1998-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1998-4