Abstract
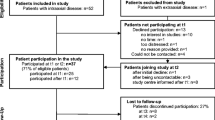
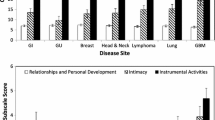
Patients diagnosed with primary brain tumors such as glioma experience psychological distress throughout the illness trajectory. Determining which patient characteristics are associated with more severe mood disturbance throughout the illness trajectory can help identify patients at risk and assist in developing targeted interventions based on these factors. Adult glioma patients were eligible for participation. Data collection tools included an investigator completed clinician assessment tool, patient completed demographic form and the Profile of mood states-short form. A multiple regression model was used to describe the relationship between the patient groups and clinical factors. The study enrolled 186 glioma patients of various tumor grades, who were categorized in three groups (newly diagnosed, on-treatment, follow-up) based on disease status at time of visit. Newly diagnosed patients experienced more total mood disturbance than all the other groups. Characteristics associated with more severe mood disturbance varied by patient group: newly diagnosed patients who were not on corticosteroids and were not married were more likely to have higher mood disturbance [R2 = 0.27, F (2, 29) = 5.31, p < 0.02]. For those on treatment, the use of concomitant medications, having more than 1 recurrence and low income predicted higher mood disturbance [R2 = 0.417, F (4, 67) = 11.98, p < 0.001]. For those not on active treatment, female sex, anti-depressant use and having a lower income was associated with higher mood disturbance [R2 = 0.183, F (3, 55) = 4.11, p < 0.02]. Additionally, when compared to other cancer groups, glioma patients reported similar mood disturbance to those with breast cancer. Factors other than disease characteristics are associated with higher mood disturbance and vary according to current disease status. The use of concomitant medications, demographic factors, recurrence and income are associated with mood disturbance and interventions may need to be tailored to these underlying factors.
Similar content being viewed by others
References
American Cancer Society (2012) Cancer facts and figures 2012. American Cancer Society, Atlanta, Ga. Available online Last accessed 24 Sep 2012
Dolecek TA, Propp JM, Stroup NE (2012) Kruchko, CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005–2009. J Neurooncol 14(5):1–49
Rooney AG, Carson A, Grant R (2011) Depression in cerebral glioma patients: a systematic review of observational studies. J Natl Cancer Inst 103(1):61–76
Wellisch DK, Kaleita TA, Freeman D, Cloughesy T, Goldman J (2002) Predicting major depression in brain tumor patients. Psycho-Oncology 11:230–238
Mainio A et al (2005) Depression and functional outcome in patients with brain tumors: a population-based 1-year follow-up study. J Neurosurg 103(5):841–847
Rooney AG, McNamara S, Mackinnon M, Fraser M, Rampling R, Carson A, Grant R (2011) Frequency, clinical associations, and longitudinal course of major depressive disored in adults with cerebral glioma. J Clin Oncol 29(32):4307–4312
Pringle AM, Taylor R, Whittle IR (1999) Anxiety and depression in patients with an intracranial neoplasm before and after tumour surgery. Br J Neurosurg 13(1):46–51
Lin L et al (2012) Validation of the Mishel’s uncertainty in illness scale-brain tumor form (MUIS-BT). J Neurooncol
Baker F et al (2002) A POMS short form for cancer patients: psychometric and structural evaluation. Psychooncology 11(4):273–281
Armstrong TS et al (2006) Validation of the M.D. anderson symptom inventory brain tumor module (MDASI-BT). J Neurooncol 80(1):27–35
Armstrong TS et al (2009) Clinical utility of the MDASI-BT in patients with brain metastases. J Pain Symptom Manage 37(3):331–340
Gould R, Brown SL, Bramwell R (2010) Psychological adjustment to gynaecological cancer: patients’ illness representations, coping strategies and mood disturbance. Psychol Health 25(5):633–649
Rottmann N, Dalton SO, Bidstrup PE, Wurtzen H, Hoybye MT, Ross L, Christensen J, Frederiksen K, Hansen DG, Johansen C (2011) No improvement in distress and quality of life following psychosocial cancer rehabilitation. A randomised trial. Psycho-Oncology 21:505–514
Conti CM et al (2011) Relationship between cancer and psychology: an updated history. J Biol Regul Homeost Agents 25(3):331–339
Struik K et al (2009) Fatigue in low-grade glioma. J Neurooncol 92(1):73–78
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359(5):492–507
Shi Q et al (2011) Symptom burden in cancer survivors 1 year after diagnosis: a report from the American cancer society’s studies of cancer survivors. Cancer 117(12):2779–2790
Markman M, Luce R (2010) Impact of the cost of cancer treatment: an internet-based survey. J Oncol Pract 6(2):69–73
Acknowledgments
Authors' received funds from CERN foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Acquaye, A.A., Vera-Bolanos, E., Armstrong, T.S. et al. Mood disturbance in glioma patients. J Neurooncol 113, 505–512 (2013). https://doi.org/10.1007/s11060-013-1143-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1143-1