Abstract
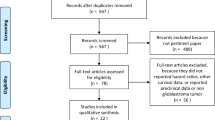
Glucocorticoids ameliorate neurologic symptoms in patients with glioblastoma, but their adverse effects limit long-term use. This study sought to identify factors associated with steroid taper success or failure in the early stages of glioblastoma treatment. We retrospectively reviewed steroid prescribing practices from date of surgery until one month following radiotherapy (RT) completion among 85 patients with newly diagnosed glioblastoma who were treated on a prospective clinical trial with RT and temozolomide. Sufficient information on steroid dosing was available in 72 patients included in the final analysis. The mean age was 54 years, and 65 % were men. Thirty-nine percent had a gross-total resection. Fifteen patients (21 %) tolerated steroid taper without requiring dose increase during the study. Men and patients with Karnofsky performance scale 90–100 were more likely to have a successful steroid taper. The most common symptom of taper failure was headache, but the reason for steroid increase differed among the different time intervals examined: worsening neurologic deficit in the early post-operative period, headache and non-focal symptoms during RT, and headache and seizure post-RT. Of the 50 patients in whom steroid use during RT was known, 36 (72 %) underwent dose reduction and of those, 21 (58 %) required an increase. The successful early taper of steroids in glioblastoma was associated with male gender and better functional status. Steroids are often tapered during RT, but there is frequent taper failure with this approach. A prospective trial with standardized steroid dosing regimens would be needed to verify these findings.
Similar content being viewed by others
References
DeAngelis LM (1994) Management of brain metastases. Cancer Invest 12:156–165
Koehler PJ (1995) Use of corticosteroids in neuro-oncology. Anticancer Drugs 6:19–33
Nahaczewski AE, Fowler SB, Hariharan S (2004) Dexamethasone therapy in patients with brain tumors–a focus on tapering. J Neurosci Nurs 36:340–343
Richter B, Neises G, Clar C (2002) Glucocorticoid withdrawal schemes in chronic medical disorders. A systematic review. Endocrinol Metab Clin North Am 31:751–758
Stummer W (2007) Mechanisms of tumor-related brain edema. Neurosurg Focus 22:E8
Hopkins RL, Leinung MC (2005) Exogenous Cushing’s syndrome and glucocorticoid withdrawal. Endocrinol Metab Clin North Am 34:371–384
Clarke JL, Iwamoto FM, Sul J, Panageas K, Lassman AB, DeAngelis LM, Hormigo A, Nolan CP, Gavrilovic I, Karimi S, Abrey LE (2009) Randomized phase II trial of chemoradiotherapy followed by either dose-dense or metronomic temozolomide for newly diagnosed glioblastoma. J Clin Oncol 27:3861–3867
Hohwieler Schloss M, Freidberg SR, Heatley GJ, Lo TC (1989) Glucocorticoid dependency as a prognostic factor in radiotherapy for cerebral gliomas. Acta Oncol 28:51–55
Watne K, Hannisdal E, Nome O, Hager B, Hirschberg H (1993) Prognostic factors in malignant gliomas with special reference to intra-arterial chemotherapy. Acta Oncol 32:307–310
Gundersen S, Lote K, Hannisdal E (1996) Prognostic factors for glioblastoma multiforme–development of a prognostic index. Acta Oncol 35(Suppl 8):123–127
Gelblum DY, Lee H, Bilsky M, Pinola C, Longford S, Wallner K (1998) Radiographic findings and morbidity in patients treated with stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 42:391–395
Ryan R, Booth S, Price S (2012) Corticosteroid-use in primary and secondary brain tumour patients: a review. J Neurooncol 106:449–459
Pruitt AA (2011) Medical management of patients with brain tumors. Curr Treat Options Neurol 13:413–426
Sturdza A, Millar BA, Bana N, Laperriere N, Pond G, Wong RK, Bezjak A (2008) The use and toxicity of steroids in the management of patients with brain metastases. Support Care Cancer 16:1041–1048
Wissinger JP, French LA, Gillingham FJ (1967) The use of dexamethasone in the control of cerebral oedema. J Neurol Neurosurg Psychiatry 30:588
Vecht CJ, Hovestadt A, Verbiest HB, van Vliet JJ, van Putten WL (1994) Dose-effect relationship of dexamethasone on Karnofsky performance in metastatic brain tumors: a randomized study of doses of 4, 8, and 16 mg per day. Neurology 44:675–680
Ryken TC, McDermott M, Robinson PD, Ammirati M, Andrews DW, Asher AL, Burri SH, Cobbs CS, Gaspar LE, Kondziolka D, Linskey ME, Loeffler JS, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Kalkanis SN (2010) The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96:103–114
Weissman DE, Janjan NA, Erickson B, Wilson FJ, Greenberg M, Ritch PS, Anderson T, Hansen RM, Chitambar CR, Lawton CA et al (1991) Twice-daily tapering dexamethasone treatment during cranial radiation for newly diagnosed brain metastases. J Neurooncol 11:235–239
Acknowledgments
Dr. Andrew Lassman received research funding and honoraria for consulting and speaking for Schering Plough/Merck
Funding
The clinical trial associated with this study was supported with funding from Schering-Plough/Merck
Conflict of interest
Dr. Mariel Deutsch, Dr. Katherine Panageas, Dr. Lisa M. DeAngelis do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deutsch, M.B., Panageas, K.S., Lassman, A.B. et al. Steroid management in newly diagnosed glioblastoma. J Neurooncol 113, 111–116 (2013). https://doi.org/10.1007/s11060-013-1096-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1096-4