Abstract
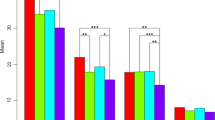
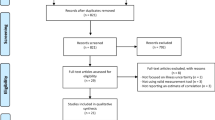
The Mishel uncertainty in illness scale (MUIS) has been used extensively with other solid tumors throughout the continuum of illness. Interventions to manage uncertainty have been shown to improve mood and symptoms. Patients with primary brain tumors (PBT) face uncertainty related to diagnosis, prognosis, symptoms and response. Modifying the MUIS to depict uncertainty in PBT patients will help define this issue and allow for interventions to improve quality of life. Initially, 15 experts reviewed the content validity of the MUIS-brain tumor form (MUIS-BT). Patients diagnosed with PBT then participated in the study to test validity and reliability. Data was collected at one point in time. Six out of 33 items in the original MUIS were modified to better describe PBT patients’ uncertainty. 32 of the 186 patients in the second-stage of the study were newly diagnosed with PBT, 85 were on treatment, and 69 were followed-up without active treatment. The validity of the MUIS-BT was demonstrated by its correlations with mood states (P < 0.01) and symptom severity (P < 0.01) and interference (P < 0.01). The MUIS-BT measures four constructs: ambiguity/inconsistency, unpredictability of disease prognosis, unpredictability of symptoms and other triggers, and complexity. Cronbach’s alphas of the four subscales were 0.90, 0.77, 0.75 and 0.65, respectively. The 33-item MUIS-BT demonstrated adequate select measures of validity and reliability in PBT patients. Based on this initial validation and significant correlations with symptom distress and mood states, further understanding of uncertainty and evaluation of measures to help manage patients’ uncertainty can be evaluated which in turn may improve coping and quality of life.
Similar content being viewed by others
References
Preusser M, de Ribaupierre S, Wöhrer A, Erridge SC, Hegi M, Weller M, Stupp R (2011) Current concepts and management of glioblastoma. Ann Neurol 70:9–21
Stupp R, Hegi ME, Gilbert MR, Chakravarti A (2007) Chemoradiotherapy in malignant glioma: standard of care and future directions. J Clin Oncol 25:4127–4136
Mishel MH (1988) Uncertainty in illness. Image J Nurs Sch 20:225–232
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJB, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross G, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJB, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomized phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Brandes AA, Tosoni A, Spagnolli F, Frezza G, Leonardi M, Calbucci F, Franceschi E (2008) Disease progression or pseudoprogression after concomitant radiochemotherapy treatment: pitfalls in neurooncology. Neuro Oncol 10:361–367
Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9:453–461
Cordova MJ, Andrykowsky MA, Kenady DE, McGrath PC, Sloan DA, Redd WH (1995) Frequency and correlations of posttraumatic-stress-disorder-like-symptoms after treatment for breast cancer. J Consult Clin Psychol 63:981–986
Osoba D, Aaronson N, Zee B, Sprangers M, te Velde A (1997) Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. Qual Life Res 6:103–108
Cella DF, Tulsky DS, Gray G, Sarafian BS, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579
Weitzner MA, Meyers CA, Gelke CK, Byrne KS, Cella DF, Levin VA (1995) The functional assessment of cancer therapy (FACT) scale: development of a brain subscale and revalidation of the general version (FACT-G) in patients with primary brain tumors. Cancer 75:1151–1161
Mishel MH (1981) The measurement of uncertainty in illness. Nurs Res 30:258–263
Mishel MH (1990) Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch 22:256–262
Mishel MH (1999) Uncertainty in chronic illness. Annu Rev Nurs Res 17:269–294
Polit DF, Beck C (2006) Essentials of nursing research: methods, appraisal and utilization, 6th edn. Lippincott Williams & Wilkins, Philadelphia
Mishel MH (1984) Perceived uncertainty and stress in illness. Res Nurs Health 7:163–171
Mishel MH, Braden CJ (1987) Uncertainty: a mediator between support and adjustment. West J Nurs Res 9:43–57
Armstrong TS, Mendoza T, Gning I, Coco C, Cohen MZ, Eriksen L, Hsu M, Gilbert MR, Cleeland C (2006) Validation of the M.D. Anderson symptom inventory brain tumor module (MDASI-BT). J Neurooncol 80:27–35
McNair DM, Lorr M, Droppleman LF (1971) EITS manual for the profile of mood states. Educational & Industrial Testing Service, San Diego
Shacham S (1983) A shortened version of the profile of mood states. J Pers Assess 47:305–306
Baker F, Denniston M, Zabora J, Polland A, Dudley WN (2002) A POMS short form for cancer patients: psychometric and structural evaluation. Psychooncology 11:273–281
Soeken KL (2010) Validity of measures. In: Waltz CF, Strickland OL, Lenz ER (eds) Measurement in nursing and health research, 4th edn. Springer, New York, pp 163–201
Nunnally JC, Bernstein IH (1994) Psychometric theory, 3rd edn. McGraw-Hill, New York
Lin L, Acquaye AA, Vera-Bolanos E, Cahill J, Gilbert MR, Armstrong TS (2011) QL-13: reliability and validity of the MUIS-brain tumor form (MUIS-BT). Neuro Oncol 13(suppl 3):124
Mishel MH (1983) Parents’ perception of uncertainty concerning their hospitalized child. Nurs Res 32:324–330
Armstrong TS, Vera-Bolanos E, Gning I, Acquaye A, Gilbert MR, Cleeland C, Mendoza T (2011) The impact of symptom interference using the MD Anderson symptom inventory brain tumor module (MDASI-BT) on prediction of recurrence in primary brain tumor patients. Cancer 117:3222–3228
Acquaye AA, Lin L, Aspenson AC, Cahill J, Vera-Bolanos E, Gilbert MR, Armstrong TS (2011) QL-11: mood disturbance in patients with brain tumors. Neuro Oncol 13(suppl 3):123
Acknowledgments
This study is supported by the Elizabeth W. Quinn Oncology Research Award from the University of Texas Health Science Center at Houston, School of Nursing. The authors would like to thank the research subjects for their participation. The authors would also like to thank the clinical experts and Dr. Mishel for evaluating the content validity of MUIS-BT.
Funding
This study is supported by the Elizabeth W. Quinn Oncology Research Award from the University of Texas Health Science Center at Houston, School of Nursing.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, L., Acquaye, A.A., Vera-Bolanos, E. et al. Validation of the Mishel’s uncertainty in illness scale-brain tumor form (MUIS-BT). J Neurooncol 110, 293–300 (2012). https://doi.org/10.1007/s11060-012-0971-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0971-8