Summary
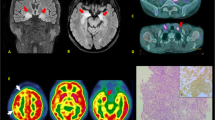
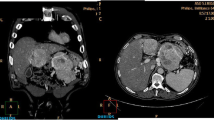
Memory loss can be a symptom of paraneoplastic limbic encephalitis (PLE) a neuropsychiatric disorder associated mostly with small-cell lung cancer and anti-Hu antibodies or with testicular tumors and anti-Ma2 antibodies. We present the case of a patient with temporal coincidence of beginning cognitive decline and diagnosis of a carcinoma of the prostate in whom we diagnosed anti-Ma1/Ma2-positive PLE. The tumor had been completely resected but memory impairment further deteriorated. As the effective treatment of the cancer is considered as the most efficient treatment of a paraneoplastic neurological syndrome (PNS) a second neoplasia was suspected in the patient. By the aid of whole body positron emission tomography with 18-fluorine fluoro-2-deoxy-glucose (FDG-PET) an adenocarcinoma of the cecum could be detected. Two months after surgery anti-Ma antibodies were negative. We conclude that a second neoplasia should be considered, if effective cancer treatment does not lead to improvement or stabilisation of a PNS. Tumor search should be exhaustive and include PET when conventional imaging fails to show a malignancy.
Similar content being viewed by others
References
Voltz R, 2002 Paraneoplastic neurological syndromes: an update on diagnosis pathogenesis, and therapy Lancet Neurol 1: 294–305
Graus F, Delattre JY, Antoine JC, et al. 2004 Recommended diagnostic criteria for paraneoplastic neurological syndromes J Neurol Neurosurg Psychiatry 75: 1135–1140
Gultekin SH, Rosenfeld MR, Votz R, et al. 2000 Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients Brain 123: 1481–1494
Hulstaert F, Blennow K, Ivanoiu A, et al., 1999 Improved discrimination of AD patients using beta-amyloid 1–42 and tau levels in CSF Neurology 52: 1555–1562
Saiz A, Graus F, Dalmau J, et al. 1999 Detection of 14-3-3 brain protein in the cerebrospinal fluid of patients with paraneoplastic neurological disorders Ann Neurol 46: 774–777
Modrego PJ, Cay A, Pina MA, Monge A, 2002 Paraneoplastic subacute encephalitis caused by adenocarcinoma of prostate: a clinico-pathological case report Acta Neurol Scand 105: 351–353
Graus F, Keime-Guibert F, Ramon R, et al. 2001 Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients Brain 124: 1138–1148
Stern RC, Hulette CM, 1999 Paraneoplastic limbic encephalitis associated with small cell carcinoma of the prostate Mod Pathol 12 (8): 814–818
Dalmau J, Gultekin H, Voltz R, et al. 1999 Ma1, a novel neuron- and testis-specific protein, is recognized by the serum of patients with paraneoplastic neurological disorders Brain 122: 27–39
Rosenfeld MR, Eichen JG, Deborky FW, et al. 2001 Molecular and clinical diversity in paraneoplastic immunity to Ma proteins Ann Neurol 50: 339–348
Dalmau J, Graus F, Villarejo A, et al. 2004 Clinical analysis of anti-Ma2-associated encephalitis Brain 127: 1831–1844
Voltz R, Gultekin H, Rosenfeld MR, et al. 1999 A serologic marker of paraneoplastic limbic and brain-stem encephalitis in patients with testicular cancer N Engl J Med 340: 1788–1795
Linke R, Schroeder M, Helmberger T, Voltz R, 2004 Antibody-positive paraneoplastic neurologic syndromes. Value of CT and PET for tumor diagnosis Neurology 63: 282–286
Rees JH, Hain SF, Johnson MR, et al. 2001 The role of (18F)fluoro-2-deoxyglucose-PET scanning in the diagnosis of paraneoplastic neurological disorders Brain 124: 2223–2231
Antoine JC, Cinotti L, Tilikete C, et al. 2000 (18F)Fluorodeoxyglucose Positron Emission Tomography in the diagnosis of cancer in patients with paraneoplastic neurological syndrome and anti-Hu antibodies Ann Neurol 48: 105–108
Younes-Mhenni S, Janier MF, Cinotti L, et al. 2004 FDG-PET improves tumour detection in patients with paraneoplastic neurological syndromes Brain 127: 2331–2338
Acknowledgements
We thank M. Reimold, PET-Center of the University of Tübingen, for kindly providing the PET images of the described patient.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leyhe, T., Schüle, R., Schwärzler, F. et al. Second primary tumor in anti-Ma1/2-positive paraneoplastic limbic encephalitis . J Neurooncol 78, 49–51 (2006). https://doi.org/10.1007/s11060-005-9052-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-005-9052-6