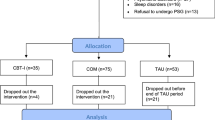
Objectives. To assess the efficacy of the cognitive behavioral therapy of insomnia (CBT-I) compared with pharmacotherapy in chronic insomnia in the Russian population. Materials and methods. A crossover trial was performed in 42 patients with chronic insomnia (14 men and 28 women) aged 29–80 years old, who received two courses of treatment: using zopiclone and using an educational method with elements of CBT-I. All patients underwent nocturnal polysomnography studies. Treatment efficacy was evaluated using the Insomnia Severity Index, the Pittsburgh Sleep Quality Index questionnaire, the Dysfunctional Beliefs about Sleep Scale, the Sleep Hygiene Index, and the Beck Depression Scale. The efficacy of medication and nonmedication treatment methods in insomnia were found to be comparable. The insomnia severity index after CBT-I decreased by 3.6 (from 17.7 ± 5.3 to 12.8 ± 5.1) points, compared with a decrease by 4.9 (from 16.5 ± 5.8 to 12.9 ± 6.2) points after courses of zopiclone (p < 0.05). However, after two weeks, treatment results persisted only after use of CBT (12.9 ± 6.2 points); scores increased to 15.5 ± 4.6 points by the end of zopiclone administration. In addition, CBT-I was followed by significant decreases in values on the Beck Depression Scale (from 11.8 ± 6.9 to 8.5 ± 7.0 points), the Sleep Hygiene Index (from 26.9 ± 7.5 to 23.9 ± 5.7 points), the Dysfunctional Beliefs about Sleep Scale, (from 104.9 ± 29.7 to 84.4 ± 34.2 points) (p < 0.05). Patients responding to CBT-I were younger than nonresponders (40.5 ± 12.9 and 57.2 ± 11.7 years, respectively, p < 0.05), such that young age can be regarded as a predictor for CBT-I being effective. Conclusions. Treatment of chronic insomnia using CBT was as effective as pharmacotherapy, its use was accompanied by additional improvements in emotional status, and its effects lasted longer.
Similar content being viewed by others
Change history
31 January 2019
The third author?s name should read M. G. Poluektov.
31 January 2019
The third author���s name should read M. G. Poluektov.
References
M. G. Poluektov (ed.), Somnology and Sleep Medicine; National Guidelines in Memory of A. M. Vein and Ya. I. Levin, Medforum, Moscow (2016).
A. Vgontzas, D. Liao, E. Bixler, A. Vela-bueno, and G. P. Chrousos, “Insomnia with objective short sleep duration is associated with a high risk for hypertension,” Sleep, 32, No. 4, 491–497 (2009).
F. Sofi , F. Cesari, and A. Casini, “Insomnia and risk of cardiovascular disease: a meta-analysis,” Eur. J. Prevent. Cardiol., 21, No. 1, 57–64 (2014), https://doi.org/10.1177/2047487312460020.
L. Meng, Y. Zheng, and R. Hui, “The relationship of sleep duration and insomnia to risk of hypertension incidence: a meta-analysis of prospective cohort studies,” Hypertens. Res., 36, 985–995 (2013), https://doi.org/10.1038/hr.2013.70.
S. Schutte-Rodin, L. Broch, D. Buysse, C. Dorsey, and M. Sateia, “Clinical guideline for the evaluation and management of chronic insomnia in adults,” J. Clin. Sleep Med., No. 5, 487–504 (2008).
J. F. Pagel and B. L. Parnes, “Medications for the treatment of sleep disorders: an overview,” J. Clin. Psychiatry, 3, 118–125 (2001), https://doi.org/10.4088/pcc.v03n0303.
Y. Ma, G. Dong, C. Mita, S. Sun, C. K. Peng, and A. C. Yang, “Publication analysis on insomnia: how much has been done in the past two decades?” Sleep Med., 16, 820–826 (2015), https://doi.org/10.1016/j.sleep.2014.12.028.
O. V. Slesarev, D. A. Trunin, and I. M. Bairikov, “Cognitive behavioral therapy of temporomandibular disorders complicated by chronic pain: challenges, prospects and limitations,” Ross. Stomatol. Zh., 20, No. 4, 209–214 (2016), https://doi.org/10.18821/1728-2802.
E. Yu. Suslova and V. A. Parfenov, “A complex approach to the treatment of patients with chronic lumbalgia,” Zh. Nevrol. Psikhiat., 115, No. 10, Iss. 2. 16–21 (2015).
N. V. Strueva, G. A. Mel’nichenko, M. G. Poluektov, and L. V. Savel’eva, “Efficacy of the treatment of obesity in patients with insomnia and obstructive sleep apnea syndrome,” Ozhiren. Metab., 13, No. 2, 26–32 (2016).
The International Classification of Sleep Disorders: Diagnostic and Coding Manual, American Academy of Sleep Medicine, Darien (2014), https://doi.org/10.7326/0003-4819-115-5-413_1.
D. J. Buysse, A. Germain, D. E. Moul, P. Franzen, L. K. Brar, M. E. Fletcher, A. Begley, P. R. Houck, S. Mazumdar, C. F. Reynolds, III, and T. H. Monk, “Efficacy of brief behavioral treatment for chronic insomnia in older Adults,” Arch. Intern. Med., 171, No. 10, 887–889 (2011), https://doi.org/10.1001/archinternmed.2010.535.
C. Iber, S. Ancoli-Israel, A. L. Chesson, Jr., and S. F. Quan, The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications, American Academy of Sleep Medicine, Westchester, IL, (2007); p. 59, https://doi.org/10.1007/978-3-7985-1852-0_7.
R. B. Berry, R. Budhiraja, D. J. Gottlieb, C. Iber, V. K. Kapur, C. L. Marcus, R. Mehra, S. Parthasarath, S. F. Quan, S. Redline, K. P. Strohl, S. L. Davidson Ward, and M. M. Tangredi, “Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine,” J. Clin. Sleep Med., 8, 597–619 (2012), https://doi.org/10.5664/jcsm.2172.
A. T. Beck, R. A. Steer, and G. Brown, Beck Depression Inventory-II. PsycTESTS Dataset, https://doi.org/10.1037/t00742-000.
C. D. Spielberger, Studies of Anxiety, adapted by I. B. Hanin, Diagnosis of Emotional and Moral Development, edited and compiled by I. B. Dermanov, St. Petersburg (2002).
E. G. Starostina, G. D. Teilor, L. K. Kvilti, A. E. Bobrov, E. N. Moshnyaga, N. V. Puzyreva, M. A. Bobrova, M. G. Ivashkina, M. N. Krivchikova, E. P. Shavrikova, and R. M. Begbi, “The Toronto Alexithymia Scale (20 Points): validation of the Russian-language version on a cohort of therapy patients,” Sots. Klin. Psikhiatr., 4, No. 20, 31–38 (2010).
Five-factor Personality Questionnaire. Methodological Guidelines, A. B. Khromov (ed.), Kurgan State University Press, Kurgan (2000).
S. Morin, G. Belleville, and L. Belanger, “The ISI: Psychometric Indicators to detect insomnia cases and evaluate treatment response,” Sleep, 34, No. 5, 601–608 (2011).
D. J. Buysse, C. F. Reynolds, T. H. Monk, S. R. Berman, and D. J. Kupfer, “The Pittsburgh Sleep Quality Index (PSQI): a new instrument for psychiatric research and practice,” Psychiatry Res., 28, 193–213 (1989), https://doi.org/10.1016/0165-1781(89)90047-4.
D. F. Mastin, J. Bryson, and R. Corwyn, “Assessment of sleep hygiene using the Sleep Hygiene Index,” J. Behav. Med., 29, No. 3, 223–227 (2006), https://doi.org/10.1007/s10865-006-9047-6.
A. Sh. Tkhostov and E. I. Rasskazova, The Dysfunctional Beliefs about Sleep Scale. Methodological Guidelines, Moscow State Univ. Press, Moscow (2007).
C. Morin, A. Vallieres, B. Guay, H. Ivers, J. Savard, C. Merette, C. Bastien, and L. Baillargeon, “Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia,” JAMA, 301, 2005–2015 (2009), https://doi.org/10.1001/jama.2009.682.
M. Sato, W. Yamadera, M. Matsushima, H. Itoh, and K. Nakayama, “Clinical efficacy of individual cognitive behavior therapy for psychophysiological insomnia in 20 outpatients,” Psych. Clin. Neurosci., 64, 187–195 (2010), https://doi.org/10.1111/j.1440-1819.2009.02060.x.
Y. Ma, M. Dong, C. Mita, S. Sun, C.-K. Peng, and A. C. Yang, “Publication analysis on insomnia: how much has been done in the past two decades?” Sleep Med., 16, 820–826 (2015), https://doi.org/10.1016/j.sleep.2014.12.028.
E. C. Mason and A. G. Harvey, “Insomnia before and after treatment for anxiety and depression,” J. Affect. Disord., 168, 415–421 (2014), https://doi.org/10.1016/j.jad.2014.07.020.
W. M. Troxel, T. S. Conrad, A. Germain, and J. D. Buysse, “Predictors of treatment response to Brief Behavioral Treatment of Insomnia (BBTI) in older adults,” J. Clin. Sleep Med., 9, No. 12, 1281–1289 (2013), https://doi.org/10.5664/jcsm.3270.
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Zhurnal Nevrologii i Psikhiatrii imeni S. S. Korsakova, Vol. 117, No. 4, Iss. II, Sleep Disorder, pp. 48–55, April, 2017.
Rights and permissions
About this article
Cite this article
Pchelina, P.V., Tabidze, A.A. & Poluekotov, M.G. A Comparative Study of the Efficacy of Cognitive Behavioral Therapy and Zopiclone in Chronic Insomnia. Neurosci Behav Physi 49, 38–44 (2019). https://doi.org/10.1007/s11055-018-0688-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11055-018-0688-z