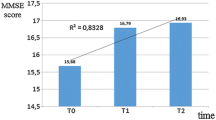
Objective – to compare different doses of escitalopram (Cipralex) in the prophylaxis of dementia in patients with depression and moderate cognitive dysfunction on the background of chronic cerebral ischemia. Materials and methods. Two groups of patients, aged 65–78 years, with chronic cerebral ischemia and mild-moderate depression and moderate cognitive dysfunction were studied and treated with different doses of escitalopram: 30 patients received escitalopram at a dose of 5 mg/day throughout the treatment period; 42 patients received escitalopram at a dose of 5 mg/day for the fi rst week and then 10 mg/day. Treatment duration was six months and the observation period was eight months. Results and conclusions. Escitalopram was shown to be effective not only in the treatment of depression-associated cognitive dysfunction in patients with chronic cerebral ischemia but also in decreasing the risk of dementia in the long term. The effectiveness of the prophylaxis of dementia was found to depend on the escitalopram dose used.
Similar content being viewed by others
References
R. G. Troxler, E. A. Sprague, R. A. Albanese, et al., “The association of elevated plasma cortisol and early atherosclerosis as demonstrated by coronary angiography,” Atherosclerosis, 26, 151–162 (1977); doi: 10.1016/0021-9150(77)90098-3.
R. M. Carney, J. A. Blumenthal, P. K. Stein, et al., “Depression, heart rate variability, and acute myocardial infarction,” Circulation, 104, 2024–2028 (2001); doi: 10.1161/hc4201.097834.
P. L. Morris, R. G. Robinson, P. Andrzejewski, et al., “Association of depression with 10-year poststroke mortality,” Am. J. Psychiatry, 150, 124–129 (1993); doi: 10.1176/ajp.150.1.124.
J. H. Lichtman, E. S. Froelicher, J. A. Blumenthal, et al., “Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: A scientific statement from the American Heart Association,” Circulation, 129, No. 12, 1350–1369 (2014); doi: 10.1161/CIR.0000000000000019.
G. S. Alexopoulos, B. S. Meyers, R. C. Young, et al., “Vascular depression hypothesis,” Arch. Gen. Psychiatry, 54, 915–922 (1997); doi: 10.1001/archpsyc.1997.01830220033006.
M. May, P. McCarron, S. Stansfeld, et al., “Does psychological distress predict the risk of ischemic stroke and transient ischemic attack? The Caerphilly Study,” Stroke, 33, 7–12 (2002); doi: 10.1161/hs0102.100529.
S. L. Larson, P. L. Owens, D. Ford, and W. Eaton, “Depressive disorder, dysthymia, and risk of stroke. Thirteen-year follow-up from the Baltimore Epidemiological Catchment Area Study,” Stroke, 32, 1979–1983 (2001); doi: http://dx.doi.org/10.1161/hs0901.094623.
M. C. Pascoe, S. G. Crewther, L. M. Carey, and D. P. Crewther, “Inflammation and depression: why poststroke depression may be the norm and not exception,” Int. J. Stroke, 6, No. 2, 128–135 (2011); doi: http://dx.doi.org/10.1111/j.1747-4949.2010.00565.
A. Singh, S. E. Black, N. Nerrmann, et al., “Functional and neuroanatomic correlations in poststroke depression: The Sunnybrook Stroke Study,” Stroke, 31, 637–644 (2000); doi: http://dx.doi.org/10.1161/01.str.31.3.637.
R. G. Robinson, K. L. Kubos, L. B. Starr, et al., “Mood disorders in stroke patients. Importance of location of lesion,” Brain, 107, 81–93 (1984); doi: http://dx.doi.org/10.1093/brain/107.1.81.
S. H. Lee, M. E. Payne, D. C. Steffens, et al., “Subcortical lesion severity and orbitofrontal cortex volume in geriatric depression,” Biol. Psychiatry, 54, 529–533 (2003); doi: 10.1016/s0006-3223(03) 00063-5.
J. R. MacFall, M. E. Payne, J. E. Provenzale, and K. R. Krishnan, “Medial orbital frontal lesions in late-onset depression,” Biol. Psychiatry, 49, 803–806 (2001); doi: http://dx.doi.org/10.1016/s0006- 3223(00)01113-6.
S. M. MacHale, S. J. O’Rourke, J. M. Wardlaw, and M. S. Dennis, “Depression and its relation to lesion location after stroke,” J Neurol. Neurosurg. Psychiatry, 64, 371–374 (1998); doi: http://dx.doi.org/10.1136/jnnp.64.3.371.
K. Shimoda and R. G. Robinson, “The relationship between poststroke depression and lesion location in long-term follow-up,” Biol. Psychiatry, 45, 187–192 (1999); doi: 10.1016/s0006-3223(98) 00178-4.
D. Sinyor, P. Jacques, D. G. Kaloupek, et al., “Poststroke depression and lesion location: An attempted replication,” Brain, 109, 537–546 (1986); doi: 10.1093/brain/109.3.537.
R. Vataja, T. Pohjasvaara, A. Leppävuori, et al., “Magnetic resonance imaging correlates of depression after ischemic stroke,” Arch. Gen. Psychiatry, 58, 925–931 (2001); doi: 10.1001/archpsyc.58.10.925.
A. Berg, H. Palomäki M. Lehtihalmes, et al., “Poststroke depression: An 18-month follow-up,” Stroke, 34, 138–143 (2003); doi: 10.1161/01.str.0000048149.84268.07.
G. Gianotti, A. Azzoni, F. Gasparini, et al., “Relation of lesion location to verbal and nonverbal mood measures in stroke patients,” Stroke, 28, 2145–2149 (1997); doi: 10.1161/01.str.28.11.2145.
A. House, M. Dennis, C. Warlow, et al., “Mood disorders after stroke and their relation to lesion location: A CT scan study,” Brain, 113, 1113–1129 (1990); doi: 10.1093/brain/113.4.1113.
M. Åström, R. Adolfsson, and K. Asplund, “Major depression in stroke patients: A 3-year longitudinal study,” Stroke, 24, 976–982 (1993); doi: 10.1161/01.str.24.7.976.
D. Dam, H. E. Pedersen, and P. Ahlgren, “Depression among patients with stroke,” Acta Psychiatr. Scand., 80, 118–124 (1989).
B. S. Greenwald, E. Kramer-Ginsberg, and K. R. R. Krishnan, “Neuroanatomic localization of magnetic resonance imaging signal hyperintensities in geriatric depression,” Stroke, 29, 613–617 (1998); doi: 10.1161/01.str.29.3.613.
G. M. S. Nys, M. J. E. van Zandvoort, H. B. der Worp, et al., “Early depression symptoms after stroke: Neuropsychological correlates and lesion characteristics,” J. Neurol. Sci., 228, 27–33 (2005); doi: 10.1016/j.jns.2004.09.031.
F. Piamarta, S. Iurlaro, V. Isella, et al., “Unconventional affective symptoms and executive functions after stroke in the elderly,” Arch. Gerontol. Geriat., 9, Supplement, 315–323 (2004); doi: 10.1016/j.archger.2004.04.042.
S. E. Starkstein, J. P. Fedoroff, T. R. Price, et al., “Apathy following cerebrovascular lesions,” Stroke, 24, 1625–1630 (1993); doi: 10.1161/01.str.24.11.1625.
S. Yamagata, S. Yamaguchi, and S. Kovayashi, “Impaired novelty processing in apathy after subcortical stroke,” Stroke, 35, 1935–1940 (2004); doi: 10.1161/01.str.0000135017.51144.c9.
K. P. Bhatia, and C. D. Marsden, “The behavioural and motor consequences of focal lesions of the basal ganglia in man,” Brain, 117, 859–876 (1994); doi: 10.1093/brain/117.4.859.
R. Levy and B. Dubois, “Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits,” Cereb. Cortex, 16, 916–928 (2006); doi: 10.1093/cercor/bhj043.
F. Holsboer, “Stress, hypercortisolism and corticosteroid receptors in depression: implications for therapy,” J. Affect. Disord., 62, 77–91 (2001); doi: 10.1016/s0165-0327(00)00352-9.
F. Holsboer, “Corticotropin-releasing hormone modulations and depression,” Curr. Opin. Investig. Drugs, 4, 46–50 (2003).
J. M. Reul and F. Holsboer, “Corticotropin-releasing factor receptions 1 and 2 in anxiety and depression,” Curr. Opin. Pharmacol., 2, 23–33 (2002)l doi: 10.1016/S1471-4892(01)00117-5.
R. M. Sapolsky, “Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders,” Arch. Gen. Psychiatry, 57, 925–935 (2000); doi: 10.1001/archpsyc.57.10.925.
E. Fuchs and E. Gould, “Mini-review: in vivo neurogenesis in the adult brain: regulation and functional implications,” Eur. J. Neurosci., 12, 12211–2214 (2000); doi: 10.1046/j.1460-9568.2000. 00130.x.
M. A. Smith, S. Makino, R. Kvetnansky, and R. M. Post, “Effects of stress on neurotrophic factor expression in the rat brain,” Ann. NY Acad. Sci., 771, 234–239 (1995); doi: 10.1111/j.1749-6632.1995. tb44684.x.
M. Nibuya, S. Morinobu, and S. Duman, “Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments,” J. Neurosci., 15, 7639–7547 (1995).
B. Chen, D. Dowlatshahi, G. M. MacQueen, et al., “Increased hippocampal BDNF immunoreactivity in subjects treated with antidepressant medication,” Biol. Psychiatry, 50, 260–265 (2001); doi: 10.1016/s0006-3223(01)01083-6.
Y. I. Sheline, P. W. Wang, M. H. Gado, et al., “Hippocampal atrophy in recurrent major depression,” Proc. Natl. Acad. Sci. USA, 93, No. 9, 3908–3913 (1996); doi: 10.1073/pnas.93.9.3908.
Y. I. Sheline, M. Sanghavi, M. I. Mintun, and M. H. Gado, “Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depression,” J. Neurosci., 19, No. 12, 5034–5043 (1999).
Y. I. Sheline, M. H. Gado, and H. C. Kraemer, “Untreated depression and hippocampal volume loss,” Am. J. Psychiatry, 160, No. 8, 1516–1518 (2003); doi: 10.1176/appi.ajp.160.8.1516.
Y. I. Sheline, M. H. Gado, and J. L. Price, “Amygdala core nuclei volumes are decreased in recurrent major depression,” Neuroreport, 8, No. 9, 2023–2028 (1998).
J. D. Bremner, M. Vithilingham, E. Vermetten, et al., “Reduced volume of orbitofrontal cortex in major depression,” Biol. Psychiatry, 51, 273–279 (2002); doi: 10.1016/s0006-3223(01)01336-1.
C. E. Coffey, W. E. Wilkinson, R. D. Weiner, et al., “Quantitative cerebral anatomy in depression: a controlled magnetic resonance imaging study,” Arch. Gen. Psychiatry, 50, 7–16 (1993); doi: 10.1001/archpsyc.1993.01820130009002.
T. Lai, M. E. Payne, C. E. Byrum, et al., “Reduction of orbital frontal cortex volume in geriatric depression,” Biol. Psychiatry, 48, No. 10, 971–975 (2000); doi: 10.1016/s0006-3223(00)01042-8.
T. N. van den Kommer, H. C. Comijs, M. A. Aartsen, et al., “Depression and cognition: how do they interrelate in old age?” Am. J. Geriatr. Psychiatry, 21, No. 4, 398–410 (2013); doi: 10.1016/j.jagp.2012.12.01.
B. S. Diniz, M. A. Butters, S. M. Albert, et al., “Late-life depression and risk of vascular dementia and Alzheimer’s disease: systematic review and meta-analysis of community-based cohort studies,” Br. J. Psychiatry, 202, No. 5, 329–335, (2013); doi: 10.1192/bjp.bp.112.118307.
J. Altman and G. D. Das, “Autoradiographic and histologic evidence of postnatal neurogenesis in rats,” J. Comp. Neurol., 124, 319–335 (1965); doi: 10.1002/cne.901240303.
M. A. Kheirbek and R. Hen, “(Radio)active neurogenesis in the human hippocampus,” Cell, 153, No. 6, 1183–1184 (2013); doi: 10.1016/j.cell.2013.05.033.
G. S. Alexopoulos, C. F. Murphy, F. M. Gunning-Dixon, et al., “Serotonin transporter polymorphisms, microstructural white matter abnormalities and remission of geriatric depression,” J. Affect. Disord., 119, No. 1–3, 132–141 (2009); doi: 10.1016/j.jad.2009.03.004.
M. Boldrini, M. D. Underwood, R. Hen, et al., “Antidepressants increase neural progenitor cells in the human hippocampus,” Neuropsychopharmacology, 34, No. 11, 2376–2389 (2009); doi: 10.1038/npp.2009.75.
S. Bleakley, “Review of the choice and use of antidepressant drugs,” Prog. in Neurol. Psychiatry, 17, No. 6, 18–26 (2013); doi: 10.1002/pnp.311.
I. M. Anderson, I. N. Ferrier, R. C. Baldwin, et al., “Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2000 British Association for Psychopharmacology guidelines,” J. Psychopharm., 22, 343–396 (2008); doi: 10.1177/0269881107088441.
National Institute for Health and Care Excellence, Depression in Adults. Clinical Guideline CG90, NICE, (2009), http://guidance.nice.org.uk/CG90, acces. May 15, 2015.
I. Herrera-Guzmán, E. Gudayol-Ferré, J. E. Herrera-Abarca, et al., “Major depressive disorder in recovery and neuropsychological functioning: effects of selective serotonin reuptake inhibitor and dual inhibitor depression treatments on residual cognitive deficits in patients with major depressive disorder in recovery,” J. Affect. Disord., 123, No. 1–3, 341–350 (2010); doi: 10.1016/j.jad.2009.10.0.
G. B. Cassano, F. Puca, P. L. Scapicchio, and M. Trabucchi, Italian Study Group on Depression in Elderly Patients, “Paroxetine and fluoxetine effects on mood and cognitive functions in depressed nondemented elderly patients,” J. Clin. Psychiatry, 63, No. 5, 396–402 (2002); doi: 10.4088/jcp.v63n0504.
E. L. Constant, S. Adam, B. Gillain, et al., “Effects of sertraline on depressive symptoms and attentional and executive functions in major depression,” Depress. Anxiety, 21, No. 2, 78–89 (2005); doi: 10.1002/da.20060.
C. Katona, T. Hansen, and C. K. Olsen, “A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder,” Int. Clin. Psychopharmacol., 27, No. 4, 215–223 (2012); doi: 10.1097/yic.0b013e3283542457.
N. Ishikawa and K. Hashimoto, “The role of sigma-1 receptors in the pathophysiology of neuropsychiatric diseases,” J. Recept. Lig. Chann. Res., 3, 25–36 (2010); doi: 10.2147/JRLCR.S8453.
I. Ishima, Y. Fujita, and K. Hashimoto, “Interaction of new antidepressants with sigma-1 receptor chaperones and their potentiation of neurite outgrowth in PC12 cells,” Eur. J. Pharmacol., 727, 167–173 (2014); doi: 10.1016/j.ejphar.2014.01.064.
R. G. Robinson, R. E. Jorge, D. J. Moser, et al., “Escitalopram and problem-solving therapy for prevention of poststroke depression: a randomized controlled trial,” JAMA, 299, No. 20, 2391–2400 (2008); doi: 10.1001/jama.299.20.2391.
A. Rasmussen, M. Lunde, D. L. Poulsen, et al., “A double-blind placebo-controlled study of sertraline in prevention of depression in stroke patients,” Psychosomatics, 44, 216–222 (2003); doi: 10.1176/appi.psy.44.3.216.
K. Narushima, J. T. Kosier, and R. G. Robinson, “Preventing of poststroke depression. A 12-week double-blind randomized treatment trial with 21-month follow-up,” J. Nerv. Ment. Dis., 190, 296–303 (2002); doi: 10.1097/00005053-200205000-00005.
S. Mohamed, K. Osatuke, M. Aslam, and J. Kasckow, “Escitalopram for comorbid depression and anxiety in elderly patients: A 12-week, open-label, flexible-dose, pilot trial,” Am. J. Geriatr. Pharmacother., 4, No. 3, 201–209 (2006); doi: 10.1016/j.amjopharm.2006.08.001.
S. Kasper, O. M. Lemming, and H. de Swart, “Escitalopram in the long-term treatment of major depressive disorder in elderly patients,” Neuropsychobiology, 54, 152–159 (2006); doi: 10.1159/000098650.
E. Savaskan, S. E. Müller, A. Böhringer, et al., “Antidepressive therapy with escitalopram improves mood, cognitive symptoms, and identity memory for angry faces in elderly depressed patients,” Int. J. Neuropsychopharmacol., 11, No. 3, 381–288 (2008), doi: 10.1017/s1461145707007997.
H.-J. Möller, J. Schnitker, and W. Flürenbrock, “Factors associated with response in depressed elderly outpatients treated with escitalopram in a naturalistic setting in Germany,” Pharmacopsychiatry, 43, 210–215 (2010); doi: 10.1055/s-0030-1254152.
R. C. Petersen and J. C. Morris, “Clinical features,” in: Mild Cognitive Impairment: Aging to Alzheimer’s Disease, Oxford University Press, New York (2003), pp. 15–40; doi: 10.1056/nejm 200310023491425.
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Zhurnal Nevrologii i Psikhiatrii imeni S. S. Korsakova, Vol. 115, No. 8, Iss. 1, pp. 53–60, August, 2015.
Rights and permissions
About this article
Cite this article
Zhitkova, Y.V. Comparison of Different Doses of Escitalopram in the Prophylaxis of Dementia in Patients with Depression and Moderate Cognitive Dysfunction in Chronic Cerebral Ischemia. Neurosci Behav Physi 47, 296–302 (2017). https://doi.org/10.1007/s11055-017-0396-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11055-017-0396-0