Abstract
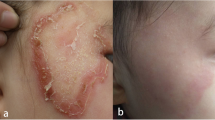
Tinea nigra is a superficial fungal infection usually caused by Hortaea werneckii (H. werneckii). We report a special case of tinea nigra in an immunocompetent child who developed a unilateral, rapidly growing pigmented lesion on her palm. Interestingly, Curvularia lunata (C. lunata) was isolated from the lesion scrapes and was identified by both morphological features and molecular biology methods. The lesion was completely cleared by topical naftifine hydrochloride and ketoconazole cream. We present—to the best of our knowledge—the first case of tinea nigra where the causative pathogen was identified as C. lunata. We therefore provide a brief literature review of previously reported cases of tinea nigra to broaden the knowledge of the potential causative pathogens. The etiology, demography, clinical features, diagnostic methods, and treatment of the reviewed cases are summarized and analyzed.


Similar content being viewed by others
References
Piliouras P, et al. Dermoscopy improves diagnosis of tinea nigra: a study of 50 cases. Australas J Dermatol. 2011;52(3):191–4.
McKinlay JR, Barrett TL, Ross EV. Picture of the month. Tinea nigra. Arch Pediatr Adolesc Med. 1999;153(3):305–6.
Uva L, Leal-Filipe P, Soares-de-Almeida L, Ferreira J, Oliveira A. Reflectance confocal microscopy for the diagnosis of tinea nigra. Clin Exp Dermatol. 2018;43(3):332.
Bonifaz A, et al. Tinea nigra by Hortaea werneckii, a report of 22 cases from Mexico. Stud Mycol. 2008;61:77–82.
Fader RC, McGinnis MR. Infections caused by dematiaceous fungi: chromoblastomycosis and phaeohyphomycosis. Infect Dis Clin North Am. 1988;2(4):925–38.
Perez C, et al. Tinea nigra: report of twelve cases in Venezuela. Mycopathologia. 2005;160(3):235–8.
Schwartz RA. Superficial fungal infections. Lancet. 2004;364(9440):1173–82.
Mittag H. The fine structure of Hortaea werneckii. Mycoses. 1993;36(11–12):343–50.
Abliz P, Fukushima K, Takizawa K, Miyaji M, Nishimura K. Specific oligonucleotide primers for identification of Hortaea werneckii, a causative agent of tinea nigra. Diagn Microbiol Infect Dis. 2003;46(2):89–93.
Parmelee JA. The identification of the curvularia parasite of gladiolus. Mycologia. 1956;48(4):558–67.
Tóth EJ, Monika V, Takó M, Homa M, Jáger O, Hermesz E, Orvos H, Nagy G, Vágvölgyi C, Papp T. Response of human neutrophil granulocytes to the hyphae of the emerging fungal pathogen Curvularia lunata. Pathogens. 2020;9(3):235.
Gugnani HC. Nondermatophytic filamentous keratinophilic fungi and their role in human infection. Rev Iberoam Micol 2000;109–114.
Hughes JR, Moore MK, Pembroke AC. Tinea nigra palmaris. Clin Exp Dermatol. 1993;18(5):481–2.
Severo LC, Bassanesi MC, Londero AT. Tinea nigra: report of four cases observed in Rio Grande do Sul (Brazil) and a review of Brazilian literature. Mycopathologia. 1994;126(3):157–62.
Gu H, et al. A case report of tinea palmaris caused by Hortaea werneckii. Chin J Dermatol. 1996;5:354–5.
Gupta G, Burden AD, Shankland GS, Fallowfield ME, Richardson MD. Tinea nigra secondary to Exophiala werneckii responding to itraconazole. Br J Dermatol. 1997;137(3):483–4.
Smith SB. Dermoscopy in the diagnosis of tinea nigra plantaris. Cutis. 2001;68(6):377–80.
Liu Z, et al. A case of Tinea Nigra of the chest. Chin J Lepr Skin Dis. 2001;3:201.
Muellenhoff M, Cukrowski T, Morgan M, Miller R. Enlarging pigmented patches on the hand. Int J Dermatol. 2003;42(10):810.
Pegas JR, Criado PR, Lucena SK, de Oliveira MA. Tinea nigra: report of two cases in infants. Pediatr Dermatol. 2003;20(4):315–7.
Dai X, et al. A case of Tinea Manuum Nigra. J Clin Dermatol. 2004;5:290–1.
Pi X, et al. A case of Tinea Nigra. Chin J Dermatol. 2005;8:66.
Wu Q, et al. Pediatric Tinea Nigra caused by Hortaea werneckii. Chin J Lab Med. 2005;28(4):448.
Rosen T, Ahila L. Rapid treatment of tinea nigra palmaris with ciclopirox olamine gel, 0.77%. Skinmed. 2006;5(4):201–3.
Uezato H, et al. A case of tinea nigra palmaris in Okinawa. Japan J Dermatol. 2006;33(1):23–9.
Larangeira de Almeida Jr. H, et al. Bilateral tinea nigra in a temperate climate. Dermatol Online J. 2007;13(3):25.
Maldonado I. Tinea nigra palmaris: a clinical case in Argentina. Rev Argent Microbiol. 2007;39(4):218–20.
Qu B, et al. Pediatric Tinea Nigra: case report. Chin J Dermatol. 2007;40(08):510.
Xavier MH, Ribeiro LHS, Duarte H, Saraça G, Souza AC. Dermatoscopy in the diagnosis of tinea nigra. Dermatol Online J. 2008;14(8):15.
Wang X, et al. Tinea Nigra palmaris in a child: a case report. J Clin Dermatol. 2008;11:721–2.
Tilak R, et al. A case report of tinea nigra from North India. Indian J Dermatol Venereol Leprol. 2009;75(5):538–9.
Schneider J, LaCasse A. What is your diagnosis? Tinea nigra. Cutis. 2009;84(6):299–300.
Rezusta A, Gilaberte Y, Betran A, Gene J, Querol I, Arias M, Revillo MJ. Tinea nigra: a rare imported infection. J Eur Acad Dermatol Venereol. 2010;24(1):89–91.
Paschoal FM, et al. Study of the dermatoscopic pattern of tinea nigra: report of 6 cases. Skinmed. 2010;8(6):319–21.
Rossetto AL, Cruz RC. Tinea nigra in geographical forms of “heart” and "parrot beak. An Bras Dermatol. 2011;86(2):389–90.
Helm TN, et al. What is your diagnosis? Tinea Nigra. 2011;87(5):229.
Rossetto AL, Cruz R. Spontaneous cure in a case of Tinea nigra. An Bras Dermatol. 2012;87(1):160–2.
Rossetto AL, Cruz R. Tinea nigra: successful treatment with topical butenafine. An Bras Dermatol. 2012;87(6):939–41.
Criado PR, Delgado L. Dermoscopy revealing a case of Tinea Nigra. An Bras Dermatol. 2013;88(1):128–9.
Rossetto AL, et al. Double-blind study with topical Isoconazole and Terbinafine for the treatment of one patient with bilateral Tinea nigra plantaris and suggestions for new differential diagnosis. Rev Inst Med Trop Sao Paulo. 2013;55(2):125–8.
Julián-González R, Vargas-de Julian V. Tinea nigra in an unusual anatomic location. An Pediatr Barc. 2013;79(5):340–1.
Cabrera R, Sabatini N, Urrutia M, Sepúlveda R. Tinea nigra: a allochthonous case report in Chile. Rev Chilena Infectol. 2013;30(1):90–3.
Rossetto AL, et al. Tinea nigra presenting speckled or “salt and pepper” pattern. Am J Trop Med Hyg. 2014;90(6):981.
Rossetto AL, et al. A case of Tinea nigra associated to a bite from a European rabbit (Oryctolagus cuniculus, Leporidae): the role of dermoscopy in diagnosis. An Bras Dermatol. 2014;89(1):165–6.
Guarenti IM, et al. Scanning electron microscopy of tinea nigra. An Bras Dermatol. 2014;89(2):334–6.
Sarangi G, Dash D, Chayani N, Patjoshi SK, Jena S. Bilateral Tinea Nigra of palm: a rare case report from Eastern India. Indian J Med Microbiol. 2014;32(1):86–8.
Tan H, et al. Tinea Nigra Palmaris: a case report. J Clin Dermatol. 2014;43(06):354–5.
Darrigade AS, Saint Marie D, Dufour J, Edouard S, Graille J, Cheuret M, Couppié P. The value of dermoscopy in the diagnosis of tinea nigra. Dermatol Venereol. 2014;141(2):167–9.
Falcão EM, et al. Bilateral tinea nigra plantaris with good response to isoconazole cream: a case report. Case Rep Dermatol. 2015;7(3):306–10.
Solak B, Unus Z. Tinea nigra on the fingers. BMJ Case Rep. 2015.
Noguchi H, et al. Tinea nigra showing a parallel ridge pattern on dermoscopy. J Dermatol. 2015;42(5):518–20.
MaiaAbinader MV, et al. Tinea nigra dermoscopy: a useful assessment. J Am Acad Dermatol. 2016;74(6):121.
Thomas CL, et al. Entodermoscopy: a spotlight on tinea nigra. Int J Dermatol. 2016;55(2):117.
Nazzaro G, et al. Tinea nigra: a diagnostic pitfall. J Am Acad Dermatol. 2016;75(6):e219.
Lu S, et al. A case report and a brief survey of the Tinea Nigra Cases reported in Mainland China. Chin J Mycol. 2016;11(05):279–81.
Guo Y, et al. A case report of tinea nigra palmaris caused by Hortaea werneckii. J Clin Dermatol. 2016;45(10):736–9.
Veasey JV, et al. Reflectance confocal microscopy of tinea nigra: comparing images with dermoscopy and mycological examination results. An Bras Dermatol. 2017;92(4):568–9.
Perez-Tanoira R, et al. Tinea nigra palmaris: a clinical case in a rural Ethiopian hospital. Rev Inst Med Trop Sao Paulo. 2018;60:e52.
Giordano L, et al. Tinea nigra: report of three pediatrics cases. Rev Chil Pediatr. 2018;89(4):506–10.
Xia Y, et al. Tinea Nigra Palmaris mistaken for junctional nevus- case report. Chin J Lepr Skin Dis. 2018;34(11):690–2.
Nogita A, et al. Case of tinea nigra on the sole: correspondences between dermoscopic and histological findings. J Dermatol. 2019;46(6):e187–8.
Arellano J, et al. First autochthonous case report of tinea nigra in Chile. Medwave. 2019;19(6):e7666.
Eksomtramage T, Aiempanakit K. Tinea nigra mimicking acral melanocytic nevi. IDCases. 2019;18:e00654.
Yang X, et al. A case of tinea nigra palmaris in a child caused by Hortaea werneckii. J Clin Dermatol. 2019;48(07):414–6.
Zhao X, et al. A case of tinea nigra palmaris caused by Hortaea werneckii. J Pract Dermatol. 2019;12(02):117–8.
Kupsa R, et al. Suspicious hyperpigmentation with parallel ridge pattern on acral skin: three case reports. Hautarzt. 2020;71(2):154–7.
Ibraheim MK, et al. Interdigital Tinea Nigra. Cureus. 2020;12(4):e7579.
Lima Dantas M, et al. Entodermoscopy in the diagnosis of Tinea Nigra: two case reports. Dermatol Pract Concept. 2020;10(3):e2020065.
Chamroensakchai T, et al. Tinea nigra palmaris-associated peritonitis, caused by Hortaea werneckii: the first case report in a peritoneal dialysis patient. Perit Dial Int. 2020;41(3):333–6.
Li M, et al. The first case of Tinea Nigra on wrist caused by Hortaea werneckii in Chinese mainland and literature review. Chin J Mycol. 2020;15(04):193–6.
Zhou S, et al. Two cases of children Tinea Nigra caused by Hortaea werneckii. Chin J Dermatovenereol. 2021;35(02):174–7.
Label A, Sole J, Larralde M. Tinea Nigra: dermoscopic findings. Actas Dermosifiliogr. 2021;112(6):539–40.
de Oliveira Valentim F. Tinea nigra: a series of three cases observed in Botucatu, São Paulo. Revista da Sociedade Brasileira de Medicina Tropical. 2021;54:563.
Zheng W, et al. Hortaea werneckii infection: report of 14 cases. Chin J Infect Chemother. 2021;21(5):552–6.
Patel SM, et al. Superficial Mycoses and Dermatophytes 2017;190–201. https://doi.org/10.1016/B978-0-323-29634-2.00017-1
Revankar SG, Sutton DA. Melanized fungi in human disease. Clin Microbiol Rev. 2010;23(4):884–928.
Shoff CJ, Perfect JR. Uncommon yeasts and molds causing human disease. Encyclopedia of Mycology. Elsevier. 2021:813–834.
Wilhelmus KR, Jones DB. Curvularia keratitis. Trans Am Ophthalmol Soc. 2001;99:111–30.
Kumar A, Khurana A. Bilateral Curvularia keratitis. J Ophthalmic Vis Res. 2020;15(4):574–5.
Pathengay A, et al. Curvularia lunata endophthalmitis presenting with a posterior capsular plaque. Indian J Ophthalmol. 2006;54(1):65–6.
Bartynski JM, McCaffrey TV, Frigas E. Allergic fungal sinusitis secondary to dermatiaceous fungi–Curvularia lunata and Alternaria. Otolaryngol Head Neck Surg. 1990;103(1):32–9.
Kamalam A, et al. Paronychia and black discoloration of a thumb nail caused by Curvularia lunata. Mycopathologia. 1992;118(2):83–4.
Garg A, et al. Eumycetoma due to Curvularia lunata. Indian J Dermatol Venereol Leprol. 2008;74(5):515–6.
Bryan CS, et al. Curvularia lunata endocarditis treated with terbinafine: case report. Clin Infect Dis. 1993;16(1):30–2.
Yau YC, et al. Fungal sternal wound infection due to Curvularia lunata in a neonate with congenital heart disease: case report and review. Clin Infect Dis. 1994;19(4):735–40.
McAleer R, et al. Allergic bronchopulmonary disease caused by Curvularia lunata and Drechslera hawaiiensis. Thorax. 1981;36(5):338–44.
Guarner J, et al. Fungal peritonitis caused by Curvularia lunata in a patient undergoing peritoneal dialysis. Am J Med Sci. 1989;298(5):320–3.
Rohwedder JJ, et al. Disseminated Curvularia lunata infection in a football player. Arch Intern Med. 1979;139(8):940–1.
Tessari G, et al. Lethal systemic dissemination from a cutaneous infection due to Curvularia lunata in a heart transplant recipient. J Eur Acad Dermatol Venereol. 2003;17(4):440–2.
Vineetha M, et al. Cutaneous phaeohyphomycosis of foot web by Curvularia lunata. Glob J Med Clin Case Rep. 2017;4:070–5.
Mary V, et al. Verrucous onychomycosis caused by curvularia in a patient with congenital pterygium. Indian J Dermatol. 2016;61(6):701.
Vásquez-del-Mercado E, et al. Subcutaneous phaeohyphomycosis due to Curvularia lunata in a renal transplant patient. Rev Iberoam Micol. 2013;30(2):116–8.
Carter E, Boudreaux C. Fatal cerebral phaeohyphomycosis due to Curvularia lunata in an immunocompetent patient. J Clin Microbiol. 2004;42(11):5419–23.
Safdar A. Curvularia–favorable response to oral itraconazole therapy in two patients with locally invasive phaeohyphomycosis. Clin Microbiol Infect. 2003;9(12):1219–23.
Anbu P, et al. Secretion of keratinolytic enzymes and keratinolysis by Scopulariopsis brevicaulis and Trichophyton mentagrophytes: regression analysis. Can J Microbiol. 2006;52(11):1060–9.
Acknowledgements
This case was supported by grants from the Natural Science Foundation of Guangxi Province of China (2020GXNSFGA238001), and The First Affiliated Hospital of Guangxi Medical University Provincial and Ministerial Key Laboratory Cultivation Project: Guangxi Key Laboratory of Tropical Fungi and Mycosis Research (No. YYZS2020006).
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Handling Editor: Ping Zhan.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Odaini, N., Wei, Jy., Zheng, Yq. et al. A Special Tinea Nigra Caused by Curvularia lunata: Case Report and Literature Review. Mycopathologia 187, 291–298 (2022). https://doi.org/10.1007/s11046-022-00619-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00619-8