Abstract
Objective
This research study was undertaken to investigate antimicrobial resistance patterns and the prevalence of hospital-acquired infections (HAIs). The study focuses on common microorganisms responsible for HAIs and explores emerging challenges posed by antimicrobial drug-resistant isolates.
Methods
A comprehensive analysis of 123 patients with HAIs, hospitalized in surgical department and intensive care unit (ICU) at Imam Khomeini Hospital, Ilam, Iran, was conducted over a six-month period. Pathogenic bacterial isolates, including methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Staphylococcus aureus (VRSA), were isolated and subjected to antibiotic susceptibility testing.
Results
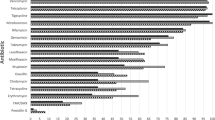
The study findings revealed a significant prevalence of multidrug-resistant (MDR) isolates, of which 73.3% were MRSA. Notably, 6.7% of S. aureus isolates exhibited resistance to vancomycin, indicating the emergence of VRSA. Respiratory infections were identified as the most prevalent HAI, constituting 34.67% of cases, often arising from extended ICU stays and invasive surgical procedures. Furthermore, patients aged 60 and above, particularly those associated with MDR, exhibited higher vulnerability to HAI.
Conclusions
This research sheds light on the intricate interplay between drug resistance and HAI, highlighting the imperative role of rational antibiotic use and infection control in addressing this critical healthcare challenge.

Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Yang XGR, Zhang B, Xie B, Zhou S, Zhang B, Lai Q (2023) Retrospective analysis of drug resistance characteristics and infection related risk factors of multidrug-resistant organisms (MDROs) isolated from the orthopedics department of a tertiary hospital. Sci Rep 13(1):2199
Horn SR, Liu TC, Horowitz JA, Oh C, Bortz CA, Segreto FA et al (2018) Clinical impact and economic burden of hospital-acquired conditions following common surgical procedures. Spine 43(22):E1358–E63
Weigelt JA, Lipsky BA, Tabak YP, Derby KG, Kim M, Gupta V (2010) Surgical site infections: causative pathogens and associated outcomes. Am J Infect Control 38(2):112–120
Yang K, Han Q, Chen B, Zheng Y, Zhang K, Li Q et al (2018) Antimicrobial hydrogels: promising materials for medical application. Int J Nanomed. :2217–2263
Medina E, Pieper DH (2016) Tackling threats and future problems of multidrug-resistant bacteria. How to overcome the antibiotic crisis: facts, challenges, technologies and future perspectives. :3–33
Yang X, Guo R, Zhang B, Xie B, Zhou S, Zhang B et al (2023) Retrospective analysis of drug resistance characteristics and infection related risk factors of multidrug-resistant organisms (MDROs) isolated from the orthopedics department of a tertiary hospital. Sci Rep 13(1):2199
Poorabbas B, Mardaneh J, Rezaei Z, Kalani M, Pouladfar G, Alami MH et al (2015) Nosocomial infections: Multicenter surveillance of antimicrobial resistance profile of Staphylococcus aureus and Gram negative rods isolated from blood and other sterile body fluids in Iran. Iran J Microbiol 7(3):127
Cong Y, Yang S, Rao X (2020) Vancomycin resistant Staphylococcus aureus infections: a review of case updating and clinical features. J Adv Res 21:169–176
Khoshnood S, Shahi F, Jomehzadeh N, Montazeri EA, Saki M, Mortazavi SM et al (2019) Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among methicillin-resistant Staphylococcus aureus strains isolated from burn patients. Acta Microbiol Immunol Hung 66(3):387–398
Hassanzadeh P, Hassanzadeh Y, Mardaneh J, Rezai E, Motamedifar M (2015) Isolation of methicillin-resistant Staphylococcus aureus (MRSA) from HIV patients referring to HIV referral center, Shiraz, Iran, 2011–2012. Iran J Med Sci 40(6):526
Shakya J (2019) Antibiogram of Biofilm Producing and Non-Producing Community Acquired-Methicillin Resistant Staphylococcus aureus Isolated from Potential Risk Population of Dharan, Nepal
Askarian M, Mahmoudi H, Assadian O (2013) Incidence of nosocomial infections in a big university affiliated hospital in Shiraz, Iran: a six-month experience. Int J Prev Med 4(3):366
Mosadeghrad A, Afshari M, Isfahani P (2021) Prevalence of nosocomial infection in Iranian hospitals: a systematic review and Meta- analysis. Iran J Epidemiol 16(4):352–362
Lewis KL, Thompson JM (2009) Health care professionals’ perceptions and knowledge of infection control practices in a community hospital. Health Care Manag 28(3):230–238
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Forbes BA, Sahm DF, Weissfeld AS (2007) Diagnostic microbiology: Mosby St Louis
McPherson RA, Pincus MR (2021) Henry’s clinical diagnosis and management by laboratory methods E-book. Elsevier Health Sciences
Standard C (2020) M100 Performance standards for Antimicrobial susceptibility testing. Clinical and Laboratory Standards Institute (CLSI). Wayne, PA, USA
Queipo-Ortuño MI, De Dios Colmenero J, Macias M, Bravo MJ, Morata P (2008) Preparation of bacterial DNA template by boiling and effect of immunoglobulin G as an inhibitor in real-time PCR for serum samples from patients with brucellosis. Clin Vaccine Immunol 15(2):293–296
Ghanbari F, Nourmoradi H, Nazari A, Sadeghifard N, Pakzad I, Soroush S et al (2023) Molecular epidemiology and recycling of Staphylococcus aureus resistant to methicillin among the staff, patients, and surfaces in university hospital in West Iran, Ilam. Infectious disorders-drug targets (formerly current drug targets-infectious disorders). 23(1):42–51
Goudarzi G, Hasanvand Y, Rezaei F, Delfani S (2021) A comparative characterization of nasal and clinical isolates of Staphylococcus aureus from West of Iran. Iran J Microbiol 13(6):817
Tiwari HK, Sen MR (2006) Emergence of Vancomycin resistant Staphylococcus aureus (VRSA) from a tertiary care hospital from northern part of India. BMC Infect Dis 6:1–6
Golli A-L, Cristea OM, Zlatian O, Glodeanu A-D, Balasoiu AT, Ionescu M et al (2022) Prevalence of multidrug-resistant pathogens causing bloodstream infections in an intensive care unit. Infect Drug Resist. :5981–5992
Vickers ML, Ballard EL, Harris PN, Knibbs LD, Jaiprakash A, Dulhunty JM et al (2020) Bacterial profile, multi-drug resistance and seasonality following lower limb orthopaedic surgery in tropical and subtropical Australian hospitals: an epidemiological cohort study. Int J Environ Res Public Health 17(2):657
Bubonja-Sonje M, Matovina M, Skrobonja I, Bedenic B, Abram M (2015) Mechanisms of carbapenem resistance in multidrug-resistant clinical isolates of Pseudomonas aeruginosa from a Croatian hospital. Microb Drug Resist 21(3):261–269
Wang M, Wei H, Zhao Y, Shang L, Di L, Lyu C et al (2019) Analysis of multidrug-resistant bacteria in 3223 patients with hospital-acquired infections (HAI) from a tertiary general hospital in China. Bosnian J Basic Med Sci 19(1):86
Ruscher C, Pfeifer Y, Layer F, Schaumann R, Levin K, Mielke M (2014) Inguinal skin colonization with multidrug-resistant bacteria among residents of elderly care facilities: frequency, persistence, molecular analysis and clinical impact. Int J Med Microbiol 304(8):1123–1134
Zhou Y, Yu F, Yu Y, Zhang Y, Jiang Y (2021) Clinical significance of MDRO screening and infection risk factor analysis in the ICU. Am J Translational Res 13(4):3717
Eliopoulos GM, Cosgrove SE, Carmeli Y (2003) The impact of antimicrobial resistance on health and economic outcomes. Clin Infect Dis 36(11):1433–1437
Mazzariol A, Bazaj A, Cornaglia G (2017) Multi-drug-resistant gram-negative bacteria causing urinary tract infections: a review. J Chemother 29(sup1):2–9
Deemer K, Grey J, Fronczek C, Marr K (2020) Impact of reflex fosfomycin susceptibility testing on the utilization of carbapenems for definitive extended-spectrum β-lactamase Escherichia coli urinary tract infection treatment. Am J Health-System Pharm 77(Supplement4):S105–S10
Schilero GJ, Spungen AM, Bauman WA, Radulovic M, Lesser M (2009) Pulmonary function and spinal cord injury. Respir Physiol Neurobiol 166(3):129–141
Park SH (2014) Third-generation cephalosporin resistance in gram-negative bacteria in the community: a growing public health concern. Korean J Intern Med 29(1):27
Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME (2012) Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum β-lactamases: a systematic review and meta-analysis. J Antimicrob Chemother 67(12):2793–2803
Park SH, Choi S-M, Lee D-G, Kim J, Choi J-H, Kim S-H et al (2011) Emergence of extended-spectrum β-lactamase-producing Escherichia coli as a cause of community-onset bacteremia in South Korea: risk factors and clinical outcomes. Microb Drug Resist 17(4):537–544
Kang C-I, Song J-H, Chung DR, Peck KR, Ko KS, Yeom J-S et al (2010) Risk factors and treatment outcomes of community-onset bacteraemia caused by extended-spectrum β-lactamase-producing Escherichia coli. Int J Antimicrob Agents 36(3):284–287
Lee S, Han SW, Kim KW, Kwon KT (2014) Third-generation cephalosporin resistance of community-onset Escherichia coli and Klebsiella pneumoniae bacteremia in a secondary hospital. Korean J Intern Med 29(1):49
Garoy EY, Gebreab YB, Achila OO, Tekeste DG, Kesete R, Ghirmay R et al (2019) Methicillin-resistant Staphylococcus aureus (MRSA): prevalence and antimicrobial sensitivity pattern among patients—a multicenter study in Asmara, Eritrea. Canadian Journal of Infectious Diseases and Medical Microbiology. 2019
Yang X, Guo R, Xie B, Lai Q, Xu J, Hu N et al (2021) Drug resistance of pathogens causing nosocomial infection in orthopedics from 2012 to 2017: a 6-year retrospective study. J Orthop Surg Res 16:1–8
Sepandi M, Motahari F, Taheriyan M, Hashemi S (2021) Evaluation of the prevalence of nosocomial infections and their Antibiotic Resistance in one of the military hospitals affiliated Army Medical University during 2018–2019
Kaleem F, Usman J, Sattar A, Amanat ST, Hassan A, Omair M et al (2012) Current status of Vancomycin susceptibility against methicillin resistant Staphylococcus aureus (MRSA) strains: a study at two tertiary care hospitals of Pakistan. Afr J Microbiol Res 6(33):6243–6246
Saadat S, Solhjoo K, Norooz-Nejad M-J, Kazemi A (2014) VanA and vanB positive Vancomycin-resistant Staphylococcus aureus among clinical isolates in Shiraz, South of Iran. Oman Med J 29(5):335
Selim S, Faried OA, Almuhayawi MS, Saleh FM, Sharaf M, El Nahhas N et al (2022) Incidence of Vancomycin-resistant Staphylococcus aureus strains among patients with urinary tract infections. Antibiotics 11(3):408
Gohar NM, Balah MM, Sahloul N (2023) Detection of Vancomycin Resistance among Hospital and Community-acquired Methicillin-resistant Staphylococcus aureus isolates. Egypt J Med Microbiol 32(4):45–52
Yetmar ZA, Razi S, Nayfeh T, Gerberi DJ, Mahmood M, Saleh OMA (2022) Ceftriaxone versus antistaphylococcal antibiotics for definitive treatment of methicillin-susceptible Staphylococcus aureus infections: a systematic review and meta-analysis. Int J Antimicrob Agents 59(1):106486
Chen H-Y, Huang T-Y, Chen J-L, Kuo L-T, Huang K-C, Tsai Y-H (2022) Rational use of ceftriaxone in necrotizing fasciitis and mortality associated with bloodstream infection and hemorrhagic bullous lesions. Antibiotics 11(11):1454
Kourtis AP, Hatfield K, Baggs J, Mu Y, See I, Epson E et al (2019) Vital signs: epidemiology and recent trends in methicillin-resistant and in methicillin-susceptible Staphylococcus aureus bloodstream infections—United States. Morb Mortal Wkly Rep 68(9):214
Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Tleyjeh IM, Rybak MJ et al (2015) Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 132(15):1435–1486
Shariati A, Arshadi M, Khosrojerdi MA, Abedinzadeh M, Ganjalishahi M, Maleki A et al (2022) The resistance mechanisms of bacteria against ciprofloxacin and new approaches for enhancing the efficacy of this antibiotic. Front Public Health 10:1025633
System N (2003) National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1992 through June 2003, issued August 2003. Am J Infect Control 31(8):481–498
Ghanbari F, Ghajavand H, Behshod P, Ghanbari N, Khademi F (2018) Prevalence of hospital-acquired infections in hospitalized patients in different wards of Shariati Hospital of Isfahan, 2014. J Health 8(5):511–517
Koch AM, Nilsen RM, Eriksen HM, Cox RJ, Harthug S (2015) Mortality related to hospital-associated infections in a tertiary hospital; repeated cross-sectional studies between 2004–2011. Antimicrob Resist Infect Control 4(1):1–8
Funding
The authors received no funding for this work.
Author information
Authors and Affiliations
Contributions
Nourkhoda Sadeghifard contributed to the study conception and design. Data collection and analysis were performed by Somayeh Karamolahi, Saeed Khoshnood, Vahab Hassan Kaviar, Marzieh Hashemian, and Jalil Feizi. The first draft of the manuscript was written by Somayeh Karamolahi and Saeed Khoshnood, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflict of interest in this study.
Ethical approval
The study protocol was approved by the local ethics committee of Ilam University of Medical Sciences Iran. Written informed consent was received from each patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karamolahi, S., Kaviar, V.H., Haddadi, M.H. et al. Molecular characterization of Staphylococcus aureus isolated from hospital-acquired infections in Ilam, Iran. Mol Biol Rep 51, 686 (2024). https://doi.org/10.1007/s11033-024-09580-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09580-9