Abstract
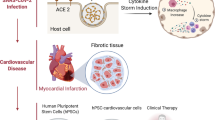
Modeling severe acute respiratory syndrome, Coronavirus 2 (SARS-CoV-2) infection in stem cell-derived organoids has helped in our understanding of the molecular pathogenesis of COVID-19 disease due to their resemblance to actual human tissues or organs. Over the past decade, organoid 3-dimensional (3D) cultures have represented a new perspective and considerable advancement over traditional in vitro 2-dimensional (2D) cell cultures. COVID-19 disease causes lung injury and multi-organ failure leading to death, especially in older patients. There is an urgent need for physiological models to study SARS-CoV-2 infection during the pandemic. Human stem cell-derived organoids can provide insight into understanding the SARS-CoV-2 cell entry molecular mechanism. Identifying such complexities will help to develop the best preventive drug targets.


Similar content being viewed by others
Data Availability
This Declaration is not applicable.
Abbreviations
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus SARS 2
- ISGs:
-
Interferon-gamma stimulated genes
- iPSCs:
-
induced Pluripotent Stem Cells
- ASCs:
-
Adult Stem Cells
- ESCs:
-
Embryonic Stem Cells
- hPSCs:
-
human Pluripotent Stem Cells
- ACE2:
-
Angiotensin-Converting Enzyme 2
- TMPRSS2:
-
Transmembrane serine proteinase 2
- AT2:
-
Alveolar type II
- MPA:
-
Mycophenolic Acid
- hBO:
-
human Bronchial Organoids
- hBEpC:
-
human Bronchial Epithelial Cells
- hrsACE2:
-
human recombinant soluble ACE2
- LTL:
-
Lotus Tetraglobus Lectin
- hSIOs:
-
human Small Intestine Organoids
- ChP:
-
Choroid Plexus
- CORGs:
-
Cerebral Organoids
- NPCs:
-
Neural Progenitor Cells
- RBD:
-
Receptor-Binding Domain
- PPC:
-
Proprotein Convertase motif
- EMMPRIN:
-
Extracellular Matrix Metalloproteinase Inducer
- CatB/L:
-
proteases Cathepsin B and L
References
Drosten C, Günther S, Preiser W et al (2003) Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. https://doi.org/10.1056/NEJMoa030747
Hemida MG, Perera RA, Wang P et al (2013) Middle east respiratory syndrome (MERS) coronavirus seroprevalence in domestic livestock in Saudi Arabia, 2010 to 2013. https://doi.org/10.2807/1560-7917.ES2013.18.50.20659. Eurosurveillance
Guan W, Ni Z, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. https://doi.org/10.1056/NEJMoa2002032
Monteil V, Kwon H, Prado P et al (2020) Inhibition of SARS-CoV-2 infections in Engineered Human Tissues using Clinical-Grade Soluble Human ACE2. https://doi.org/10.1016/j.cell.2020.04.004. Cell
Yu F, Jia R, Tang Y et al (2020) SARS-CoV-2 infection and stem cells: Interaction and intervention. Stem Cell Res
Chrzanowski W, Kim SY, McClements L (2020) Can stem cells beat COVID-19: advancing stem cells and extracellular vesicles toward Mainstream Medicine for Lung Injuries Associated with SARS-CoV-2 infections. https://doi.org/10.3389/fbioe.2020.00554. Front Bioeng Biotechnol
Wu X, Loan V, Thi D et al (2018) Intrinsic Immunity Shapes Viral Resistance of Stem Cells Article Intrinsic Immunity Shapes Viral Resistance of Stem Cells. Cell
Antonucci J, Gehrke L (2019) Cerebral organoid models for neurotropic viruses. ACS Infect. Dis
Lehmann R, Lee CM, Shugart EC et al (2019) Human organoids: a new dimension in cell biology. Mol Biol Cell. https://doi.org/10.1091/mbc.E19-03-0135
Han Y, Yang L, Duan X et al (2020) Identification of candidate COVID-19 therapeutics using hPSC-derived lung organoids. https://doi.org/10.1101/2020.05.05.079095. bioRxiv
Suzuki T, Ito Y, Sakai Y et al (2020) Generation of human bronchial organoids for SARS-CoV-2 research. https://doi.org/10.1101/2020.05.25.115600. bioRxiv
Zhao B, Ni C, Gao R et al (2020) Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids. Protein Cell
Yang L, Han Y, Nilsson-Payant BE et al (2020) A human pluripotent stem cell-based platform to Study SARS-CoV-2 tropism and model virus infection in human cells and organoids. https://doi.org/10.1016/j.stem.2020.06.015. Cell Stem Cell
Lamers MM, Beumer J, van der Vaart J et al (2020) SARS-CoV-2 productively infects human gut enterocytes. Science. https://doi.org/10.1126/science.abc1669
Zhou J, Li C, Liu X et al (2020) Infection of bat and human intestinal organoids by SARS-CoV-2. Nat Med. https://doi.org/10.1038/s41591-020-0912-6
McMahon CL, Staples H, Gazi M et al (2021) SARS-CoV-2 targets glial cells in human cortical organoids. Stem Cell Reports. https://doi.org/10.1016/j.stemcr.2021.01.016
Jacob F, Pather SR, Huang WK et al (2020) Human pluripotent stem cell-derived neural cells and Brain Organoids reveal SARS-CoV-2 Neurotropism predominates in Choroid Plexus Epithelium. https://doi.org/10.1016/j.stem.2020.09.016. Cell Stem Cell
Tiwari SK, Wang S, Smith D et al (2021) Revealing tissue-specific SARS-CoV-2 infection and host responses using human stem cell-derived lung and cerebral organoids. https://doi.org/10.1016/j.stemcr.2021.02.005. Stem Cell Reports
Lai HIAM, Chou SJ, Chien Y et al (2021) Expression of endogenous angiotensin-converting enzyme 2 in human induced pluripotent stem cell-derived retinal organoids. Int J Mol Sci. https://doi.org/10.3390/ijms22031320
Luo Y, Zhang M, Chen Y et al (2021) Application of Human Induced Pluripotent Stem Cell-Derived Cellular and Organoid Models for COVID-19 Research. Front. Cell Dev. Biol
Tran BM, Deliyannis G, Hachani A et al (2022) Organoid Models of SARS-CoV-2 infection: what have we learned about COVID-19? Organoids. https://doi.org/10.3390/organoids1010002
Han Y, Yang L, Lacko LA, Chen S (2022) Human organoid models to study SARS-CoV-2 infection. Nat Methods 418–428. https://doi.org/10.1038/s41592-022-01453-y
Chen D, Su X, Chen H et al (2022) Human organoids as a Promising platform for fighting COVID-19. Int. J. Biol. Sci.
Kim J, Koo BK, Clevers H (2022) Organoid Studies in COVID-19 Research. Int J Stem Cells 15:3–13. https://doi.org/10.15283/ijsc21251
Pei S, Chia S, Li S et al (2022) 3D human organoids: the next viral model for the molecular basis of Infectious Diseases. https://doi.org/10.3390/biomedicines10071541
Boroojerdi MH, Al Jabry T, Mirarefin SMJ, Albalushi H (2023) Insights into organoid-based modeling of COVID-19 pathology. Virol J 20:1–13. https://doi.org/10.1186/s12985-023-01996-2
Young BE, Ong SWX, Kalimuddin S et al (2020) Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA - J Am Med Assoc. https://doi.org/10.1001/jama.2020.3204
Fang KY, Cao WC, Xie TA et al (2021) Exploration and validation of related hub gene expression during SARS-CoV-2 infection of human bronchial organoids. Hum Genomics. https://doi.org/10.1186/s40246-021-00316-5
Wang W, Xu Y, Gao R et al (2020) Detection of SARS-CoV-2 in different types of clinical specimens. JAMA - J. Am. Med. Assoc
Ling Y, Xu SB, Lin YX et al (2020) Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl). https://doi.org/10.1097/CM9.0000000000000774
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. https://doi.org/10.1016/S0140-6736(20)30183-5
Xiao F, Tang M, Zheng X et al (2020) Evidence for gastrointestinal infection of SARS-CoV-2. https://doi.org/10.1053/j.gastro.2020.02.055. Gastroenterology
Pellegrini L, Albecka A, Mallery DL et al (2020) SARS-CoV-2 infects the Brain Choroid Plexus and disrupts the Blood-CSF barrier in human brain organoids. Cell Stem Cell. https://doi.org/10.1016/j.stem.2020.10.001
Apicella M, Campopiano MC, Mantuano M et al (2020) COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. https://doi.org/10.1016/s2213-8587(20)30238-2
Bansal M (2020) Cardiovascular disease and COVID-19. Diabetes Metab Syndr Clin Res Rev. https://doi.org/10.1016/j.dsx.2020.03.013
Mills RJ, Humphrey SJ, Fortuna PRJ et al (2021) BET inhibition blocks inflammation-induced cardiac dysfunction and SARS-CoV-2 infection. Cell. https://doi.org/10.1016/j.cell.2021.03.026
Lindner D, Fitzek A, Bräuninger H et al (2020) Association of Cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.3551
Eriksen AZ, Møller R, Makovoz B et al (2021) SARS-CoV-2 infects human adult donor eyes and hESC-derived ocular epithelium. Cell Stem Cell. https://doi.org/10.1016/j.stem.2021.04.028
Mahmoud IS, Jarrar YB, Alshaer W, Ismail S (2020) SARS-CoV-2 entry in host cells-multiple targets for treatment and prevention. Biochimie
Shang J, Wan Y, Luo C et al (2020) Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.2003138117
Grabovenko F, Nikiforova L, Yanenko B et al (2022) Glycosylation of receptor binding domain of SARS-CoV-2 S-Protein influences on binding to immobilized DNA aptamers. Int J Mol Sci 23. https://doi.org/10.3390/ijms23010557
Zhao X, Chen H, Wang H (2021) Glycans of SARS-CoV-2 spike protein in Virus infection and antibody production. Front. Mol. Biosci
Watanabe Y, Allen JD, Wrapp D et al (2020) Site-specific glycan analysis of the SARS-CoV-2 spike. Sci (80)369. https://doi.org/10.1126/science.abb9983
Basu A, Sarkar A, Maulik U (2020) Molecular docking study of potential phytochemicals and their effects on the complex of SARS-CoV2 spike protein and human ACE2. Sci Rep 10. https://doi.org/10.1038/s41598-020-74715-4
Ghosh N, Nandi S, Saha I (2022) A review on evolution of emerging SARS-CoV-2 variants based on spike glycoprotein. Int Immunopharmacol 105
Casalino L, Gaieb Z, Goldsmith JA et al (2020) Beyond shielding: the roles of glycans in the SARS-CoV-2 spike protein. ACS Cent Sci 6. https://doi.org/10.1021/acscentsci.0c01056
Zhao P, Praissman JL, Grant OC et al (2020) Virus-receptor interactions of glycosylated SARS-CoV-2 spike and human ACE2 receptor. Cell Host Microbe 28. https://doi.org/10.1016/j.chom.2020.08.004
Thépaut M, Luczkowiak J, Vivès C et al (2021) DC/L-SIGN recognition of spike glycoprotein promotes SARS-CoV-2 trans-infection and can be inhibited by a glycomimetic antagonist. PLoS Pathog 17. https://doi.org/10.1371/journal.ppat.1009576
Guo L, Liang Y, Li H et al (2021) Epigenetic glycosylation of SARS-CoV-2 impact viral infection through DC&L-SIGN receptors. https://doi.org/10.1016/j.isci.2021.103426. iScience 24:
Casas-Sanchez A, Romero-Ramirez A, Hargreaves E et al (2022) Inhibition of protein N-Glycosylation blocks SARS-CoV-2 infection. https://doi.org/10.1128/MBIO.03718-21. MBio
Pizzato M, Baraldi C, Boscato Sopetto G et al (2022) SARS-CoV-2 and the host cell: a tale of interactions. Front Virol. https://doi.org/10.3389/fviro.2021.815388
Kadam SB, Sukhramani GS, Bishnoi P et al (2021) SARS-CoV-2, the pandemic coronavirus: Molecular and structural insights. J Basic Microbiol 61
Liu XH, Cheng T, Liu BY et al (2022) Structures of the SARS-CoV-2 spike glycoprotein and applications for novel drug development. Front Pharmacol 13:1–21. https://doi.org/10.3389/fphar.2022.955648
Costa LB, Perez LG, Palmeira VA et al (2020) Insights on SARS-CoV-2 molecular interactions with the renin-angiotensin system. Front. Cell Dev. Biol
Hoffmann M, Kleine-Weber H, Schroeder S et al (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. https://doi.org/10.1016/j.cell.2020.02.052. Cell
Johnson BA, Xie X, Bailey AL et al (2021) Loss of furin cleavage site attenuates SARS-CoV-2 pathogenesis. Nature. https://doi.org/10.1038/s41586-021-03237-4
Jackson CB, Farzan M, Chen B, Choe H (2022) Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol.
Wang K, Chen W, Zhang Z et al (2020) CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells. Signal Transduct Target Ther. https://doi.org/10.1038/s41392-020-00426-x
Warschkau D, Delgado-Betancourt E, Holthaus D et al (2022) From 3D to 2D: harmonization of protocols for two-dimensional cultures on cell culture inserts of intestinal organoids from various species. https://doi.org/10.21769/BioProtoc.4295. Bio-protocol
Roodsant T, Navis M, Aknouch I et al (2020) A human 2D primary organoid-derived epithelial monolayer model to study Host-Pathogen Interaction in the small intestine. https://doi.org/10.3389/fcimb.2020.00272. Front Cell Infect Microbiol
Acknowledgements
We thank Dr. David Vocadlo for his support. L.D.N appreciates Dr. Josef Penninger and Dr. Lisa Julian for their comments and guidance. L.D.N is grateful to PE. Aryan for her encouragement.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
The main draft of the manuscript was designed and written by L.D.N and all authors commented on previous versions of the manuscript. L.D.N prepared the figures and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This Declaration is not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dawoody Nejad, L., Julian, L.M. Stem cell-derived organoid models for SARS-CoV-2 and its molecular interaction with host cells. Mol Biol Rep 50, 10627–10635 (2023). https://doi.org/10.1007/s11033-023-08785-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08785-8