Abstract
Background
An experimental study was conducted to examine whether melatonin influences osteogenic/odontogenic differentiation of human stem cells derived from the apical papilla (hSCAPs).
Materials and methods
In order to isolate hSCAPs, the undeveloped root of a third molar of a human tooth was used. Melatonin was administered to the experimental groups in an osteogenic medium. No treatment was administered to the control group. The methyl thiazolyl tetrazolium (MTT) assay was performed on days 1, 2, and 3 to assess cell viability (n = 8). A determination of odontogenic/osteogenic differentiation was accomplished using alkaline phosphatase (ALP) activity alizarin red staining (ARS) (n = 6), and the expression of osteogenic genes by real-time polymerase chain reaction (RT-PCR) (n = 3) on days 1, 2, and 7. Evaluation of the data was conducted using SPSS version 18. All experiments were conducted at least three times. The Mann Whitney U test, the ANOVA analysis, Tukey’s test, and t-test was implemented to analyze the data (α = 0.05).
Results
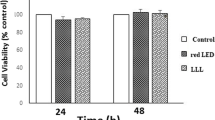
After 24 h, 48 h, and 72 h, No significant difference was observed between the control group and the melatonin treatment group in terms of viability of hSCAPs. (from 1 up to 10 µg/ml) (P > 0.05). The assessment of ARS and ALP activity showed that melatonin treatment enhanced osteogenic differentiation of hSCAPs (P < 0.001). Melatonin treatment caused hSCAPs to show an increase of genes related to osteogenic/odontogenic differentiation. These genes included ALP, dentin sialophosphoprotein (DSPP), dentin matrix protein 1 (DMP-1), and bone sialoprotein (BSP) (P < 0.001).
Conclusions
Melatonin treatment enhanced osteogenic/odontogenic differentiation of hSCAPs with a dose dependent effect on cell viability.




Similar content being viewed by others
Data Availability
The corresponding author, Elham Khoshbin, possesses the entire documentation of the study participant and other data, which can be accessed through a reasonable request.
Abbreviations
- hSCAPs:
-
Human Stem cells from the apical papilla
- MTT:
-
Methyl thiazolyl tetrazolium
- ISSCR:
-
International Society for Stem Cells Research
- qrt-PCR:
-
Quantitative reverse-transcription polymerase chain reaction
- ARS:
-
Alizarin red staining
- LLL:
-
Low level laser
- LLLI:
-
Low level laser irradiation
- LLLT:
-
Low level laser therapy
- ALP:
-
Alkaline phosphatase
- DSPP:
-
Dentin sialophosphoprotein
- DMP1:
-
Dentin matrix protein 1
- BSP:
-
Bone sialoprotein
- DPSCs:
-
Dental pulp stem cells
- hPDL:
-
Human periodontal ligament
- hPDLSCs:
-
Human periodontal ligament stem cells
- LED:
-
Light-emitting diode
- PBS:
-
Phosphate-buffered saline
- SPSS:
-
Statistical Package of the Social Sciences
- SEM:
-
Standard error of the mean
- Fig:
-
Figure
References
García-Bernal D, López-García S, Sanz JL, Guerrero-Gironés J, García-Navarro EM, Moraleda JM et al (2021) Melatonin treatment alters biological and immunomodulatory properties of human dental pulp mesenchymal stem cells via augmented transforming growth factor beta secretion. J Endod 47(3):424–435
Hu C, Li L (2019) Melatonin plays critical role in mesenchymal stem cell-based regenerative medicine in vitro and in vivo. Stem Cell Res Ther 10(1):1–11
Reiter R, Rosales-Corral S, Liu X, Acuna‐Castroviejo D, Escames G, Tan DX (2015) Melatonin in the oral cavity: physiological and pathological implications. J Periodontal Res 50(1):9–17
Gholami Farashah MS, Javadi M, Mohammadi A, Soleimani Rad J, Shakouri SK, Roshangar L (2022) Bone marrow mesenchymal stem cell’s exosomes as key nanoparticles in osteogenesis and bone regeneration: specific capacity based on cell type. Mol Biol Rep 49(12):12203–12218
Yan H, De Deus G, Kristoffersen IM, Wiig E, Reseland JE, Johnsen GF et al (2023) Regenerative endodontics by cell homing: a review of recent clinical trials. J Endod 49(1):4–17
Smeda M, Galler KM, Woelflick M, Rosendahl A, Moehle C, Lenhardt B et al (2022) Molecular biological comparison of dental pulp-and apical papilla-derived stem cells. Int J Mol Sci 23(5):2615
Sarıtekin E, Üreyen Kaya B, Aşcı H, Özmen Ö (2019) Anti-inflammatory and antiresorptive functions of melatonin on experimentally induced periapical lesions. Int Endod J 52(10):1466–1478
Zhou Y, Wang C, Si J, Wang B, Zhang D, Ding D et al (2020) Melatonin up-regulates bone marrow mesenchymal stem cells osteogenic action but suppresses their mediated osteoclastogenesis via MT2‐inactivated NF‐κB pathway. Br J Pharmacol 177(9):2106–2122
Radio NM, Doctor JS, Witt-Enderby PA (2006) Melatonin enhances alkaline phosphatase activity in differentiating human adult mesenchymal stem cells grown in osteogenic medium via MT2 melatonin receptors and the MEK/ERK (1/2) signaling cascade. J Pineal Res 40(4):332–342
de Souza Araújo IJ, Münchow EA, Tootla S, Bottino MC (2022) Dental pulp tissue regeneration. Elsevier, Tissue Engineering, pp 313–346
Goodis HE, Hargreaves KM, Tay FR (eds) (2012) Seltzer and Bender’s Dental pulp. Quintessence Pub. Batavia
Malakoti F, Zare F, Zarezadeh R, Sadigh AR, Sadeghpour A, Majidinia M, Yousefi B, Alemi F (2022) The role of melatonin in bone regeneration: a review of involved signaling pathways. Biochimie 202:56–70
Chan Y-H, Ho K-N, Lee Y-C, Chou M-J, Lew W-Z, Huang H-M et al (2022) Melatonin enhances osteogenic differentiation of dental pulp mesenchymal stem cells by regulating MAPK pathways and promotes the efficiency of bone regeneration in calvarial bone defects. Stem Cell Res Ther 13(1):73
Chen W, Chen X, Chen AC, Shi Q, Pan G, Pei M et al (2020) Melatonin restores the osteoporosis-impaired osteogenic potential of bone marrow mesenchymal stem cells by preserving SIRT1-mediated intracellular antioxidant properties. Free Radic Biol Med 146:92–106
Wang X, Chen T, Deng Z, Gao W, Liang T, Qiu X et al (2021) Melatonin promotes bone marrow mesenchymal stem cell osteogenic differentiation and prevents osteoporosis development through modulating circ_0003865 that sponges miR-3653-3p. Stem Cell Res Ther 12:1–20
Li Y, Feng C, Gao M, Jin M, Liu T, Yuan Y et al (2019) MicroRNA-92b‐5p modulates melatonin‐mediated osteogenic differentiation of bone marrow mesenchymal stem cells by targeting ICAM‐1. J Cell Mol Med 23(9):6140–6153
Zhang W, Walboomers X, Wolke J, Bian Z, Fan M, Jansen JA (2005) Differentiation ability of rat postnatal dental pulp cells in vitro. Tissue Eng 11(3–4):357–368
Huang GT-J, Shagramanova K, Chan SW (2006) Formation of odontoblast-like cells from cultured human dental pulp cells on dentin in vitro. J Endod 32(11):1066–1073
Najeeb S, Khurshid Z, Zohaib S, Zafar MS (2016) Therapeutic potential of melatonin in oral medicine and periodontology. Kaohsiung J Med Sci 32(8):391–396
Karkehabadi H, Ahmadyani E, Najafi R, Khoshbin E (2022) Effect of biodentine coated with emdogain on proliferation and differentiation of human stem cells from the apical papilla. Mol Biol Rep 49(5):3685–3692
Garrido M, Morales D, Saldías MP, Fernández C, Villalobos V, Cerda O et al (2021) Cellular response of human apical papilla cells to calcium hydroxide and tricalcium silicate-based cements. BMC Oral Health 21(1):1–8
Rahmati A, Abbasi R, Najafi R, Rezaei-Soufi L, Karkehabadi H (2022) Effect of diode low level laser and red light emitting diode irradiation on cell proliferation and osteogenic/odontogenic differentiation of stem cells from the apical papilla. BMC Oral Health 22(1):1–9
Bakopoulou A, Leyhausen G, Volk J, Tsiftsoglou A, Garefis P, Koidis P et al (2011) Comparative analysis of in vitro osteo/odontogenic differentiation potential of human dental pulp stem cells (DPSCs) and stem cells from the apical papilla (SCAP). Arch Oral Biol 56(7):709–721
Liang Y, Leng R-X, Pan H-F, Ye D-Q (2017) Associated variables of myositis in systemic lupus erythematosus: a cross-sectional study. Med Sci monitor: Int Med J experimental Clin Res 23:2543
Xu J, Wang Y, Li J, Zhang X, Geng Y, Huang Y et al (2016) IL-12p40 impairs mesenchymal stem cell-mediated bone regeneration via CD4 + T cells. Cell Death & Differentiation 23(12):1941–1951
Manaspon C, Jongwannasiri C, Chumprasert S, Sa-Ard-Iam N, Mahanonda R, Pavasant P et al (2021) Human dental pulp stem cell responses to different dental pulp capping materials. BMC Oral Health 21(1):1–13
Pereira LO, Longo JPF, Azevedo RB (2012) Laser irradiation did not increase the proliferation or the differentiation of stem cells from normal and inflamed dental pulp. Arch Oral Biol 57(8):1079–1085
Karkehabadi H, Rahmati A, Abbasi R, Farmany A, Najafi R, Behroozi R et al (2023) Effect of copper oxide nanoparticles and light-emitting diode irradiation on the cell viability and osteogenic/odontogenic differentiation of human stem cells from the apical papilla. BMC Oral Health 23(1):1–12
Calabrese EJ (2022) Hormesis and dental apical papilla stem cells. Chemico-Biol Interact 357:109887
Sonoyama W, Liu Y, Fang D, Yamaza T, Seo B-M, Zhang C et al (2006) Mesenchymal stem cell-mediated functional tooth regeneration in swine. PLoS ONE 1(1):e79
Wang LH, Gao SZ, Bai XL, Chen ZL, Yang F (2022) An up-to-date overview of dental tissue regeneration using dental origin mesenchymal stem cells: challenges and road ahead. Front Bioeng Biotechnol 10:855396
Rakhimova O, Schmidt A, Landström M, Johansson A, Kelk P, Romani Vestman N (2021) Cytokine secretion, viability, and real-time proliferation of apical-papilla stem cells upon exposure to oral Bacteria. Front Cell Infect Microbiol 10:620801
Ntege EH, Sunami H, Shimizu Y (2020) Advances in regenerative therapy: a review of the literature and future directions. Regenerative therapy 14:136–153
Law S, Chaudhuri S (2013) Mesenchymal stem cell and regenerative medicine: regeneration versus immunomodulatory challenges. Am J stem cells 2(1):22
Camacho-Alonso F, Urrutia-Rodríguez I, Onate-Cabrerizo D, Oñate-Sánchez R, Rodríguez-Lozano F (2017) Cytoprotective effects of melatonin on zoledronic acid-treated human osteoblasts. J Cranio-Maxillofacial Surg 45(8):1251–1257
Guerrero-Gironés J, Alcaina-Lorente A, Ortiz-Ruiz C, Ortiz-Ruiz E, Pecci-Lloret MP, Rodríguez-Lozano FJ et al (2020) Melatonin as an agent for direct pulp-capping treatment. Int J Environ Res Public Health 17(3):1043
Luchetti F, Canonico B, Betti M, Arcangeletti M, Pilolli F, Piroddi M et al (2010) Melatonin signaling and cell protection function. FASEB J 24(10):3603–3624
Radogna F, Nuccitelli S, Mengoni F, Ghibelli L (2009) Neuroprotection by melatonin on astrocytoma cell death. Ann N Y Acad Sci 1171(1):509–513
Cristofanon S, Uguccioni F, Cerella C, Radogna F, Dicato M, Ghibelli L et al (2009) Intracellular prooxidant activity of melatonin induces a survival pathway involving NF-κB activation. Ann N Y Acad Sci 1171(1):472–478
Martín V, Herrera F, Carrera-Gonzalez P, García-Santos G, Antolín I, Rodriguez-Blanco J et al (2006) Intracellular signaling pathways involved in the cell growth inhibition of glioma cells by melatonin. Cancer Res 66(2):1081–1088
Vaseenon S, Chattipakorn N, Chattipakorn SC (2021) Effects of melatonin in wound healing of dental pulp and periodontium: evidence from in vitro, in vivo and clinical studies. Arch Oral Biol 123:105037
Kantrong N, Jit-Armart P, Arayatrakoollikit U (2020) Melatonin antagonizes lipopolysaccharide-induced pulpal fibroblast responses. BMC Oral Health 20:1–13
Keskin Ş, Şengül F, Şirin B (2023) Evaluating the cytotoxic effect of Melatonin and Oxyresveratrol on Dental Pulp Stem cells. Eurasian J Med 55(1):32
Patil S, Alamoudi A, Zidane B, Alzahrani KJ, Alzahrani FM, Banjer HJ et al (2022) Dose-dependent Effects of Melatonin on the viability, proliferation, and differentiation of Dental Pulp Stem cells (DPSCs). J Personalized Med 12(10):1620
Dai J, Inscho EW, Yuan L, Hill SM (2002) Modulation of intracellular calcium and calmodulin by melatonin in MCF-7 human breast cancer cells. J Pineal Res 32(2):112–119
Mao L, Cheng Q, Guardiola-Lemaître B, Schuster‐Klein C, Dong C, Lai L et al (2010) In vitro and in vivo antitumor activity of melatonin receptor agonists. J Pineal Res 49(3):210–221
Alvarez-García V, González A, Alonso-González C, Martínez-Campa C, Cos S (2013) Antiangiogenic effects of melatonin in endothelial cell cultures. Microvasc Res 87:25–33
Chang HM, Liu CH, Hsu WM, Chen LY, Wang HP, Wu TH et al (2014) Proliferative effects of melatonin on S chwann cells: implication for nerve regeneration following peripheral nerve injury. J Pineal Res 56(3):322–332
Nakade O, Koyama H, Ariji H, Yajima A, Kaku T (1999) Melatonin stimulates proliferation and type I collagen synthesis in human bone cells in vitro. J Pineal Res 27(2):106–110
Satomura K, Tobiume S, Tokuyama R, Yamasaki Y, Kudoh K, Maeda E et al (2007) Melatonin at pharmacological doses enhances human osteoblastic differentiation in vitro and promotes mouse cortical bone formation in vivo. J Pineal Res 42(3):231–239
Wang B, Wen H, Smith W, Hao D, He B, Kong L (2019) Regulation effects of melatonin on bone marrow mesenchymal stem cell differentiation. J Cell Physiol 234(2):1008–1015
Zhou L, Chen X, Yan J, Li M, Liu T, Zhu C et al (2017) Melatonin at pharmacological concentrations suppresses osteoclastogenesis via the attenuation of intracellular ROS. Osteoporos Int 28:3325–3337
Sethi S, Radio NM, Kotlarczyk MP, Chen CT, Wei YH, Jockers R et al (2010) Determination of the minimal melatonin exposure required to induce osteoblast differentiation from human mesenchymal stem cells and these effects on downstream signaling pathways. J Pineal Res 49(3):222–238
Qin C, Brunn J, Cadena E, Ridall A, Tsujigiwa H, Nagatsuka H et al (2002) The expression of dentin sialophosphoprotein gene in bone. J Dent Res 81(6):392–394
Gluhak-Heinrich J, Ye L, Bonewald LF, Feng JQ, MacDougall M, Harris SE et al (2003) Mechanical loading stimulates dentin matrix protein 1 (DMP1) expression in osteocytes in vivo. J Bone Miner Res 18(5):807–817
Kang J, Chen H, Zhang F, Yan T, Fan W, Jiang L et al (2021) RORα regulates odontoblastic differentiation and mediates the pro-odontogenic effect of melatonin on dental papilla cells. Molecules 26(4):1098
Zhang F, Jiang L, He Y, Fan W, Guan X, Deng Q et al (2018) Changes of mitochondrial respiratory function during odontogenic differentiation of rat dental papilla cells. J Mol Histol 49:51–61
Son JH, Cho YC, Sung IY, Kim IR, Park BS, Kim YD (2014) Melatonin promotes osteoblast differentiation and mineralization of MC 3T3-E1 cells under hypoxic conditions through activation of PKD/p38 pathways. J Pineal Res 57(4):385–392
Han Y, Kim Y-M, Kim HS, Lee KY (2017) Melatonin promotes osteoblast differentiation by regulating Osterix protein stability and expression. Sci Rep 7(1):1–11
Zhong Z-M, Li T, Xu Z-X, Meng T-T, Zeng J-H, Zheng S et al (2013) Effect of melatonin on the proliferation and differentiation of chondrocytes from rat vertebral body growth plate in vitro. Int J Med Sci 10(10):1392–1398
Tachibana R, Tatehara S, Kumasaka S, Tokuyama R, Satomura K (2014) Effect of melatonin on human dental papilla cells. Int J Mol Sci 15(10):17304–17317
Zhang L, Zhang J, Ling Y, Chen C, Liang A, Peng Y et al (2013) Sustained release of melatonin from poly (lactic-co‐glycolic acid)(PLGA) microspheres to induce osteogenesis of human mesenchymal stem cells in vitro. J Pineal Res 54(1):24–32
Balaji TM, Varadarajan S, Jagannathan R, Mahendra J, Fageeh HI, Fageeh HN et al (2021) Melatonin as a topical/systemic formulation for the management of periodontitis: a systematic review. Materials 14(9):2417
Acknowledgements
The Vice-Chancellor of Research and Technology of the Hamadan University of Medical Sciences provided funding for this study (140111119663).
Funding
The Vice-Chancellor of Research and Technology of the Hamadan University of Medical Sciences provided funding for this study (140111119663).
Author information
Authors and Affiliations
Contributions
Hamed Karkehabadi: Conceptualization; Study selection; Data collection; Quality assessment; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing (review/ editing). Roshanak Abbasi: Conceptualization; Study selection; Data collection; Quality assessment; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing (original draft). Rezvan Najafi: Conceptualization; Study selection; Data collection; Quality assessment; Methodology; Project administration; Resources; Supervision; Validation; Visualization: Elham Khoshbin: Conceptualization; Study selection; Data collection; Quality assessment; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing (review/ editing). The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was carried out in accordance with the ISSCR Guidelines for Stem Cell Research and Clinical Translation, and received approval from the ethics committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1401.605). The study’s procedure was conducted following ethical standards established in the 1964 Helsinki Declaration and its subsequent amendments.
Informed consent
The patient who was enrolled in the trial received a thorough explanation of the procedures involved. The participant signed an informed permission form for the express aim of using the extracted teeth for study prior to the extraction at the Department of Oral and Maxillofacial Surgery, Hamadan University of Medical Sciences.
Consent for publication
Not applicable.
Competing interests
The authors have nothing significant to disclose in terms of financial or non-financial interests. The material discussed in this article is not subject to any financial or proprietary interests held by the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karkehabadi, H., Abbasi, R., Najafi, R. et al. The effects of melatonin on the viability and osteogenic/odontogenic differentiation of human stem cells from the apical papilla. Mol Biol Rep 50, 8959–8969 (2023). https://doi.org/10.1007/s11033-023-08747-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08747-0